Translate this page into:
Ventriculoperitoneal shunt catheter migration to the pulmonary artery: A rare case report

*Corresponding author: Peng Yan, Department of Interventional Vascular Surgery, Hunan Provincial People’s Hospital, Changsha City, China. ypjoinnow@hunnu.edu.cn
-
Received: ,
Accepted: ,
How to cite this article: Tan J, Li Z, Li Z, Yan P. Ventriculoperitoneal shunt catheter migration to the pulmonary artery: A rare case report. J Clin Imaging Sci. 2025;15:15. doi: 10.25259/JCIS_21_2025
Abstract
Ventriculoperitoneal (VP) shunts are commonly used to treat hydrocephalus by diverting cerebrospinal fluid from the ventricles to the peritoneal cavity. Migration of the VP shunt into the heart and pulmonary artery is a rare complication. Herein, we described a 67-year-old man with a VP shunt catheter that migrated through the venous system into the pulmonary circulation, highlighting early diagnosis with imaging and symptoms.
Keywords
Computed tomography
Migration
Pulmonary artery
Ventriculoperitoneal shunt
INTRODUCTION
Ventriculoperitoneal (VP) shunts are the standard treatment for hydrocephalus and work by redirecting cerebrospinal fluid from the ventricles to the peritoneal cavity.[1] While these devices are generally effective, they can cause a number of complications. More frequently encountered issues include infections, obstructions, and disconnections of the catheter; however, rare complications can present significant risks.[2] A rare but serious event is migration of the shunt catheter to an unintended anatomical site, such as the pulmonary artery.
The first known case of VP shunt migration into the pulmonary artery was described by Morell et al. in 1994, when the patient experienced life-threatening complications from this unusual shunt malfunction.[3] Although such cases are uncommon, they demonstrate the potential for catheter migration to atypical locations with serious consequences. Since the initial report, additional cases have emerged, underscoring the need for clinicians to recognize and promptly manage this rare complication.
In this case report, we detail the migration of a VP shunt catheter into the pulmonary circulation through the venous system. We highlight the critical role of early imaging and symptom recognition in diagnosing and managing this rare complication.
CASE REPORT
A 67-year-old male patient had fainting and head impact 4 months ago, with unconsciousness and vomiting as the main clinical symptoms. A computed tomography (CT) scan performed at a local hospital showed limited subarachnoid hemorrhage. The local hospital provided timely treatment to reduce intracranial pressure (ICP) and protect the brain and carried out follow-up rehabilitation treatment after the symptoms were relieved. However, the right limb trembled severely suddenly during rehabilitation 3 months ago. Emergency CT scan showed an enlarged subarachnoid hemorrhage. The patient was transferred to a local tertiary hospital for emergency subdural burr hole drainage to relieve intracranial hypertension. The patient was admitted to our center approximately 2 months ago with right limb dysfunction, disorganized speech and behavior, memory loss, and complete inability to care for himself. The plain CT scan of the head showed hydrocephalus and cerebral edema, and the estimated ICP by lumbar puncture was 95 cm H2O, which was severely elevated. After multidisciplinary consultation, VP shunt was selected to relieve the hydrocephalus. A repeat head and thoracic CT scan were performed 4 days after the VP shunt was established, and the radiologist reported that the VP shunt catheter was in the correct position [Figure 1]. After the VP shunt was established, the symptoms related to hydrocephalus and cerebral edema were relieved, and the shunt functioned normally.
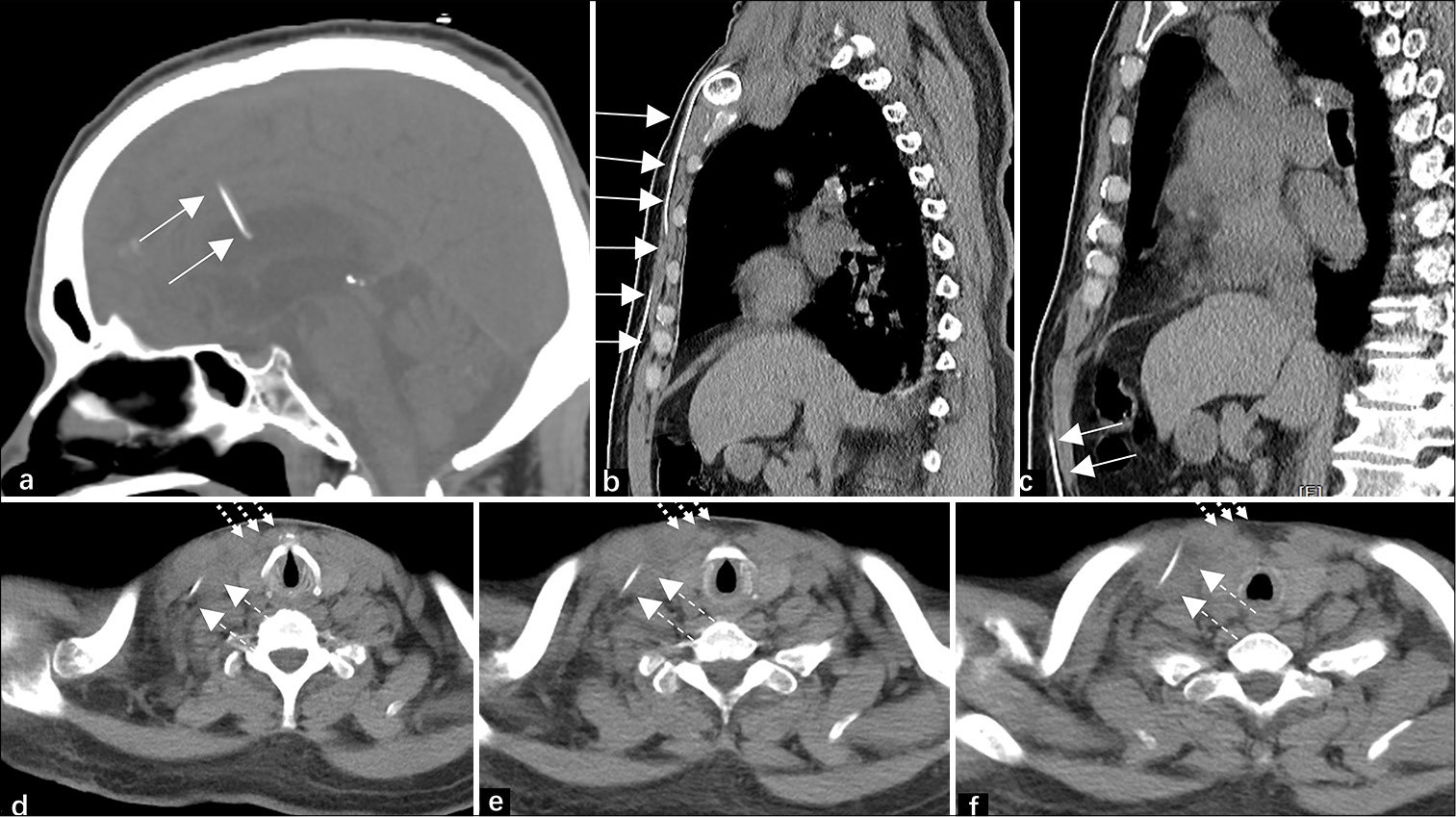
- A 67-year-old man’s head and thoracic CT scan, taken 4 days after the initial VP shunt surgery. (a-c) show the full course of the VP shunt catheter from the third ventricle to the peritoneal cavity (solid white arrow). (d-f) illustrate the catheter penetrating the right internal jugular vein, with unclear surrounding margins (dotted white arrow) and sternocleidomastoid muscle (dashed white arrow).
However, the patient’s neurological symptoms worsened 2 weeks ago, accompanied by palpitations and dyspnea, and he was admitted to the hospital again. CT of the head and chest showed migration of the VP shunt catheter to the right heart with its tip located within the main pulmonary artery [Figure 2]. To tackle this migration, the scalp was incised through the original right postauricular incision to capture the displaced VP shunt catheter and it was removed under ultrasound guidance without node and adhere. Subsequently, a new VP shunt catheter was placed through the right subcutaneous tunnel, and ventral cerebrospinal fluid (CSF) drainage was effective. Postoperative CT showed that the VP shunt catheter was placed normally [Figure 3]. Symptoms related to cerebral edema were relieved after surgery, and the patient was discharged without other complications.
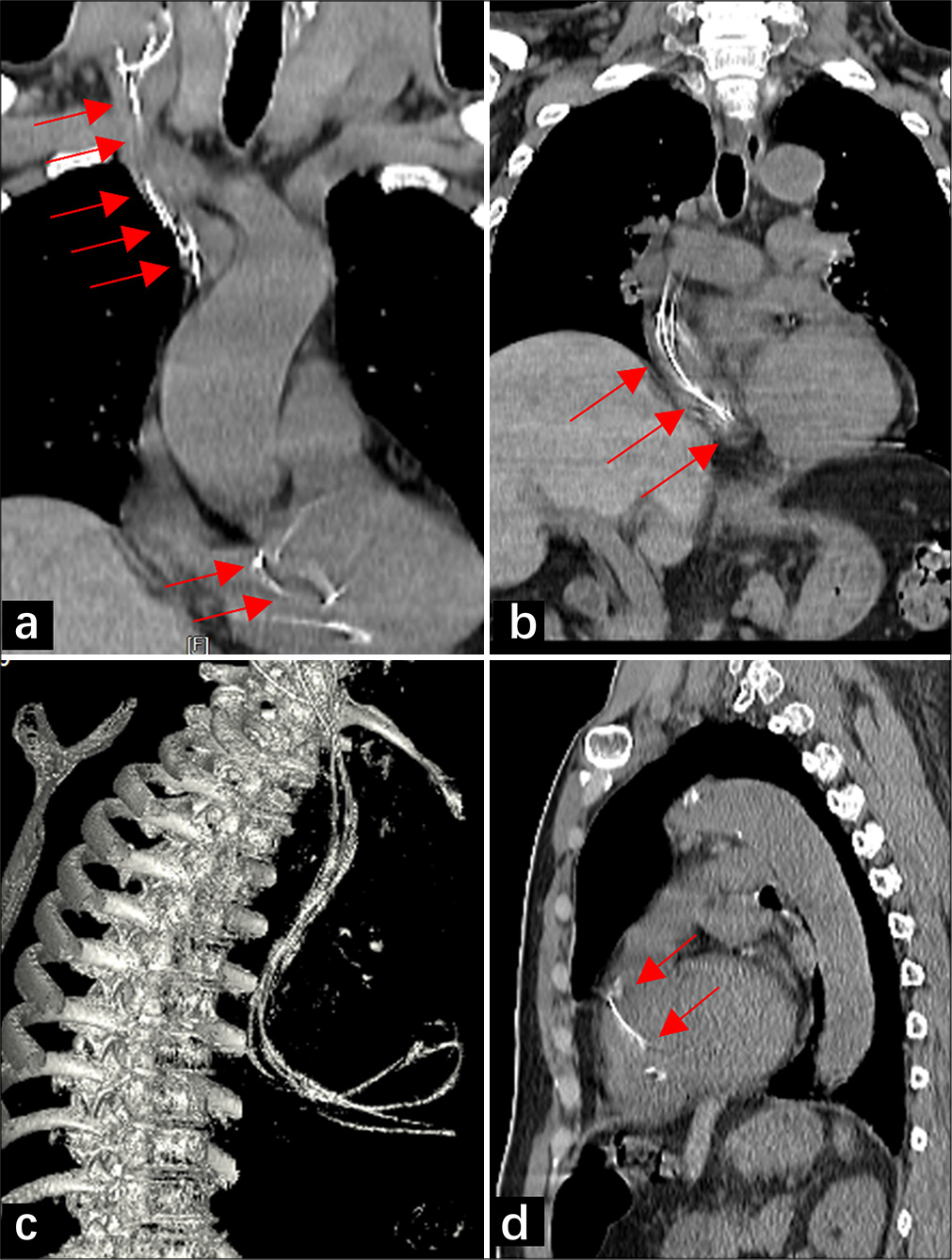
- A 67-year-old man’s head and thoracic computed tomography (CT) scan, taken 2 months after the initial ventriculoperitoneal (VP) shunt surgery. (a and b) show coronary CT images demonstrating the migration of the VP shunt catheter through the jugular vein and superior vena cava into the right heart (solid red arrow). (c) shows a maximum intensity projection reconstruction of the migrated VP shunt catheter. (d) displays a sagittal CT image showing the tip of the migrated catheter located in the pulmonary artery trunk (solid red arrow).
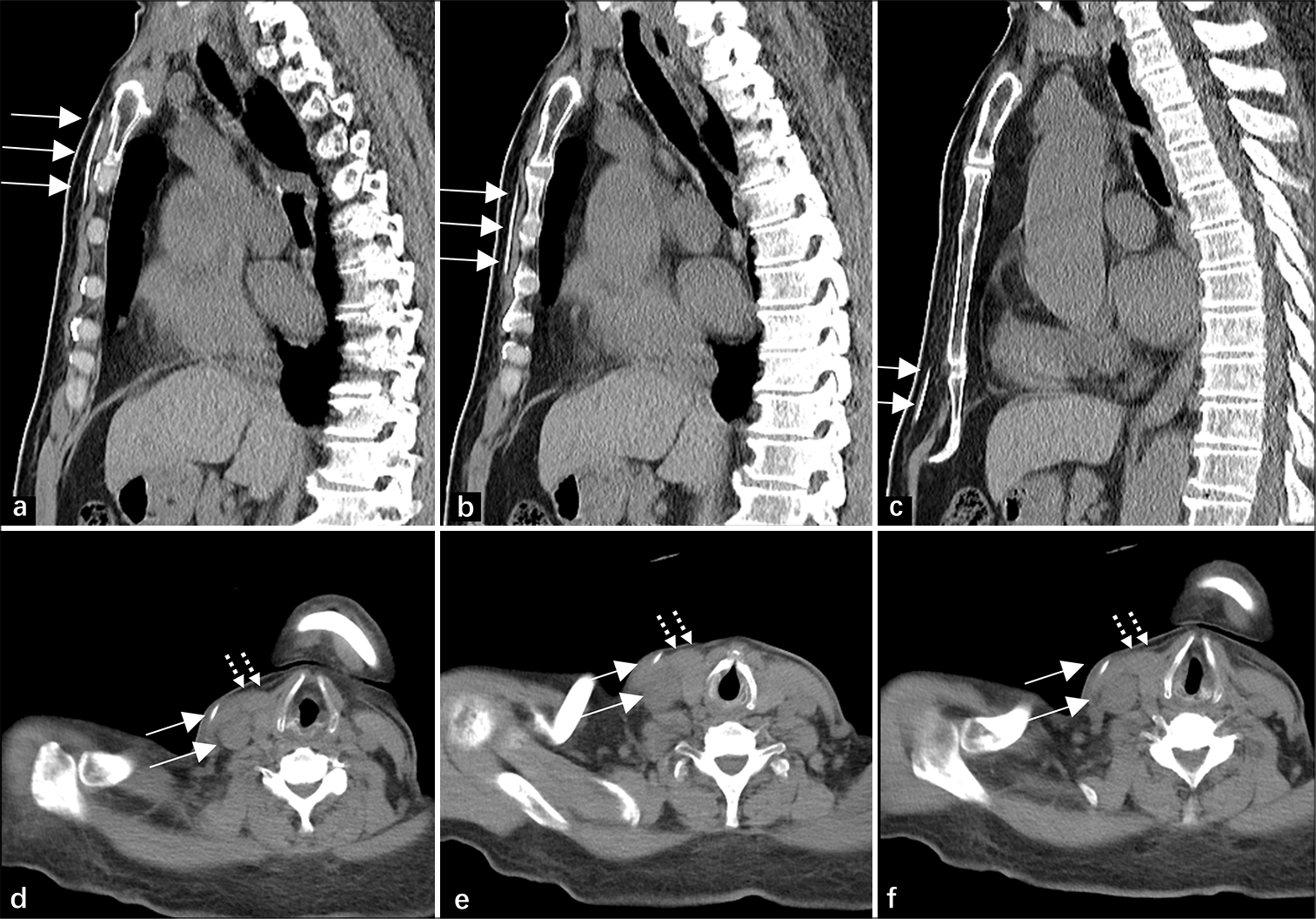
- A 67-year-old man’s head and thoracic computed tomography scan after the second ventriculoperitoneal (VP) shunt surgery. (a-c) show the course of the VP shunt catheter along the stern-abdominal wall (solid white arrow). (d-f) depict the normal position of the catheter, which is not in the right internal jugular vein (solid white arrow) and clearly delineates the sternocleidomastoid muscle (dashed white arrow).
When we retrospectively reviewed the CT scan after the initial VP shunt surgery [Figure 1], we found that the shunt catheter was passed in the wrong direction through the neck, deep to the sternocleidomastoid muscle, and penetrated the right internal jugular vein, with unclear surrounding margins and sternocleidomastoid muscle [Figure 1d-f].
DISCUSSION
Migration of a VP shunt catheter into the pulmonary artery, first described by Morell et al. in 1994, is an exceptionally rare yet potentially life-threatening complication of shunt placement.[3] Clinical presentations of this condition vary, often including signs of shunt malfunction, respiratory distress, neck pain, or, in some cases, the absence of immediate symptoms.[1,2]
Timely diagnosis relies heavily on imaging techniques. Chest X-rays are typically the first step, providing an initial assessment of the catheter’s position. CT scans, with or without 3D reconstruction, are valuable for mapping the catheter’s pathway and identifying complications like kinking or knot formation. In addition, echocardiography and angiography play crucial roles, with the latter aiding in both diagnosis and planning for potential catheter retrieval.[4,5]
Therefore, we combined relevant published studies and our case to summarize several mechanisms of VP shunt migration into the venous system. Migration is typically caused by accidental penetration of vascular structures (e.g., jugular veins) during catheter tunneling or placement.[6,7] Negative intrathoracic pressure and venous blood flow facilitate the catheter’s movement into the cardiac system and pulmonary vasculature. In addition, chronic erosion of vessel walls by the catheter has also been noted as a cause.[4] Two factors mentioned by Li et al. may promote the migration of catheters.[8] First, the subcutaneous tissue of the neck is thin, making it easier to damage the jugular vein during catheterization, so the frequency of catheter displacement is higher. Second, high-intensity rehabilitation exercises such as sit-ups can increase intra-abdominal pressure and neck movement, potentially leading to displacement.
Prompt intervention, including removal of the catheter and possible revision of the shunt system, is necessary to prevent further complications such as sepsis, pulmonary embolism, cardiovascular compromise, and arrhythmia.[9] First, manual extraction through cervical or retroarticular incision if migration is detected early.[6] Endovascular retrieval using snare catheters or guidewires is recommended for cases involving catheter knots or deep migration.[10] Open-heart surgery is the last resort in cases of severe entanglement or associated complications or applied when the aforementioned methods fail.[3,4] In our case, we highlight the important role of ultrasound monitoring the catheter status in the jugular vein to avoid entanglement or other complications.
This case also highlights the importance of obtaining a comprehensive CT scan after VP shunt catheter placement, and the course of the VP shunt catheter should be thoroughly examined to exclude anomalous penetration. Furthermore, maintaining a high index of suspicion for atypical presentations in patients with VP shunts, particularly those who present with new respiratory or hemodynamic symptoms, emphasizes the need for careful management to ensure a positive outcome.
CONCLUSION
Pulmonary artery migration of a VP shunt catheter is a rare but serious complication. Early diagnosis through imaging and prompt intervention are critical to prevent life-threatening outcomes. Management should be tailored to the extent of migration, with options ranging from manual or endovascular retrieval to open-heart surgery in severe cases. This case highlights the importance of thorough postoperative imaging and vigilant monitoring to detect atypical catheter positioning and ensure timely treatment.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: The research/study was funded by the Research project of Hunan Provincial Health Commission, Grant Number: D202304017483 and Chen Xiaoping Foundation for the Development of Science and Technology of Hubei Province, Grant Number: H2023-11.
References
- Pediatric hydrocephalus systematic review and Evidence-based guidelines task force. Pediatric hydrocephalus: Systematic literature review and evidence-based guidelines. Part 4 Cerebrospinal fluid shunt or endoscopic third ventriculostomy for the treatment of hydrocephalus in children. J Neurosurg Pediatr. 2014;14(Suppl 1):30-4.
- [CrossRef] [PubMed] [Google Scholar]
- Ventricular shunt tap as a predictor of proximal shunt malfunction in children: A prospective study. J Neurosurg Pediatr. 2008;1:439-43.
- [CrossRef] [PubMed] [Google Scholar]
- Migration of a ventriculoperitoneal shunt into the pulmonary artery. J Neurosurg Anesthesiol. 1994;6:132-4.
- [CrossRef] [PubMed] [Google Scholar]
- Peritoneal shunt migration into the pulmonary artery--case report. Neurol Med Chir (Tokyo). 2002;42:572-4.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular retrieval of migrated distal end of ventriculoperitoneal shunt from bilateral pulmonary arteries: A technical note. Ann Vasc Surg. 2017;45:305-14.
- [CrossRef] [PubMed] [Google Scholar]
- Early cardiac migration of distal shunt catheter. Br J Neurosurg. 2012;26:545-6.
- [CrossRef] [PubMed] [Google Scholar]
- Migration of a distal shunt catheter into the heart and pulmonary artery: Report of a case and review of the literature. Childs Nerv Syst. 2010;26:1113-6.
- [CrossRef] [PubMed] [Google Scholar]
- Migration of a distal ventriculoperitoneal shunt catheter into the pulmonary vasculature: A report of an unusual case and a review of the literature. J Craniofac Surg. 2019;30:e243-e4.
- [CrossRef] [PubMed] [Google Scholar]
- Sepsis caused by bacterial colonization of migrated distal ventriculoperitoneal shunt catheter into the pulmonary artery: A first case report and literature review. World Neurosurg. 2019;126:172-80.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular retrieval of detached ventriculoatrial shunt into pulmonary artery in pediatric patient: Case report. J Pediatr Neurosci. 2018;13:78-80.
- [CrossRef] [PubMed] [Google Scholar]







