Translate this page into:
Use of Cone Beam Computed Tomography in the Diagnosis of Superior Semicircular Canal Dehiscence
Address for correspondence: Dr. Ilson Sepúlveda, Otolaryngology, Head and Neck Surgery Service, General Hospital of Concepcion, San Martin AV, N° 1436, Concepción, Chile. E-mail: isepulvedaguilar@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Superior semicircular canal dehiscence is a relatively new syndrome in the field of otology. It is of unknown etiology presenting with a variety of vestibular and auditory symptoms and radiologic findings play a crucial role in its diagnosis. Cone beam computed tomography has been shown to be a powerful tool in the field of otolaryngology. It is a three dimensional technique that uses lower radiation resulting in fewer artifacts and offers higher resolution when compared with multi-slice computed tomography. It is considered to be an excellent imaging modality for radiological exploration of the ear.
Keywords
Cone beam computed tomography
dehiscence
superior semicircular canal
INTRODUCTION

Cone beam computed tomography (CBCT) is a relatively new radiological technique.[123] It was initially developed for angiography, but it has also been found useful in Oral and Maxillofacial Radiology (OMFR).[4] The introduction of CBCT has made three-dimensional imaging possible in OMFR. CBCT offers a 3D approach to data acquisition, image reconstruction, image display, and image interpretation. CBCT scan can be achieved in a relatively short period of time, making it ideal for imaging children and claustrophobic adults. The patient finds the examination comfortable as it can be performed with the patient in a standing or sitting position.[26]
The technique is characterized by fast image acquisition with relatively high three-dimensional resolution, lower radiation exposure to patients, and fewer artifacts when compared with conventional computed tomography (CT). CBCT units use image intensifiers or flat panel detectors for image acquisition. The voxels are isotropic and the resolution varies from 0.07 to 0.25 mm depending on the manufacturer. These values exceed most high-grade multi-slice CT units in terms of spatial resolution, real time image analysis, and three-dimensional display.[178]
CBCT technology has been used for preoperative implant planning, evaluation of the jaws, and presurgical assessment of the bone volume required for orthognathic surgery. As CBCT systems have become more prevalent, its use has gained attention in the field of otolaryngology.[1] CBCT of the inner ear [Figures 1 and 2] is effective in the diagnoses of most malformations, dysplasia, traumatic lesions, thin osseous labyrinthine wall erosion, or dehiscence.[291011] The advantages and diagnostic value of CBCT have been demonstrated in the analysis of the position of cochlear implants in the temporal bone, the free visualization of alloplastic middle ear titanium, gold, or platinum implants. It is also possible that the smallest bone structure or position of the prosthesis can be defined with high precision contributing valuable information to the diagnosis, preoperative planning, and prevention of intra-operative complications.[238]
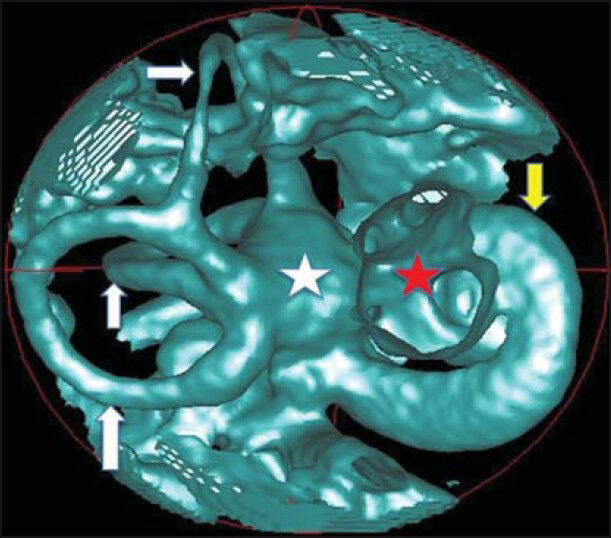
- 60-year-old female patient with clinical history of hearing loss diagnosed with sensorineural hearing loss. CBCT of temporal bone three-dimensional image with air cavity volume rendering (green), shows normal inner ear: Semicircular canals (white arrows), vestibule (white star), cochlea (yellow arrow) and internal auditory canal (red star).

- 28-year-old male patient with clinical history of bilateral hearing loss and semicircular canal dehiscence diagnosed with conductive hearing loss due to bilateral fixing of the malleus. Bilateral CBCT of temporal bone three-dimensional image with osseous volume rendering demonstrates normal superior semicircular canal.
Superior semicircular canal dehiscence
A semicircular canal dehiscence (SCD) is characterized by a pathological opening in a small section of the bony wall of the semicircular canal (SC) of the inner ear. An SCD can be found in three different places according to different etiologies: The superior [Figures 3 and 4], lateral, and posterior SCs. Regardless of differences in SCD location, dehiscence patients have complained of similar symptoms such as vertigo, oscillopsia, and/or hearing loss.[12]
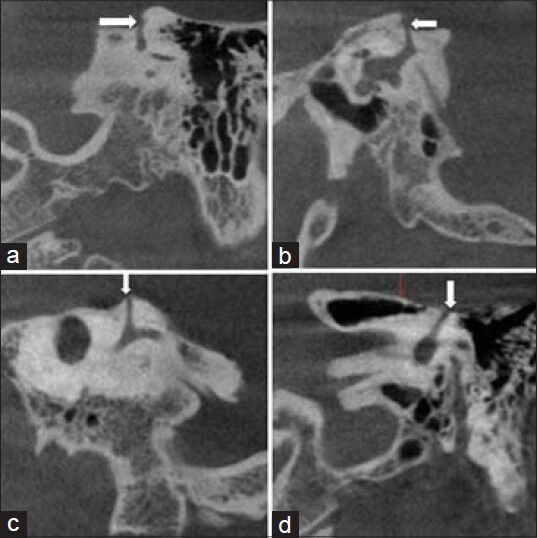
- 35-year-old male patient with clinical history of vertigo and autophony diagnosed with left superior semicircular canal dehiscence. CBCT of temporal bone (a and d) coronal (b) sagittal (c) oblique sagittal images show a dehiscence of the left superior semicircular canal (white arrow).
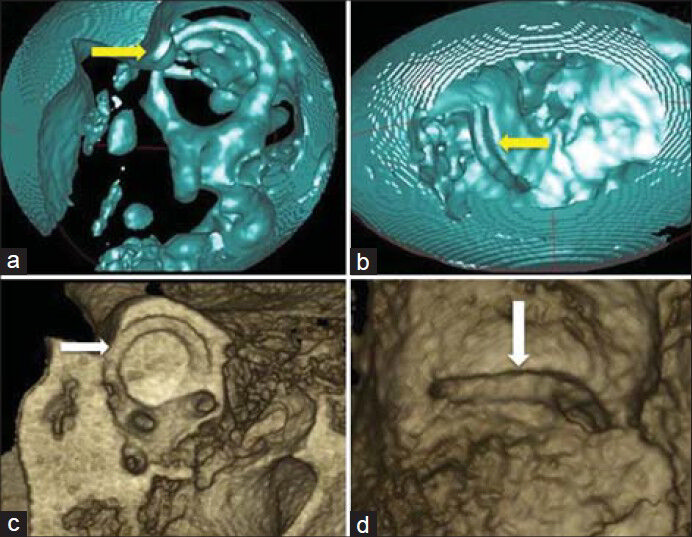
- 17-year-old patient with clinic history of progressive hearing loss, without vertigo and oscillopsia diagnosed with sensorineural hearing loss and right superior semicircular canal dehiscence. CBCT of temporal bone, air cavity volume rendering (green) images (a) sagittal view, (b) endocranial view, (c) osseous volume rendering oblique sagittal view and (d) osseous volume rendering superior view show superior semicircular canal dehiscence (yellow arrow in a), (yellow arrow in b), (white arrow in c), and (white arrow in d).
Superior semicircular canal dehiscence (SSCD) syndrome is characterized by sound and/or pressure-induced vertigo and oscillopsia due to a dehiscence of bone overlying the superior SC in the roof of the temporal bone or in the neighborhood of the epidural space. This often leads to a so-called “third mobile window”. Minor et al., first described this in 1998, and it has become a new and exciting concept in the field of otology.[1314151617181920] Vertigo as a result of loud noises (Tullio phenomenon), autophony, oscillopsia, disequilibrium due to sound changes in middle ear pressure, or changes in intracranial pressure were observed in these patients. SSCD may present with a variety of atypical vestibular and/or auditory symptoms, which can be suggestive of otosclerosis. SSCD is relatively rare, the reported cases in the literature range from 0.4% to 0.7% with the majority of patients being asymptomatic.[1317202122]
The etiology of SSCD syndrome is unknown.[1314] Several etiologies have been linked to hereditary, developmental, intracranial hypertension, and trauma.[17] Other authors have suggested that SSCD may be due to a congenital or a genetic condition.[1923] SSCD most commonly occurs along the apex or the roof of the SC, termed the arcuate eminente. However, approximately 9.1% of SSCD may also occur more posteriorly or medially, involving the groove of the superior petrosal sinus[24] [Figure 5].
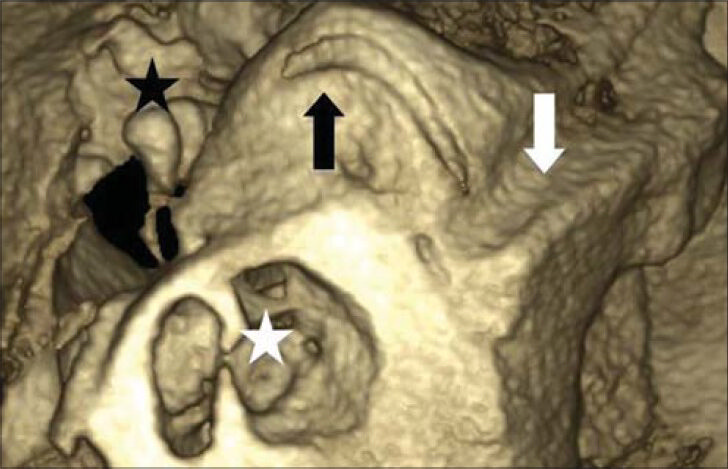
- 42-year-old male patient, with clinical history of cranial trauma and initial diagnosis of left temporal bone fracture diagnosed with left temporal bone fracture and ipsilateral superior semicircular canal dehiscence. CBCT of temporal bone shows incidental find of dehiscence of the superior semicircular canal (black arrow) in superior petrosal sinus canal area (white arrow), cochlea (white star), and ossicle chain (black star).
Diagnosis of SSCD is based on the presence of vestibular or auditory symptoms and radiologic findings. The dehiscence is confirmed with high resolution computed tomography (HRCT) scanning of the temporal bones using bone window settings. This is a key component in the diagnosis of SSCD, especially when a surgical intervention is contemplated. SSCD is detected on CT scans in 3.6% of patients. In 2005, Minor reported a sensitivity of 100%, a specificity of 99%, a positive predictive value of 99%, and a negative predictive value of 100% in the identification of SSCD.[1416171820212225]
DISCUSSION
Teymoortash et al., analyzed radiological imaging of 43 structures of the temporal bone by CBCT and CT in 38 human temporal bones. The frequency of visualization of these anatomic structures were studied and statistically analyzed: 9 structures (20.1%) of axial scans and 5 structures (11.6%) of coronal scans could be identified as statistically significantly (P < 0.05) more often in CBCT than in CT. They determined that anatomical structures of the temporal bone can be identified significantly better in CBCT than in CT scans.[2]
Cloutier et al., analyzed a total of 581 temporal bone CT scans. A dehiscent-appearing superior canal was seen in 4.0% of cases, while published pathologic studies reported that only 0.5% of temporal bone SSCs have a dehiscence (P < 0.001). They established that the prevalence of dehiscent-appearing superior canal on thin-section temporal bone scanning with reformation in the SSC plane is much higher than anticipated by pathologic studies.[18]
Dalchow et al., examined 434 patients with CBCT. Eleven patients with a history of peripheral vertigo presented a fistula of the labyrinth. The results were compared with intra-operative findings to evaluate the diagnostic value of CBCT in cases of erosion of the SCs. They determined the presence of a fistula of the SCs in 100% of the cases.[9]
CONCLUSION
In conclusion, when compared with multi detector computed tomography, CBCT imaging for the inner ear is an excellent alternative. It results in lower radiation to patients, fewer artifacts, and equal or higher resolution depending on the unit used.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/49/141554
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Comparison of simulated cone beam computed tomography to conventional helical computed tomography for imaging of rhinosinusitis. Laryngoscope 2014 [Epub ahead of print]
- [Google Scholar]
- Temporal bone imaging using digital volume tomography and computed tomography: A comparative cadaveric radiological study. Surg Radiol Anat. 2011;33:123-8.
- [Google Scholar]
- Presentation of floating mass transducer and Vibroplasty Couplers on CT and Cone Beam CT. Eur Arch Otorhinolaryngol. 2014;271:665-72.
- [Google Scholar]
- Evaluation of mastoid pneumatization using cone-beam computed tomography. Oral Radiol. 2014;30:92-7.
- [Google Scholar]
- Maxillofacial cone beam computed tomography: Essence, elements and steps to interpretation. Austral Dent J. 2012;57:46-60.
- [Google Scholar]
- Movement of the patient and the cone beam computed tomography scanner: Objectives and possible solutions. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:769-73.
- [Google Scholar]
- Prevalence and characteristics of pneumatization of the temporal bone evaluated by cone beam computed tomography. Int J Oral Maxillofac Surg. 2013;42:771-5.
- [Google Scholar]
- Use of cone beam computed tomography in otolaryngologic treatments. Eur Arch Otorhinolaryngol. 2012;269:711-20.
- [Google Scholar]
- Radiographic examination of patients with dehiscence of semicircular canals with digital volume tomography. Eur Arch Otorhinolaryngol. 2013;270:511-9.
- [Google Scholar]
- A comparative evaluation of Cone Beam Computed Tomography (CBCT) and Multi-Slice CT (MSCT). Part II: On 3D model accuracy. Eur J Radiol. 2010;75:270-4.
- [Google Scholar]
- Cone-beam imaging: Applications in ENT. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128:65-78.
- [Google Scholar]
- Superior-semicircular-canal dehiscence: Effects of location, shape, and size on sound conduction. Hear Res. 2013;301:72-84.
- [Google Scholar]
- Evaluation of the superior semicircular canal morphology using cone beam computed tomography: A possible correlation for temporomandibular joint symptoms. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117:e280-8.
- [Google Scholar]
- Semicircular canal dehiscence in the pediatric population. Int J Pediatr Otorhinolaryngol. 2009;73:321-7.
- [Google Scholar]
- Bilateral superior semicircular canal dehiscence in a child with sensorineural hearing loss and without vestibular symptoms. Int J Pediatr Otorhinolaryngol. 2011;75:877-9.
- [Google Scholar]
- Semicircular canal dehiscence in HR multislice computed tomography: Distribution, frequency, and clinical relevante. Eur Arch Otorhinolaryngol. 2012;269:475-80.
- [Google Scholar]
- Superior canal dehiscence syndrome: Clinical manifestations and radiologic correlations. Eur Arch Otorhinolaryngol 2013 [Epub ahead of print]
- [Google Scholar]
- Superior semicircular canal dehiscence: Positive predictive value of high-resolution CT scanning. Eur Arch Otorhinolaryngol. 2008;265:1455-60.
- [Google Scholar]
- Superior semicircular canal dehiscence in a young child: Implication of developmental defect. Int J Pediatr Otorhinolaryngol. 2007;71:1925-8.
- [Google Scholar]
- Anatomo-radiological study of the superior semicircular canal dehiscence radiological considerations of superior and posterior semicircular canals. Eur J Radiol. 2010;76:167-72.
- [Google Scholar]
- Superior semicircular canal dehiscence: A possible pathway for intracranial spread of infection. Am J Otolaryngol. 2012;33:263-5.
- [Google Scholar]
- Superior semicircular canal dehiscence diagnosed after failed stapedotomy for conductive hearing loss. Am J Otolaryngol. 2011;32:441-4.
- [Google Scholar]
- Dehiscence of the superior semicircular canal: A review of the literature on its possible pathogenic explanations. Eur Arch Otorhinolaryngol. 2014;271:435-7.
- [Google Scholar]
- Semicircular canal dehiscence. Operative Techniques in Otolaryngology-Head and Neck Surgery. 2014;25:118-24.
- [Google Scholar]
- Diagnosis and outcomes of middle cranial fossa repair for patients with superior semicircular canal dehiscence syndrome. J Clin Neurosci. 2010;17:339-41.
- [Google Scholar]






