Traumatic Extra-capsular and Intra-capsular Floating Fat: Fat-fluid Levels of the Knee Revisited
Address for correspondence: Dr. Derik L Davis, Department of Diagnostic Radiology and Nuclear Medicine, University of Maryland School of Medicine, 22 S. Greene Street, Baltimore, Maryland 21201, USA. E-mail: ddavis7@umm.edu
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Floating fat is a sign of acute bone injury at the knee following trauma. The goal of this article is to review the etiology, patterns, and mimickers of extra-capsular and intra-capsular floating fat, with the major emphasis on knee trauma in the acute setting. We will discuss the spectrum of multimodal imaging findings for rare presentations of extra-capsular floating fat, and contrast these with common and atypical forms of intra-capsular lipohemarthrosis, as an aid to the assessment of acute bone trauma at the knee.
Keywords
Extra-capsular
floating fat
knee
lipohemarthrosis
trauma

INTRODUCTION
Lipohemarthrosis is defined as the presence of intra-capsular floating fat in a joint cavity.[1] Traumatic knee injury represents the most common cause, and lipohemarthrosis is widely considered pathognomonic for acute fracture.[234] Lipohemarthrosis occurs in 35–41% of knees presenting with intra-articular fracture.[56] Thus, lipohemarthrosis is an important sign, since knee trauma accounts for nearly 532,000 annual visits to the emergency department in the United States.[78]
The search for intra-capsular floating fat on knee radiographs following trauma has been taught ever since Holmgren first described lipohemarthrosis on radiographs more than 75 years ago.[69] As intra-articular fractures are occult on radiographs in 15% of knees, the presence of a fat–fluid level is sufficient to prompt additional radiographic views or cross-sectional studies to identify the fracture.[21011] Extra-capsular floating fat is rarely encountered, in contrast to lipohemarthrosis. Extra-capsular fat–fluid levels, by definition, are located outside of the knee joint cavity.[1213141516] In this article, we will discuss the spectrum of imaging findings for rare presentations of extra-capsular floating fat and contrast these with common and atypical forms of lipohemarthrosis. Also, rare causes and mimickers of fat–fluid levels at the knee will be reviewed, but the major emphasis will involve discussion of traumatic floating fat since most cases present in the emergency setting following acute injury.
ANATOMY
The knee joint cavity is enveloped by the joint capsule, which has an outer fibrous layer and an inner synovial layer. The articular surfaces of the femur, tibia, and patella are contained within the joint capsule. The suprapatellar bursa is an intra-capsular space which freely communicates with the knee joint cavity, and is often referred to as the suprapatellar pouch or recess after a septum separating the two cavities resolves in the fourth month of fetal development.[17] The suprapatellar pouch is an anterior midline structure which is located deep to the quadriceps tendon.[18] Numerous anterior, posterior, lateral, and medial recesses reside in the intra-capsular joint space of the knee.[19]
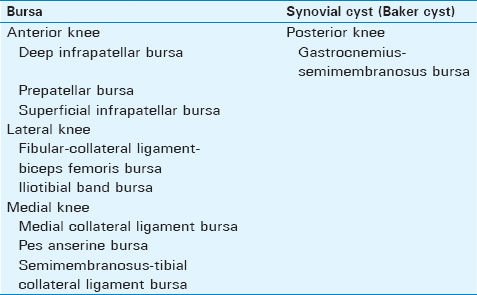
Several distinct extra-capsular soft tissues are located deep to the crural fascia at the knee, including the collateral ligaments, extensor mechanism, muscles, and deep fat. The skin and subcutaneous fat are superficial to the crural fascia. Numerous extra-capsular bursae are present in the periarticular soft tissues of the knee [Table 1]. Bursae function to reduce friction between osseous, myotendinous, and ligamentous tissues deep to the crural fascia, although some are located superficial to the crural fascia. These synovial spaces are not typically visible on imaging studies, unless distended by fluid.[18]
ETIOLOGY
Intra-capsular lipohemarthrosis
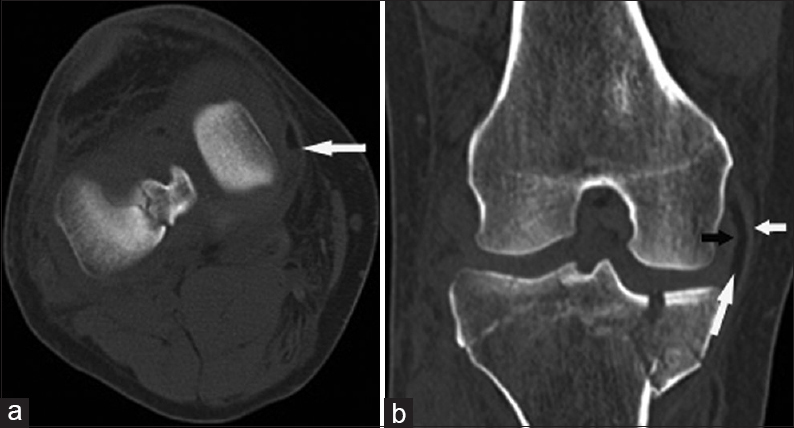
Intra-capsular fat–fluid levels result from the introduction of fatty tissue into the knee joint cavity. Fat naturally separates from fluid based on physical composition, since hydrophobic fat does not mix with hydrophilic fluid. Intra-articular fracture is the most common mechanism for leakage of fatty bone marrow and blood into the knee joint cavity [Figure 1a and b].[220] Traumatic rupture of synovial membranes, capsuloligamentous structures, and intra-capsular fat pads, such as Hoffa's fat pad, are additional rare mechanisms for release of intra-articular fat.[2021] Iatrogenic lipohemarthrosis is not an uncommon sign when imaging is performed in the immediate postoperative setting following open reduction internal fixation across an articular surface [Figure 1c]. Rarely, cortical destruction from osteomyelitis allows passage of fatty marrow into the knee joint cavity without associated trauma.[15] In this setting, rapid septic necrosis of adipose cells in the marrow cavity releases free fatty globules, which pass through a cortical defect, the cloaca, and present as lipohemarthrosis when floating in joint fluid.[12]

- 26-year-old man after a fall presents with lipohemarthrosis. (a) Cross-table lateral radiograph shows a fat–fluid level at the anterior knee (arrows). (b) Axial computed tomography (CT) image shows lipohemarthrosis (white arrow) and an acute non-displaced intra-articular fracture of the medial femoral condyle (black arrow). 43-year-old man status post recent intramedullary rod fixation of an acute midshaft femoral fracture presents with lipohemarthrosis. (c) Sagittal T1-weighted MR image shows a globule of fat (long arrow) floating on fluid and intra-capsular air (asterisk). The intramedullary rod (short arrow) is partially included in the field of view.
Extra-capsular floating fat
The location of a fat–fluid level outside of the knee joint cavity differentiates this rare phenomenon from intra-capsular lipohemarthrosis. The release of fatty tissue into a normal anatomic extra-capsular soft tissue synovial space or an acquired post-traumatic soft-tissue wound results in a fat–fluid level when blood or fluid is present in the same space. Synovial spaces include extra-capsular bursa and synovial cysts. The bony medullary space and periosteum are additional rare sites for extra-capsular fat–fluid levels.
The mechanism for release of floating fatty tissue into an extra-capsular bursa in the setting of trauma is most often an adjacent bony fracture transecting the bursal wall, allowing leakage of fatty marrow into the synovial space. This is equivalent to the mechanism described for the presence of floating fat found in tendon sheaths at the wrist and ankle[Figure 2a and b].[1622] Similarly, the presence of a fat–fluid level in a post-traumatic soft tissue wound cavity also most likely results from the direct leakage of fatty marrow from an adjacent fractured bone.

- 76-year-old man after a motor vehicular accident presents with extra-capsular fat–fluid levels. (a) Cross-table lateral radiograph shows fat–fluid levels in the prepatellar (long white arrow) and superficial infrapatellar bursae (short white arrow), along with lipohemarthrosis (black arrow) and acute comminuted patellar and tibia fractures. (b) Axial CT image shows the prepatellar bursa fat–fluid level (white arrow) and the adjacent acute comminuted patellar fracture (black arrow). 61-year-old man following acute intra-articular tibial fracture presents with an extra-capsular fat–fluid level (c) Axial CT image shows a fat–fluid level in a Baker cyst (long white arrow). Lipohemarthrosis is seen anteriorly (short white arrow).
The presence of a fat–fluid level in an extra-capsular synovial cyst most often results from “escape” of floating fat from an intra-capsular lipohemarthrosis. Baker cysts are the most frequently encountered synovial cysts at the knee. Typically, synovial cysts are formed by a portion of the intra-capsular lining becoming trapped in an extra-capsular position. Increasing intra-articular pressure forces the fluid to escape across the least path of resistance into the extra-capsular synovial cyst,[18] and in the context of lipohemarthrosis, floating fatty marrow is trapped in the synovial cyst [Figure 2c].
Rare extra-capsular fat–fluid levels in the soft tissues, or bony periosteum and medullary space, have most often been described as the sequela of osteomyelitis.[12131415] In this setting, rapid septic necrosis of adipose cells in the marrow cavity releases free fatty globules which float on a fluid layer of pus.[12]
PATTERNS OF FAT–FLUID INTERACTION
Fat–fluid levels
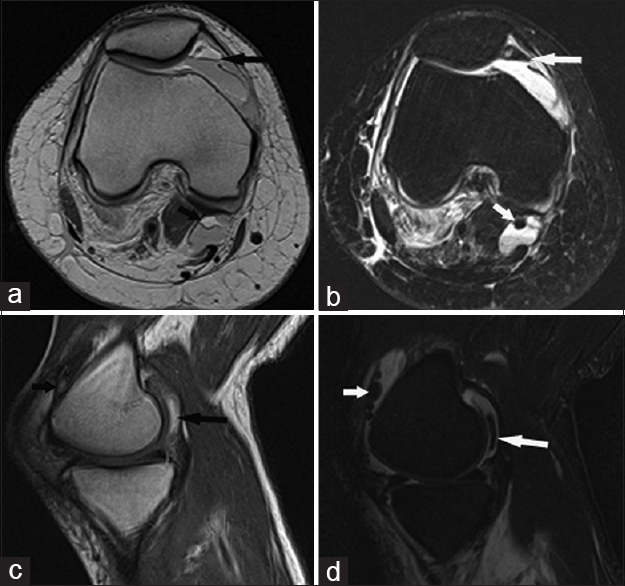
The typical fat–fluid level is sharply demarcated on imaging, based on the physical properties of fat and fluid. Distinct fat–fluid layers usually are present 3 h after intramedullary fat is introduced into a fluid containing space.[4] Fat is less dense than fluid, and thus forms the top layer and “floats” on the fluid based on gravity.[20] Thus, the visualization of two distinct adjacent liquid layers represents the most basic fat–fluid level, and is often referred to as a single “fluid–fluid level” [Figure 3a]. However, the fluid component also has the potential to separate further into serum and red blood cell precipitate layers. In this instance, the serum assumes a non-dependent position relative to the heavier red blood cell precipitate.[4] In this case, three distinct adjacent liquid layers are identified, which is referred to as a “double fluid–fluid level” [Figure 3b and c].

- 18-year-old-man following blunt trauma presents with lipohemarthrosis and an acute intra-articular tibial fracture. (a) Sagittal T1-weighted MR image shows a single fluid–fluid level presentation of lipohemarthrosis in both the suprapatellar pouch (short white arrow) and posterior recess deep to the medial head gastrocnemius muscle (long white arrow). An acute tibial fracture is also present (black arrow). 39-year-old man after a fall presents with lipohemarthrosis. (b) Cross-table radiograph and (c) sagittal CT images show a double fluid–fluid level lipohemarthrosis, with distinct fat–fluid (short white arrows) and fluid–fluid (black arrows) levels following acute intra-articular tibial fracture (long white arrow).
Globular fat–fluid interfaces
The presence of fat globules interspersed in fluid is a less commonly encountered imaging appearance of fat–fluid interaction [Figure 4]. This appearance is similar to globules of fat interspersed in bloody fluid in a syringe following diagnostic aspiration.[23] The presence of fat globules occurs in the first 2 h after intramedullary fat is introduced into the fluid containing space, before giving way to the more typically encountered straight-edge fat–fluid level appearance by the third hour.[4] Fat globules are also uncommonly encountered at the fat–fluid border, producing an undulating appearance along the fat–fluid interface [Figure 5].
- 60-year-old woman after a motor vehicle collision presents with lipohemarthrosis. (a) Axial proton density-weighted and (b) T2-weighted fat-saturated images show a globule of fat in a Baker cyst (short arrows). The straight-edge appearance of lipohemarthrosis is also present anteriorly (long arrows). 37-year-old man with an acute intra-articular tibial fracture presents with lipohemarthrosis. (c) Sagittal T1-weighted and (d) STIR-weighted images show a globule of fat in the posterior recess deep to the medial head gastrocnemius muscle (long arrows). Additional globules are present in the suprapatellar pouch (short arrows).

- 25-year-old man after a motor vehicle collision presents with an atypical pattern of lipohemarthrosis. (a) Sagittal T1-weighted image shows an undulating globular fat–fluid level pattern distally (arrow) and a straight-edge appearance proximally. 34-year-old man after a fall with an atypical pattern of lipohemarthrosis. (b) Axial T2-weighted fat-saturated image shows a bizarre-appearing interface between intra-capsular floating fat and fluid (arrows).
IMAGING
Radiographs
Radiographs are the most common imaging test for the initial evaluation of knee pain or trauma, due to the appropriateness, availability, and short acquisition time of the examination.[24] The cross-table lateral view (horizontal-beam technique) is the most sensitive radiographic technique to detect intra-capsular lipohemarthrosis at the knee [Figure 1a].[6] Radiographs distinguish the floating lipid layer from the fluid layer based on density.[25] Conventional anteroposterior and lateral views are less sensitive for detection of lipohemarthrosis, since each lacks the exact horizontal orientation necessary to distinguish floating fat from fluid and the superimposed knee soft tissues.[21] Radiographic detection of a single fluid–fluid level is not entirely pathognomonic of lipohemarthrosis, since separation of hemarthrosis into serum and red blood cell precipitate levels also produces a single fluid–fluid level appearance.[426] A double fluid–fluid level is more specific for lipohemarthrosis [Figure 3b].[4] In contrast to lipohemarthrosis, detection of fat–fluid levels on radiographs is less reliable for extra-capsular floating fat due to the variable locations of these collections and the summation artifact of overlapping bone and soft-tissue density.
Computed tomography
Computed tomography (CT) is the gold standard for detection of lipohemarthrosis in the setting of acute knee trauma.[27] CT further characterizes fracture patterns found on knee radiographs and localizes radiographically occult fractures in the setting of lipohemarthrosis [Figure 1b]. Similar to radiographs, differentiation of layering intra-capsular joint effusion into different cellular components is based on density. Low-attenuation fat floats in a non-dependent position above the fluid layer of hemarthrosis [Figure 3c].[321] Hounsfield units reflect fat and blood densities in the single fluid–fluid level presentation or fat, water, and blood densities in the double fluid–fluid level pattern. The multiplanar capabilities of CT also allow for improved sensitivity for detection and characterization of rare extra-capsular fat–fluid levels, which are most often occult or confusing on radiographic studies.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) rivals CT as the gold standard for detection of lipohemarthrosis.[28] MRI also localizes radiographically occult fractures in the setting of lipohemarthrosis [Figure 3a]. Characterization of lipohemarthrosis is dependent on the tissue relaxation times of fat and blood.[425] The non-dependent fluid layer of lipohemarthrosis follows fat signal on all pulse sequences, and a thin zone of chemical shift artifact separates the fat layer from the dependent layer of hemarthrosis [Figure 5]. MRI sequences also allow for detection of distinct serum and red blood cell components of hemarthrosis. Multiplanar MRI detects extra-capsular fat–fluid levels to greater advantage than radiographs, in a similar fashion to CT.
Ultrasound
Ultrasound is an adjunct imaging modality in the setting of acute knee trauma. Ultrasound evaluation of knee trauma is not routine, but is used selectively in the context of point-of-care treatment in the emergency department to screen the suprapatellar pouch of the knee joint cavity when clinical suspicion is high for a radiographically occult fracture.[727] Direct detection of bony injury with ultrasound is poor, but identification of lipohemarthrosis leads to a presumption that an acute intra-articular fracture is present.[27] The sonographic appearance of lipohemarthrosis includes a non-dependent hyperechoic layer, an anechoic middle serum layer, and a dependent hypoechoic red blood cell precipitate layer.[20] In some cases, the anechoic serum layer is absent.[27]
Ultrasound is less sensitive compared to CT or MRI for the detection of extra-capsular fat–fluid levels or the presence of lipohemarthrosis in the knee joint cavity in areas other than the suprapatellar pouch. Ultrasound is also operator-dependent, and the patients' physical condition and pain can limit diagnostic sensitivity.[21]
TRAUMATIC EXTRA-CAPSULAR FLOATING FAT
Synovial spaces
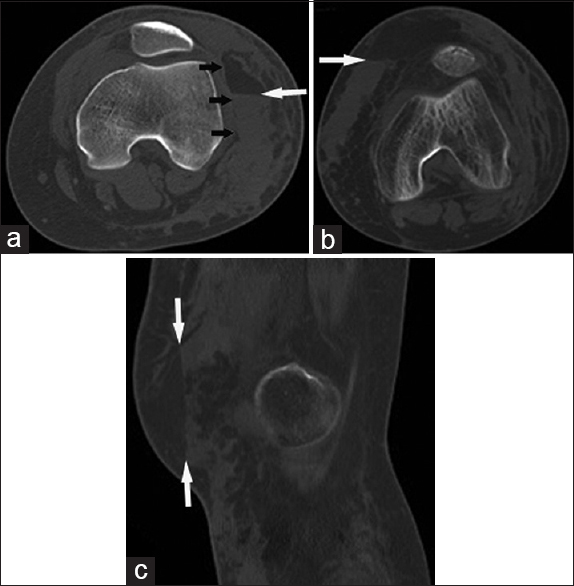
Baker cysts are present in more than half of adult knees, and are well-known findings on cross-sectional imaging studies.[18] Floating fat in these synovial spaces should not be unexpected in the presence of traumatic intra-capsular lipohemarthrosis [Figures 2c, 4a and b]. Fat–fluid levels are also found among the commonly and not-so commonly encountered bursae following acute fracture [Figures 2b and 6–8].
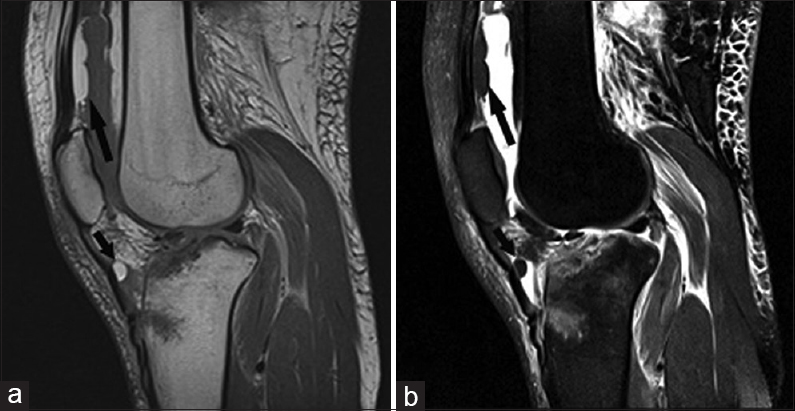
- 25-year-old man with an acute tibial fracture after a motor vehicle collision presents with extra-capsular floating fat. (a) Sagittal T1- and (b) sagittal T2-weighted fat-saturated images show a floating globule of fat (short arrows) in the deep infrapatellar bursa and lipohemarthrosis (long arrows).
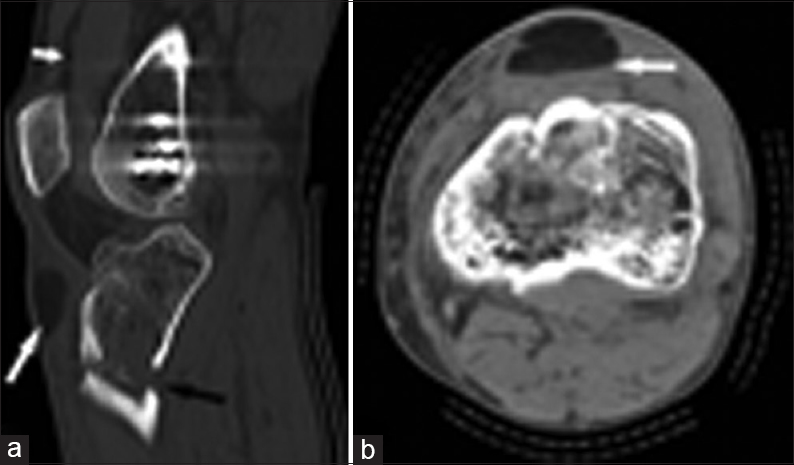
- 47-year-old man following acute tibial fracture presents with a superficial infrapatellar bursa fat–fluid level. (a) Sagittal CT image shows fat distending the superficial infrapatellar bursa (long white arrow), an acute tibial fracture (long black arrow), and lipohemarthrosis (short white arrow). (b) Axial CT image shows a fat–fluid level in the superficial infrapatellar bursa (arrow) and adjacent acute cortical disruption of the anterior proximal tibia.
- 39-year-old man after a fall presents with a medial collateral ligament bursa fat–fluid level. (a) Axial CT image shows a fat–fluid level in the medical collateral ligament (MCL) bursa (arrow). (b) Coronal CT image shows the fat-containing MCL bursa (long white arrow) between the superficial (short white arrow) and deep (black arrow) layers of the MCL, and also an acute comminuted fracture involving the medial and lateral tibial plateau.
Post-traumatic soft-tissue wounds
A Morel-Lavallée lesion is the result of a closed degloving injury, and is a non-anatomic soft tissue cavity along the perifascial plane created by the traumatic separation of the hypodermis from the underlying crural fascia by a blunt tangential force.[2930] The cavity fills with blood and lymphatic drainage in hours to days after the inciting trauma, and may persist for months to years after the formation of a fibrous pseudocapsule.[3031] In the acute setting, fat–fluid levels in a Morel-Lavallée lesion are a rare finding and are most often found in association with an acute fracture [Figure 9a].[16]
- 18-year-old-female pedestrian struck by an automobile presents with an extra-capsular fat–fluid levels in a non-anatomic soft-tissue space. (a) Axial CT image shows a fat–fluid level (long arrow) collecting in a Morel-Lavallée lesion, occurring in the subcutaneous fat along the margin of the crural fascia (short arrows). 77-year-old man following a motor vehicle accident presents with floating fat in an extra-capsular non-anatomic soft-tissue space. (b) Axial and (c) sagittal CT images show a distinct fat–fluid level centered in the subcutaneous fat (arrows). The post-traumatic fluid collection is not associated with the crural fascia, and does not conform to the location of an extra-capsular bursa.
Fat–fluid levels centered in the subcutaneous fat, at a distance from the perifascial plane and not meeting the definition of a Morel-Lavallée lesion, are also rarely encountered. These fat–fluid collections are found in hours to days following acute blunt trauma, likely in association with an acute fracture[Figure 9b and c].
DIFFERENTIAL DIAGNOSIS
Intra-capsular lipohemarthrosis
In the setting of hemarthrosis, intra-capsular fatty masses mimic lipohemarthrosis on cross-sectional imaging. Benign intra-capsular fatty masses include lipoma arborescens and lipoma.[41632] Lipoma arborescens is an uncommon lipomatous proliferation of the intra-capsular synovium. Malignant intra-capsular liposarcoma is rarely encountered.[33] Intra-capsular lipohemarthrosis is usually differentiated from an intra-articular fatty mass on clinical grounds,[4] and follow-up imaging would show persistence of the intra-articular fatty mass over time in challenging cases.
Extra-capsular floating fat
Benign periarticular soft-tissue masses uncommonly presenting with internal fat–fluid levels include lymphangiomas and dermoid cysts.[12343536] Malignant liposarcoma with an internal fluid component can mimic a fat–fluid level, although an actual fat–fluid level is rare.[3738] The presence of floating fat adjacent to an acute bony fracture and the subsequent resolution over time would distinguish extra-capsular floating fat from these masses.
CONCLUSION
The discovery of a fat–fluid level at the knee should prompt a search for an associated fracture in the setting of acute injury. Lipohemarthrosis is the most common presentation, although rare forms of extra-capsular floating fat are also encountered. Knowledge of the imaging patterns of floating fat will aid in the assessment of acute bone trauma at the knee.
Financial support and sponsorship
The authors have no grant funding to declare.
Conflicts of interest
Dr. Derik L. Davis has no disclosure or conflict of interest to declare. Dr. Prasann Vachhani has no disclosure or conflict of interest to declare.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/60/170729
REFERENCES
- Floating fat in the wrist joint and in the tendon sheaths. Skeletal Radiol. 2010;39:931-3.
- [Google Scholar]
- Bone bruise, lipohemarthrosis, and joint effusion in CT of non-displaced hip fracture. Acta Radiol. 2012;53:197-202.
- [Google Scholar]
- Evolving stages of lipohemarthrosis of the knee. Sequential magnetic resonance imaging findings in cadavers with clinical correlation. Invest Radiol. 1997;32:7-11.
- [Google Scholar]
- MR findings in patients with acute tibial plateau fractures. Comput Med Imaging Graph. 1996;20:389-94.
- [Google Scholar]
- Lipohemarthrosis of the knee: A review of recent experiences. Radiology. 1989;173:189-91.
- [Google Scholar]
- Identification of lipohemarthrosis with point-of-care emergency ultrasonography: Case report and brief literature review. J Emerg Med. 2013;44:453-6.
- [Google Scholar]
- National Hospital Ambulatory Medical Care Survey: 2004 emergency department summary. Adv Data 2006:1-29.
- [Google Scholar]
- Acute haemarthrosis of the knee in athletes. A prospective study of 106 cases. J Bone Joint Surg Br. 1993;75:945-9.
- [Google Scholar]
- Diagnosis and triage of a patient with an extra-osseous fat fluid level. Emerg Radiol. 2011;18:503-5.
- [Google Scholar]
- Extramedullary fat fluid level on MRI as a specific sign for osteomyelitis. Australas Radiol. 2003;47:443-6.
- [Google Scholar]
- Extra-osseous fat fluid level: A specific sign for osteomyelitis. Skeletal Radiol. 2007;36(Suppl 1):S101-4.
- [Google Scholar]
- Hematogenous osteomyelitis with fat-fluid level shown by CT. Radiology. 1984;153:493-4.
- [Google Scholar]
- The double fat fluid level: Lipohemarthrosis of the knee associated with suprapatellar plica synovialis. Skeletal Radiol. 1983;10:30-3.
- [Google Scholar]
- MR imaging of cysts, ganglia, and bursae about the knee. Radiol Clin North Am. 2007;45:969-82, vi.
- [Google Scholar]
- Synovial recesses of the knee: MR imaging review of anatomical and pathological features. Skeletal Radiol. 2009;38:317-28.
- [Google Scholar]
- Sonographic evaluation of lipohemarthrosis: Clinical and in vitro study. J Ultrasound Med. 1995;14:279-82.
- [Google Scholar]
- Lipohemarthrosis of the knee: MRI as an alternative to the puncture of the knee joint. Eur Radiol. 2003;13:1185-7.
- [Google Scholar]
- Non-displaced distal radius fracture with fat-fluid levels in the adjacent extensor tendon sheaths on MRI. Skeletal Radiol. 2013;42:1761-5.
- [Google Scholar]
- ACR appropriateness criteria® acute trauma to the knee. J Am Coll Radiol. 2012;9:96-103.
- [Google Scholar]
- Fluid-fluid levels in injured knees: Do they always represent lipohemarthrosis? Radiology. 1996;198:499-502.
- [Google Scholar]
- Role of magnetic resonance imaging in musculoskeletal trauma. Top Magn Reson Imaging. 2007;18:155-68.
- [Google Scholar]
- Long-standing Morel-Lavallee lesions of the trochanteric region and proximal thigh: MRI features in five patients. AJR Am J Roentgenol. 2004;182:1289-94.
- [Google Scholar]
- MRI findings of prepatellar Morel-Lavallée effusions. Skeletal Radiol. 2008;37:451-5.
- [Google Scholar]
- Progressive hematoma in an older adult: Closed internal degloving injury of the knee. Am J Orthop (Beale Mead NJ). 2013;42:376-8.
- [Google Scholar]
- Orthopaedic case of the month: A painless right knee mass in a 55-year-old woman. Diagnosis: Intraarticular lipoma. Clin Orthop Relat Res. 2013;471:1100-4.
- [Google Scholar]
- High-grade intra-articular liposarcoma of the knee. Skeletal Radiol. 2011;40:363-5.
- [Google Scholar]
- Giant dermoid cyst of the lower limb: Presentation of a rare case. J Cutan Med Surg. 2011;15:125-7.
- [Google Scholar]
- Large dermoid cyst of the left hip: Radiological approach with histopathology assessment. BMJ Case Rep. 2013;pii:bcr2012007943.
- [Google Scholar]
- Well-differentiated liposarcoma of the retroperitoneum with a fat-fluid level: US, CT, and MR appearance. Eur Radiol. 1998;8:474-5.
- [Google Scholar]
- Imaging of liposarcoma: Classification, patterns of tumor recurrence, and response to treatment. AJR Am J Roentgenol. 2011;197:W37-43.
- [Google Scholar]






