Translate this page into:
Transluminal Recanalization of Chronic Total Occlusion of Radial Artery Using Rendezvous Technique: A Case Report and Literature Review
Address for correspondence: Dr. Mohammad Arabi, Department of Medical Imaging, Prince Sultan Military Medical City, Riyadh - 11159, Kingdom of Saudi Arabia. E-mail: marabi2004@hotmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Although endovascular management of lower extremity peripheral arterial disease (PAD) is well studied, little information exists regarding endovascular treatment of critical upper limb ischemia. We report a case of transluminal recanalization of right radial artery chronic total occlusion (CTO) using rendezvous technique in a patient with critical hand ischemia and dry gangrene of the right index finger.
Keywords
Angioplasty
radial artery
recanalization
rendezvous
INTRODUCTION

Symptomatic upper limb occlusive disease is uncommon due to the presence of a rich network of collaterals. Etiologies include vasculitis, connective tissue disorders, embolic causes, thoracic outlet syndrome, traumatic vascular injuries, and atherosclerosis.[12] In contrast to the lower extremities, peripheral arterial disease (PAD) in the upper extremities is less frequent and commonly involves the brachiocephalic and subclavian arteries rather than below-the-elbow (BTE) arteries. Furthermore, upper extremity PAD is more prevalent in patients with end-stage renal disease (ESRD) on hemodialysis, who may present with critical limb ischemia due to chronic total occlusion (CTO) secondary to extensive vascular calcifications and the steal phenomenon related to arteriovenous fistulas.[3] In addition, radial access has become the standard access for coronary interventions in many institutions, which may result in radial artery occlusion in 1-10%.[4] Although usually asymptomatic, several case reports of symptomatic occlusion have been published.[56] Endovascular management of critical upper limb ischemia consists mainly of intra-arterial thrombolysis and angioplasty of above-the-elbow arteries depending on the underlying etiology. Recanalization of BTE CTO is rarely described in literature. We describe a successful case of revascularization of radial artery CTO using rendezvous technique, with a brief literature review of the previously reported endovascular techniques of upper limb arterial revascularization.
CASE REPORT
A 74-year-old man, with a history of diabetes mellitus, hypertension, ESRD on hemodialysis, and PAD, who had previously undergone right below-the-knee amputation, presented with a few months history of dry gangrene of the right index finger [Figure 1]. The patient had no arteriovenous fistula in the upper limb. On examination, gangrenous tissue was seen at the lateral aspect of the distal phalanx of the right index finger. Weak monophasic Doppler signal was detected in the radial and ulnar arteries. Computed tomography angiography (CTA) of the right upper extremity showed a focal moderate stenosis of the right axillary artery and extensive calcifications of the radial and ulnar arteries limiting proper evaluation of luminal opacification. Prior to the planned procedure, a loading dose of 160 mg of acetyl salicylic acid (ASA) and 300 mg of clopidogrel was administered orally. Conventional angiography through right common femoral artery access showed moderate stenosis at the right axillary artery [Figure 2], which was successfully treated with 6-mm Evercross balloon (ev3 Endovascular, Inc., Plymouth, MN, USA). The ulnar artery was totally occluded proximally, and the radial artery showed long segments of multifocal stenosis and focal CTO [Figure 3a]. A 5-Fr, 90-cm guiding catheter was introduced into the distal brachial artery and a 2.8-Fr, 135-cm Progreat microcatheter (Terumo Medical Corporation, Somerset, NJ, USA) was coaxially inserted to negotiate the focal total occlusion of the radial artery, which ultimately failed in the antegrade approach. Therefore, the distal radial artery was retrogradely accessed under fluoroscopy and ultrasound guidance, and a 4-Fr, 7-cm sheath was placed. A 0.035″ straight hydrophilic wire and a 4-Fr catheter were negotiated through the focal radial occlusion and a 300-cm, 0.014″ Transend wire (Boston Scientific Corporation, Natick, MA, USA) was advanced into the proximal guiding catheter using rendezvous technique. Antegrade angioplasty of the radial artery was performed using 2 mm and 3.5 mm × 8 cm × 150 cm Amphirion Deep balloons (Medtronic, Minneapolis, MN, USA), which resulted in marked improvement of flow [Figure 3b]. Following the procedure, palpable radial pulse was detected and the patient reported immediate subjective improvement of numbness, pain, and hand temperature. The patient was started on dual anticoagulation therapy including lifelong ASA and clopidogrel for 6 months. Interventional radiology clinic visit at 4 weeks showed partial healing of the gangrene [Figure 4] and improved sensation in the index finger. Color Doppler evaluation of the radial artery revealed patent vessel with biphasic waveform. At 2 months, the patient presented with excruciating pain at the index finger tip, which necessitated amputation of the distal and middle phalanges. On the same admission, the patient also underwent left superficial femoral artery angioplasty due to dry gangrene of the left big toe. Radial angiogram that was performed following the procedure showed recurrence of a short segment of high-grade stenosis at the level of the recanalized occluded segment [Figure 3c].

- 74-year-old presented with dry gangrene of the right index finger. Photo of the patient's right hand shows dry gangrene of the index finger (arrows).
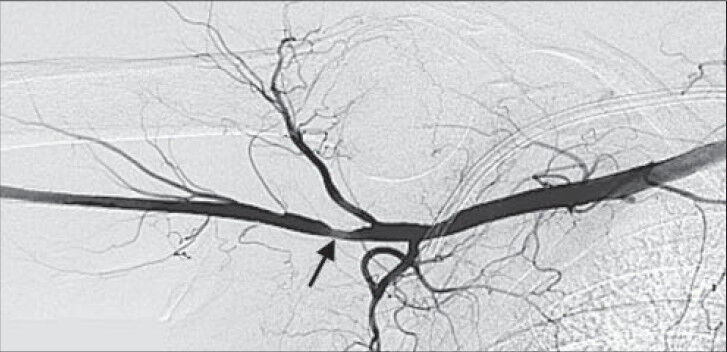
- 74-year-old presented with dry gangrene of the right index finger. Digital subtraction angiography (DSA) of the right axillary artery shows focal moderate stenosis (arrow).
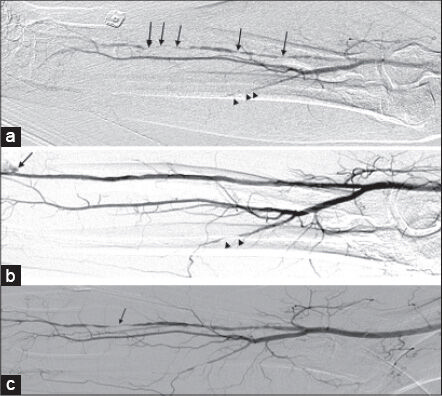
- 74-year-old presented with dry gangrene of the right index finger. a) DSA of the right radial artery shows a long segment of multifocal stenosis/ occlusion (arrows) and occlusion of the ulnar artery. b) Post percutaneous transluminal angioplasty (PTA) DSA shows marked improvement of flow within the radial artery. Minimal extravasation is seen at the radial puncture site (arrow), which was readily controlled by manual pressure. Proximal occlusion of the ulnar artery is seen (arrowheads). c) Two-month follow-up DSA shows recurrence of a short segment of high-grade stenosis at the level of the previously recanalized occluded vessel (arrow).

- 74-year-old presented with dry gangrene of the right index finger. Photo of the patient's right hand at 4-week follow-up shows partial healing of the gangrene (arrows).
DISCUSSION
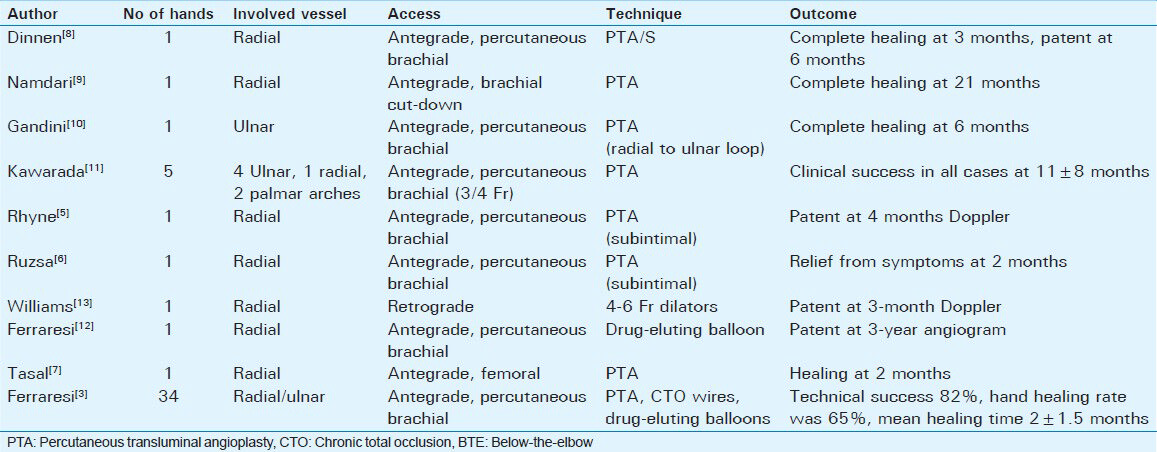
Percutaneous recanalization of BTE CTO is rarely described in literature. Ferraresi et al., evaluated the feasibility, safety, and outcomes of percutaneous transluminal angioplasty (PTA) in the treatment of chronic hand ischemia due to BTE disease in 28 patients with 34 affected hands.[3] Most of the patients in the cohort had a long history of diabetes mellitus, ESRD on hemodialysis, and systemic atherosclerosis. The inter-osseous artery was free of disease in all cases, while the radial and ulnar arteries were simultaneously involved in 90% with mean lesion length greater than 10 cm. Although technical success was achieved in 82% of cases, hand healing rate was 65% with a mean time of 2 ± 1.5 months. They concluded that technical success rate and poor digital run-off are the predictors of hand healing following PTA.
The choice of approach to the target BTE arteries depends on the extent of disease in one or more vessels, accessibility of the lesion, and the availability of balloon and stent catheters of proper length to reach the target lesions. BTE CTO lesions may be approached using percutaneous antegrade fashion either via femoral[7] or brachial access.[35689101112] Alternatively, percutaneous retrograde access through direct puncture of the radial artery may be done.[13] Surgical cut-down may be needed to gain antegrade access to the brachial artery to perform antegrade balloon angioplasty of the radial artery.[9] Gandini et al., reported retrograde recanalization of the ulnar artery using radial-to-ulnar artery loop technique via the superficial palmar arch, with complete healing of the digital ulcerations at 6 months follow-up.[10]
Different revascularization techniques of critical upper limb ischemia secondary to BTE disease are summarized in Table 1. Regular balloons ranging between 2 and 3 mm are mainly utilized for radial or ulnar angioplasty, while 2-mm balloons are used in the palmar arch. Recently, drug-eluting balloons have been utilized to perform BTE angioplasty.[312] However, the outcomes of the latter balloons need to be validated in comparison to other techniques. A case of primary use of self-expandable stents in radial CTO resulted in healing of the digital gangrene within 3 months and maintained patency of the radial artery at 6-month follow-up.[8] Self-expandable stents were also successfully used to treat flow-limiting dissections during radial PTA.[3]
In our case, the retrograde access to the radial artery was obtained due to the difficulty in crossing the focal CTO antegradely. The rendezvous technique provided a more stable access to the true lumen to facilitate transluminal angioplasty. Since handling long balloons from the radial access can be practically difficult for the operator, the balloons were introduced from the femoral approach utilizing the through-and-through wire.
CONCLUSION
The present case illustrates the use of the rendezvous technique in endovascular revascularization of upper limb ischemia secondary to BTE CTO and supports the pre-existing evidence regarding its clinical benefit.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/36/135663
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Upper limb ischemia: 20 years experience from a single center. Vascular. 2005;13:84-91.
- [Google Scholar]
- Angioplasty of below-the-elbow arteries in critical hand ischaemia. Eur J Vasc Endovasc Surg. 2012;43:73-80.
- [Google Scholar]
- Radial artery patency after transradial catheterization. Circ Cardiovasc Interv. 2012;5:127-33.
- [Google Scholar]
- Hand ischemia resulting from a transradial intervention: Successful management with radial artery angioplasty. Catheter Cardiovasc Interv. 2010;76:383-6.
- [Google Scholar]
- Anterograde recanalisation of the radial artery followed by transradial angioplasty. Cardiovasc Revasc Med. 2010;11:266. e1-4
- [Google Scholar]
- Successful angioplasty for radial artery chronic total occlusion in a patient with digital gangrene. Postepy Kardiol Interwencyjnej. 2013;9:304-6.
- [Google Scholar]
- Successful percutaneous angioplasty and stenting of the radial artery in a patient with chronic upper extremity ischemia and digital gangrene. J Endovasc Ther. 2007;14:426-8.
- [Google Scholar]
- Chronic hand ischemia treated with radial artery balloon angioplasty: Case report. J Hand Surg Am. 2008;33:551-4.
- [Google Scholar]
- Percutaneous transluminal angioplasty for treatment of critical hand ischemia with a novel endovascular approach: “The radial to ulnar artery loop technique”. J Vasc Surg. 2010;51:760-2.
- [Google Scholar]
- Angioplasty of ulnar or radial arteries to treat critical hand ischemia: Use of 3- and 4-French systems. Catheter Cardiovasc Interv. 2010;76:345-50.
- [Google Scholar]
- First use of drug-eluting balloon for below-the-elbow artery occlusion in a hemodialysis patient: A 3-year follow-up. J Vasc Access. 2013;14:202-3.
- [Google Scholar]
- Recanalization of a chronic radial artery occlusion allowing subsequent complex coronary intervention. Circ Cardiovasc Interv. 2012;5:e34-6.
- [Google Scholar]






