Translate this page into:
The imaging presentation of head and neck oncologic emergencies

*Corresponding author: Rahim Ismail, Department of Imaging Sciences, URMC, Rochester, New York, United States. rahim_ismail@urmc.rochester.edu
-
Received: ,
Accepted: ,
How to cite this article: Ismail R, Schartz D, Manganaro M, Paton C, Kessler A. The imaging presentation of head and neck oncologic emergencies. J Clin Imaging Sci 2025;15:7. doi: 10.25259/JCIS_136_2023
Abstract
This review describes the radiographic findings in emergencies of head and neck cancers (HNCs) in both undiagnosed and previously treated patients, with an emphasis on the temporal urgency of each presentation and in association with the relevant clinical presentation and necessary treatments to enhance understanding and recognition. The various presentations of HNC will be described by the organ system of their presenting complaint. The development and complications of each will be elaborated, with a focus on the clinical presentation in the emergency department and the imaging findings that are critical to recognize in making the diagnosis. Each presentation will be exhibited with a specific patient case and the exact computed tomography, magnetic resonance imaging, ultrasound, or digital subtraction angiography images obtained will be shown. Cases include airway obstruction due to glottic tumor or metastatic cervical lymphadenopathy; airway obstruction due to surgical complications of hematoma, or post-radiation soft-tissue edema; vascular complications of tumor or nodal compression, carotid blowout, carotid stenosis, or occlusion; orbital complications of compartment syndrome; and orthopedic complications of osteomyelitis and osteoradionecrosis. Eleven HNC patient cases are presented with their associated 32 images. HNC patients present with challenging imaging features in the emergent setting. Difficulty in discerning the correct diagnosis arises from the complex head and neck anatomy, often compounded by an advanced stage at presentation and poor functional status. Radiologist familiarity with common HNC emergent presentations is essential for accurate diagnosis and timely treatment.
Keywords
Head
Neck
Vascular
Oncology
Emergency
INTRODUCTION
Head and neck cancers (HNCs) are highly diverse and comprise nearly 4% of all cancers within the United States. While some subtypes of HNC are decreasing in overall incidence, others are either stable or becoming more common – for example, oropharyngeal cancer due to human papillomavirus infection, or salivary gland neoplasms for unclear reasons.[1,2] As a result, HNC patients are presenting acutely to the emergency department (ED) at increasing rates.[3] HNC patients can develop emergent symptoms/complications which can result in complex clinical and imaging presentations. Furthermore, acute presentations of HNC pathology can be a diagnostic radiological challenge in part due to the complexity of HNC anatomy combined with the advanced stage of presentation, and poor functional status, which can lead to disastrous consequences for missed diagnoses. In addition, the interval between symptom onset and clinical presentation is often prolonged in HNC compared to other cancers.[4] In fact, a retrospective review by Bannister et al. found that all patients presenting on an emergency basis (either initial or post-diagnosis), did so at higher cancer stages (level 3 or 4).[5] Because of this, a thorough knowledge of imaging features of HNC emergencies is critical for making both accurate and timely diagnoses for these patients. The purpose of this review is to describe radiographic findings in oncological emergencies in both undiagnosed and previously treated HNC patients.
AIRWAY
Stridor is the second most common presenting symptom for emergency room patients with HNC, second only to dysphagia.[5] In addition, tracheostomies are the most common emergent intervention required in this population.[6] Likewise, some studies have suggested that oropharyngeal cancers are the most common cause of acute airway obstruction.[5] It is thought that this may be a consequence of initial misdiagnosis; slowly growing oropharyngeal tumors might be incorrectly identified as recurrent infection/tonsillitis which results in continued tumor growth and risk of airway compromise. Alternatively, this delayed presentation may occur because these oropharyngeal cancers grow slowly, causing insidious symptoms that a patient may disregard before seeking treatment. Furthermore, given the anatomical location of oropharyngeal/glottic malignancies, the associated edema and/or hemorrhage can result in emergent airway obstruction [Figures 1 and 2]. Glottic tumors or metastatic cervical lymphadenopathy may also result in chronic vocal cord paralysis due to the involvement of the vocal folds or recurrent laryngeal nerve. It is important to note that rapid growth in the tumor (from submucosal edema or intratumoral hemorrhage) superimposed on chronic vocal cord paralysis can precipitate acute airway compromise, although this danger is much less common.
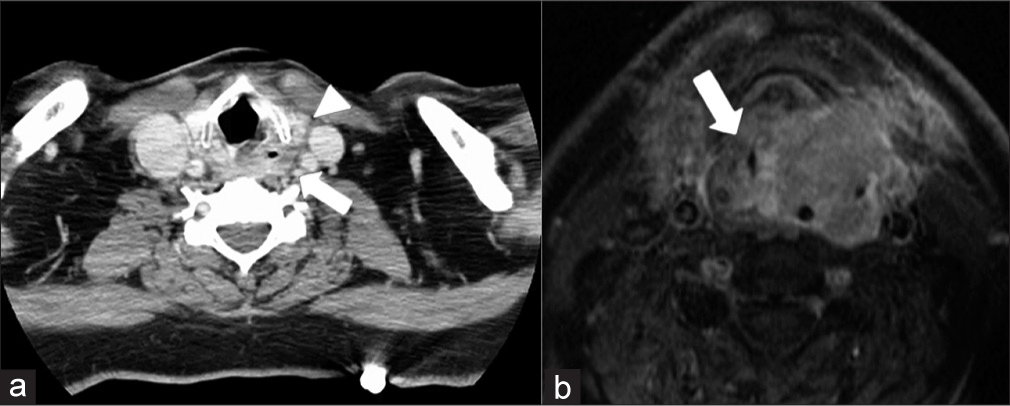
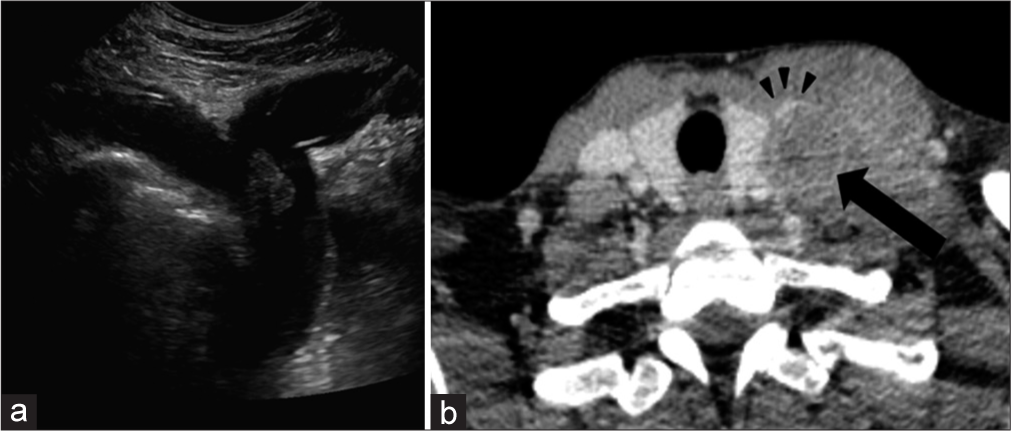
- A 57-year-old male smoker with 4–5 weeks of progressive dysphagia and dyspnea. (a) Prior axial contrast-enhanced computed tomography image demonstrates a left hypopharyngeal mass extending along the aryepiglottic fold (arrow). There is extralaryngeal extension through the thyrohyoid membrane (arrowhead), (b) Axial T1 fat-saturated post-contrast image after emergent tracheostomy placement now shows near complete obliteration of the supraglottic airway with a larger mass (arrow).
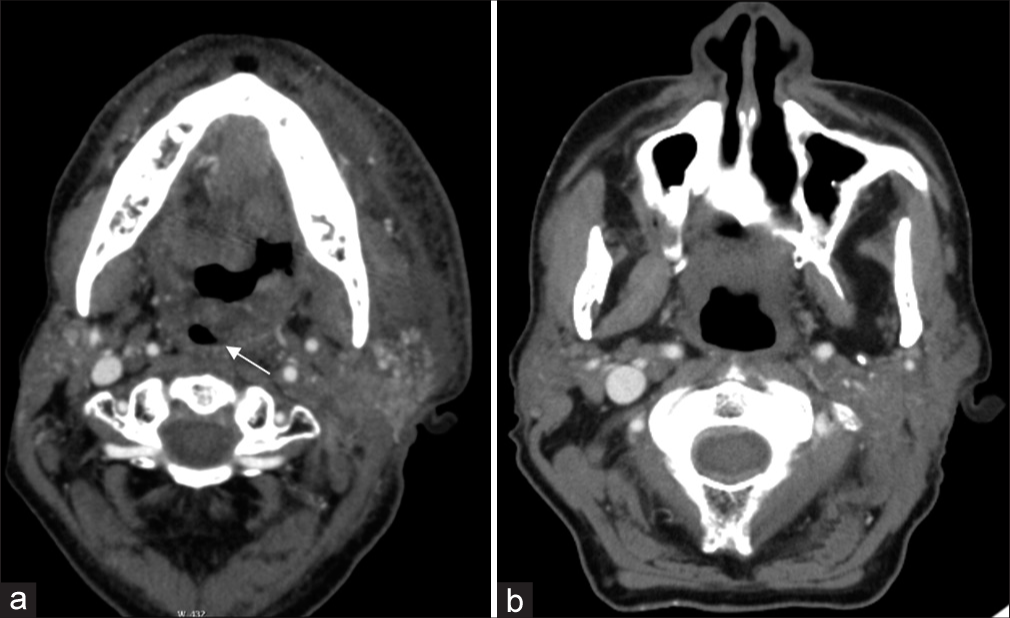
- A 59-year-old man with a history of carcinoma of the base of the tongue status post-radiation treatment presenting for symptoms of worsening dysphagia and dyspnea. (a) Axial contrast-enhanced computed tomography (CT) image demonstrates irregular mucosal nodularity along the left base of the tongue and posterolateral oropharyngeal wall. Note the significant resultant narrowing of the oropharyngeal lumen posterior to the uvula (white arrow), This obstruction has rapidly grown from the axial contrast-enhanced CT image approximately 1 month prior, (b) which demonstrated relative patency of the lumen.
Special considerations in post-treatment patients
Post-treatment patients can have different etiologies of airway obstruction. Post-surgical airway compromise is not an uncommon phenomenon in the post-anesthesia care unit and relies heavily on clinical/endoscopic evaluation.[7] On the other hand, radiation injury tends to arise more insidiously, requiring imaging to play a critical role in identification and subsequent management.
Radiation therapy, either alone or combined with chemotherapy or surgery, is utilized in the vast majority of squamous cell cancer (SCC) HNC patients. Radiation damages endothelial cells lining small blood vessels, leading to ischemia, edema, and ultimately fibrosis. In the early post-radiation period, this endothelial damage results in disruption of the venous and lymphatic drainage and results in significant interstitial edema, most commonly manifested on computed tomography (CT) as reticulations within the subcutaneous fat or thickening of the dermis along the port trajectory.[8] Consequently, an emergent presentation can occur when there is an accumulation of laryngeal or retropharyngeal edema-resulting in acute airway compromise. Key clinical information that can help clarify the clinical scenario includes radiation timing and dosage. There is a significant increase in the risk of edema with increased radiation dose, leading some authors to recommend 43.5 Gy or below at 2 Gy/fraction to reduce this risk.[9] Early edematous changes typically occur between 2 and 12 weeks of treatment [Figure 3] and chronic laryngeal edema has been found to have a median observation time of 36 weeks.[10] Additional sequelae, such as osteoradionecrosis peak at 1 year after treatment, and are further discussed below.
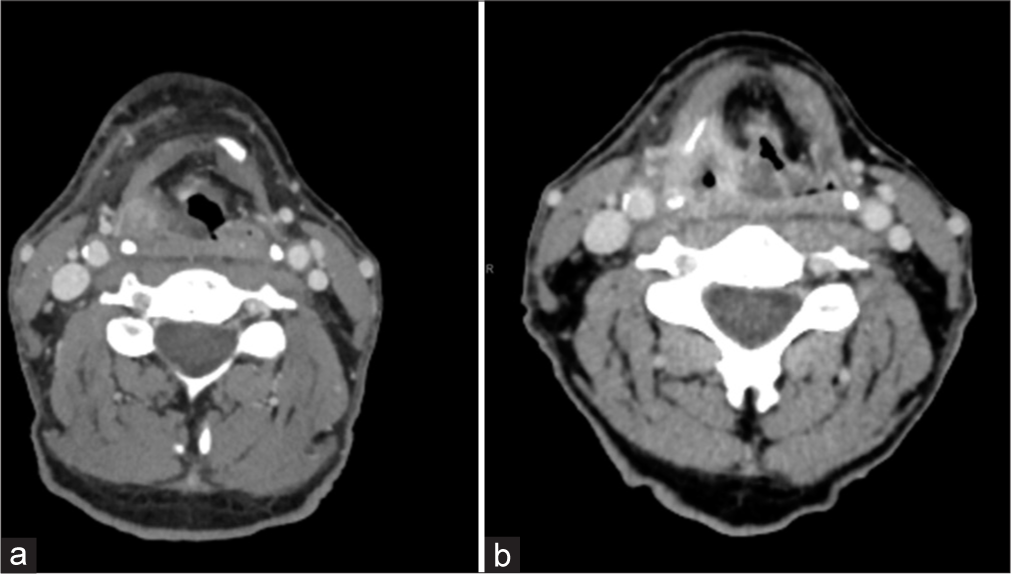
- A 62-year-old man with biopsy-proven squamous cell carcinoma status post high-dose radiation treatment. Computed tomography (CT) images demonstrate submucosal edema in the posterior pharyngeal wall causing supraglottic airway stenosis (b), which progressed from the prior CT soft tissues of the neck approximately 6 months prior (a). Imaging was obtained just over 2 weeks into the start of a 6-week radiation treatment course. (CT: computed tomography)
Temporal variability in symptom onset
An important point must be considered when regarding the variability in the timing of the aforementioned post-radiation changes. For example, osteoradionecrosis has been reported in patients up to 50 years after treatment.[11] While the typical onset of chronic laryngeal edema is less than a year as described above, [Figure 4] demonstrates an emergent presentation of a 63-year-old man who developed acute symptoms of increased dyspnea and inability to speak in full sentences which occurred 3.5 years after chemoradiation treatment.
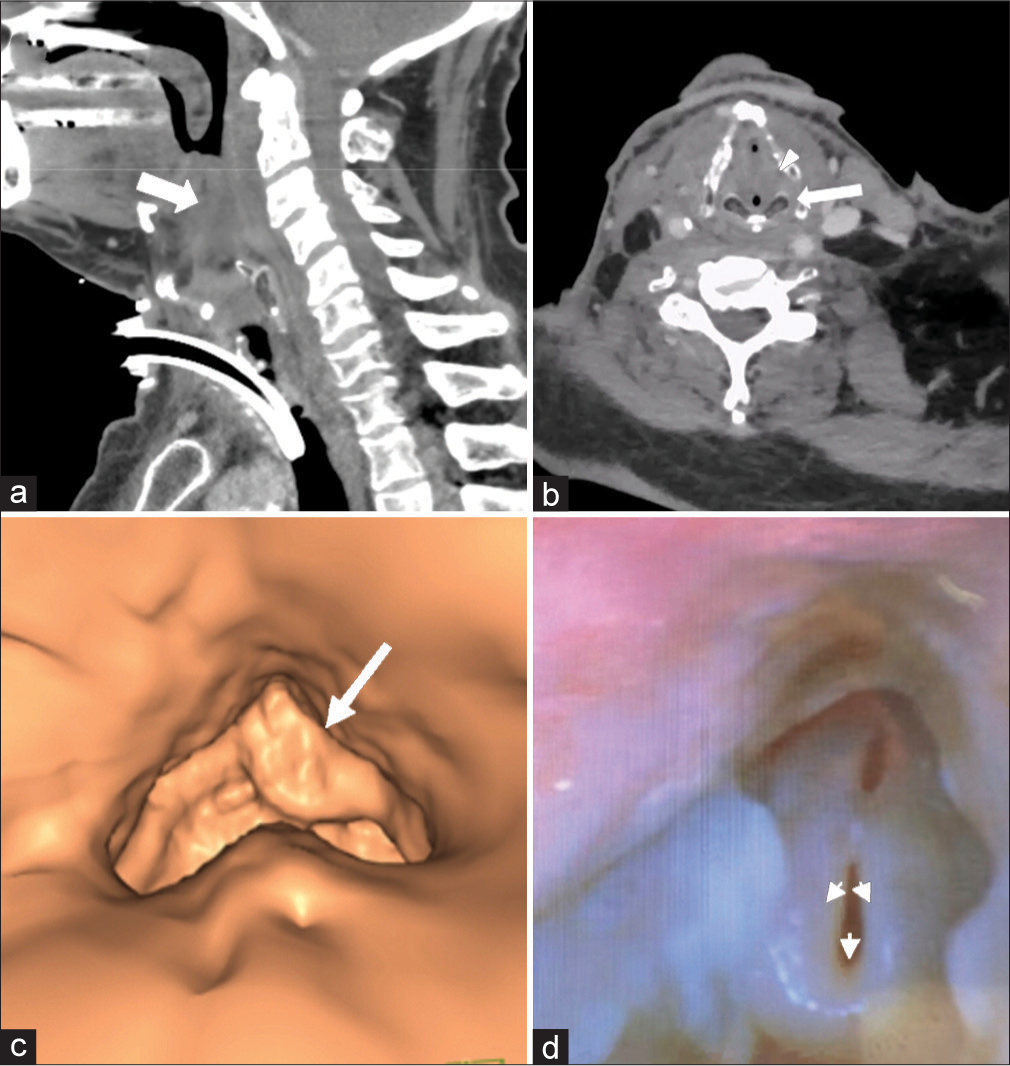
- A 63-year-old man with a history of p16 positive tonsillar squamous cell cancer s/p chemoradiation, completed 3.5 years prior. Serial outpatient cancer surveillance endoscopies showed stable curled epiglottis and arytenoid edema. Later, the patient presented acutely with several hours of increased dyspnea and inability to speak in full sentences. In (a and b) sagittal and axial contrast-enhanced computed tomography images demonstrate severe edema of the supraglottic airway (white arrow), bilateral aryepiglottic folds (white arrowhead), and vocal folds (white arrow). (c) Reformatted images of endoscopic view with left greater than right supraglottic obstruction (large white arrow). (d) Endoscopic images after emergent tracheostomy and 12 h of racemic epinephrine and Decadron still demonstrate significant edema through the supraglottic larynx and a curled “omega-shaped” epiglottis that collapses with inspiration (small white arrows).
VASCULAR
Venous occlusion/thrombus
As with most malignancies, HNC tumors exhibit a propensity for thrombogenicity. However, in contrast to most thrombogenic cancers that result in distant phlebitis or thromboembolism, HNC more commonly exerts local effects.[12] While it is poorly understood why HNC is associated with local rather than distant thrombosis, this phenomenon is well demonstrated in clinical practice. For example, head and neck tumors more commonly result in venous obstruction secondary to external compression of the internal jugular vein (IJV) due to SCC metastatic lymph nodes [Figure 5]. Moreover, when venous thrombosis arises, particularly involving the lower IJV at the neck base, it becomes, especially important for the radiologist to follow the venous system down toward the superior vena cava (SVC) to look for evidence of SVC syndrome or mediastinal tumor involvement.
- A 41-year-old woman with a history of metastatic melanoma status post-chemotherapy. (a) Sonography demonstrates a thrombus in the lower internal jugular vein (IJV), extending into the brachiocephalic vein. (b) Axial contrast-enhanced computed tomography image demonstrates a large necrotic lymph node (black arrow) compressing and nearly completely occluding the left IJV (black arrowhead).
Extratumoral extension into vascular structures can also result in a tumor thrombus precipitating vascular compromise, and this has been described in both the carotid artery and IJV.[13] Although infrequently seen with head and neck SCC, tumor thrombus has also been well described in the setting of differentiated thyroid cancer [Figure 6]. A key consideration in cases of suspected tumoral vascular invasion is utilizing the correct imaging modality. CT may provide high specificity, but there may be lower sensitivity when detecting vascular invasion, particularly when compared to other imaging modalities, such as ultrasound, which are readily available in the ED.[14]
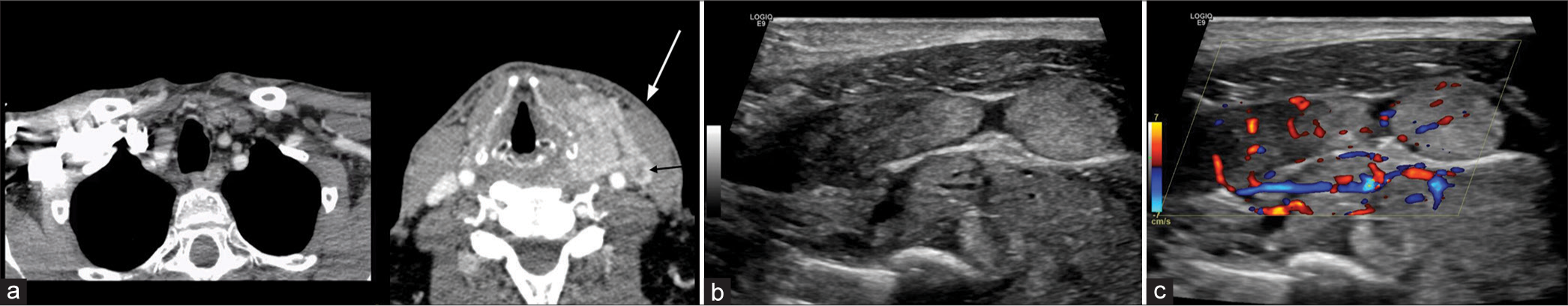
- A 58-year-old man with a history of metastatic renal cell carcinoma presenting with palpable nodular enlargement of the thyroid gland as well as a left neck mass. (a) Axial computed tomography images demonstrate multinodular enlargement of the thyroid gland with extracapsular extension on the left into the adjacent visceral space, suspicious for tumor extension into the left internal jugular vein (IJV) (tumor thrombus, white and black arrows). (b and c) Ultrasound performed demonstrates contiguous extension of tumor from the thyroid into the left IJV with color Doppler showing increased vascularity throughout the tumor thrombus.
Special considerations in post-treatment patients
Carotid blowout (CBO)
Common etiologies for CBO include radical resection, radiation necrosis, carotid exposure, wound infection, pharyngocutaneous fistula, and recurrent tumors. In addition, this can present after neck dissection (overall incidence of ~4.3%). While prior radiation has been shown to be an independent risk factor for CBO, overall risk has also been shown to increase substantially (7.6-fold) following neck dissection in patients with prior radiation.[15] CBO is classically divided into three categories: Threatened, impending, and acute.[16] Threatened CBO has imaging or clinical evidence of carotid at risk for rupture with the patient remaining asymptomatic. Common imaging findings include necrotic tissue/tumor adjacent to a vessel or the presence of a pharyngocutaneous fistula adjacent to a vessel. Impending CBO consists of transient bleeding that resolves spontaneously or with packing/pressure. Imaging may show a focal pseudoaneurysm without active bleeding or visible hematoma [Figure 7].[17] Acute CBO is the presence of uncontrollable hemorrhage requiring surgical/endovascular intervention. Imaging often shows active contrast extravasation at the site of vessel injury. Although the radiologist has a key role in the workup of all three types, identifying a threatened CBO can be the most beneficial as this diagnosis may preclude clinical suspicion.
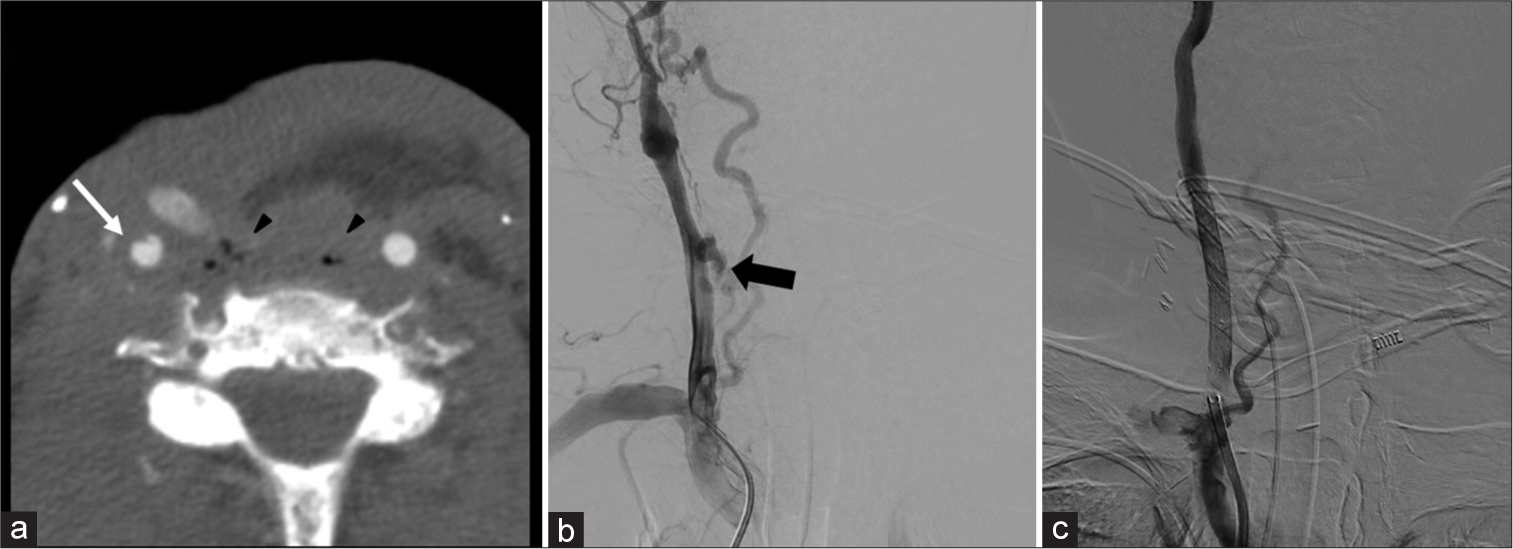
- A 72-year-old man with a history of laryngeal squamous cell cancer after chemoradiation who subsequently developed laryngeal recurrence now status post salvage laryngectomy, pharyngectomy, and partial glossectomy is presenting with balance issues and ear pain. (a) Axial computed tomography angiogram of the neck demonstrates focal dissecting pseudoaneurysm of the right common carotid artery (CCA) (white arrow) with adjacent soft-tissue gas/necrosis (black arrowhead). Soft-tissue findings alone warrant prompt notification by the radiologist as this finding represents a threatened blowout. In this instance, a dissecting pseudoaneurysm elevates this to an impending blowout. (b) Digital subtraction angiography (DSA) demonstrates clear active extravasation from mid-CCA, representing an acute carotid blowout requiring intervention (black arrow). (c) DSA post-treatment shows covered stent graft placement.
Carotid stenosis/occlusion
In the delayed phase, radiation increases the intima-media thickness and rapidly accelerates atherosclerosis,[18] which can result in progressive stenosis or thrombotic occlusion. Occlusion has been reported up to 10 years after treatment,[19] and can be seen in patients with no other concurrent risk factors.[20] In addition, adjacent soft-tissue radiation changes such as perivascular circumferential soft-tissue formation may provide subtle clues of this particular etiology. Figure 8 demonstrates progressive carotid artery occlusion in a patient following chemoradiation. Fortunately, this patient demonstrated reconstitution of flow at the cavernous segment of the internal carotid artery due to the formation of collaterals.
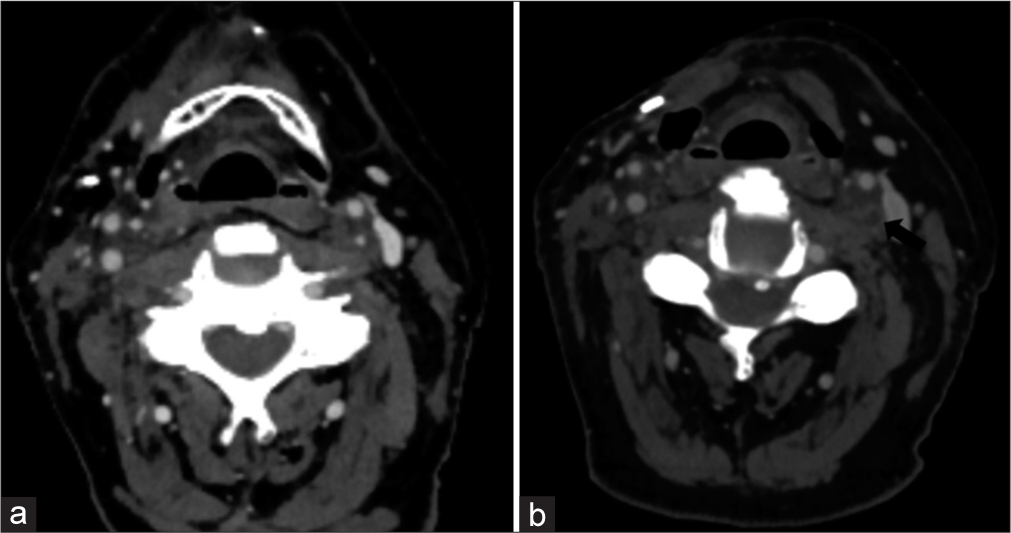
- A 77 year old male (a) Demonstrates atherosclerotic disease within the left internal carotid artery with a focal 60% stenosis of the proximal portion. (b) Demonstrates complete occlusion of the left internal carotid artery at this level approximately 1 year later. The images demonstrate the rapid rate of occlusive changes in patients with prior radiation. The patient received 60 Gy over 30 fractions to the right surgical bed and cervical lymph node levels I–V, as well as 52.5 Gy over 30 fractions to the left cervical lymph node levels II–IV.
ORBITAL
A commonly missed emergent complication of HNC on imaging is that of orbital compartment syndrome. This is a clinical diagnosis that occurs when there is a rise in orbital pressure (>20 mmHg) resulting in clinical signs of optic nerve ischemia. Symptoms such as enlarging blind spots, decreased color vision, and relative afferent pupillary defects are often clinically encountered. The low compliance of the rigid orbital walls results in low tolerance for optic nerve and retinal artery compression. The most common compressive etiologies include retrobulbar hemorrhage, infection, orbital emphysema, neoplasm, and recent surgery. Key radiographic findings include proptosis and tenting of the posterior globe resulting in a “guitar pick morphology”[21] [Figure 9]. Stretching of the optic nerve can also be a useful radiologic finding.[22]
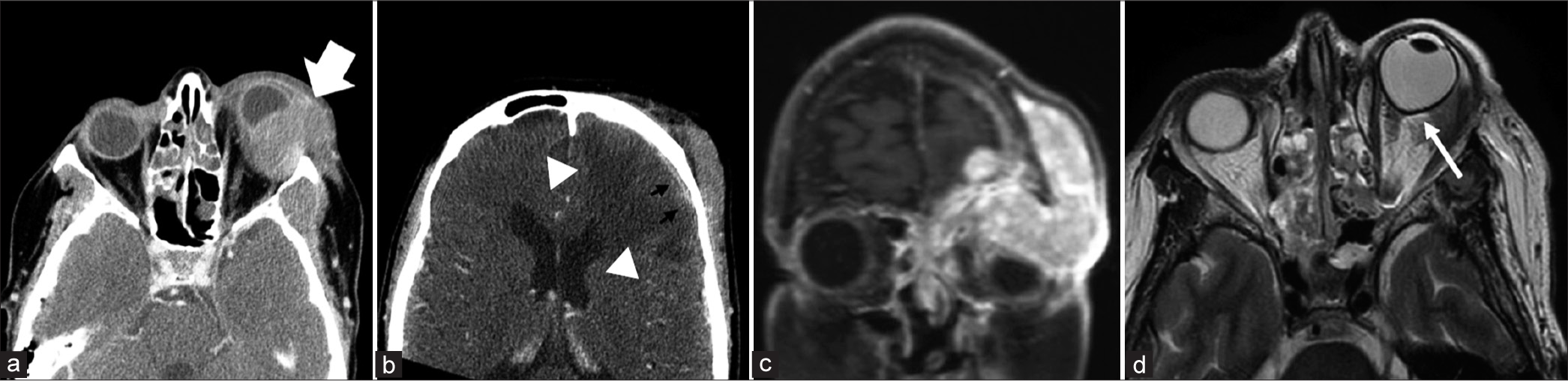
- A 64-year-old woman with several weeks of left eye swelling, pain, and drainage leading to concern for orbital cellulitis. (a) Axial contrast computed tomography demonstrates a large lobulated soft-tissue mass centered within the left orbit involving both pre-septal and post-septal soft tissues (white arrow). (b) Demonstrates extension along the left inferior anterior cranial fossa where there is dural-based enhancement (black arrowheads) and parenchymal edema (white arrowheads). (c) Coronal T1 post-contrast images demonstrate a large contrast-enhancing mass with a mass effect on the adjacent intraorbital space. (d) Axial T2 at the level of the globe demonstrates proptosis and tenting of the posterior globe resulting in a “guitar pick” sign (white arrow), indicating increased intraocular pressure.
CERVICAL SPINE
Discitis/osteomyelitis can be seen with dehiscence/breakdown of the pharynx or neopharynx. This is often seen after esophageal dilatation (a treatment for post-radiation upper esophageal strictures), likely as a result of bacterial translocation (Goldman et al., 2014). Key imaging findings include disc space fluid and adjacent vertebral body endplate erosion. Prevertebral or epidural phlegmon/abscess may also be present [Figure 10]. Identifying a site of possible pharyngeal dehiscence/breakdown is critical to guide clinical management. Of note, infectious discitis/osteomyelitis has a predilection for the avascular disc space before involving the vertebral body (unlike metastasis, which primarily involves the highly vascularized vertebral body). Figure 10 demonstrates two destructive C6 lesions; one lesion demonstrates an infectious etiology originating from the disc space and extending to the vertebral bodies, and the other demonstrates metastatic etiology, primarily encompassing the vertebral body.
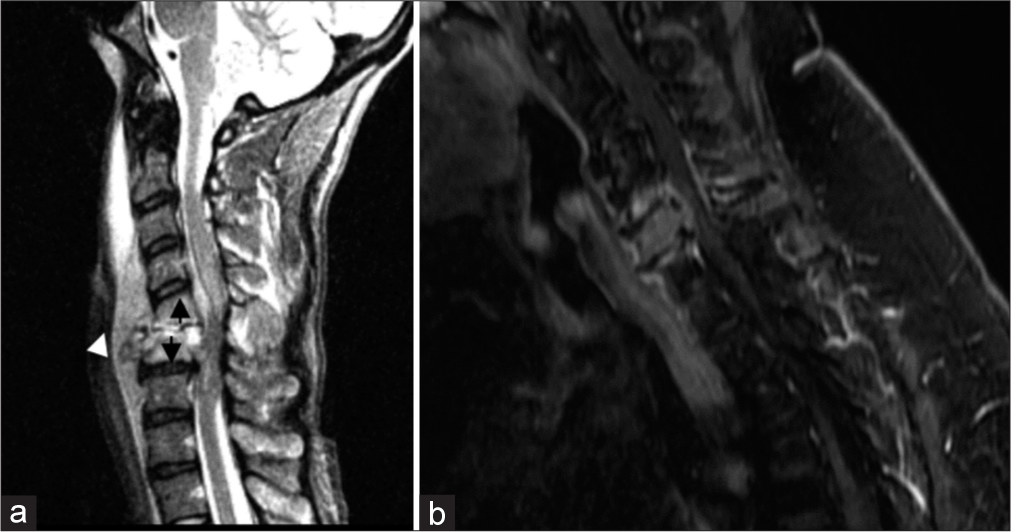
- A 38 year old female (a) Demonstrates the typical destruction pattern of osteomyelitis, which begins in the avascular disc space as can be seen by the complete collapse of the C5–6 disc space (white arrowhead). Furthermore, destructive changes and marrow edema are seen extending upward from the disc space (black arrows) most notably at the adjacent endplates. Prevertebral and ventral epidural fluids are also present. In contrast, (b) demonstrates a focal metastasis centered in the highly vascularized C6 vertebral body. The disc spaces are preserved and there is adjacent reactive endplate edema without erosion.
Special considerations in post-treatment patients
Osteoradionecrosis has been reported in the cervical spine following radiotherapy for HNC, of which nasopharyngeal carcinoma is most commonly described.[23] Common presenting symptoms include neck pain, kyphosis, paresthesia, discitis/osteomyelitis, fracture, and cord compression. This often has a subacute or chronic course, occurring between 4 and 48 months after treatment. Key imaging findings are similar to discitis/osteomyelitis, with mixed sclerotic-lucent appearance and bone destruction. Often confounded by secondary discitis/osteomyelitis, a subtle differentiating imaging feature can be the absence of fluid in the disc spaces. However, tissue sampling is often needed to exclude the presence of infection as findings can be nearly identical. Figure 11 demonstrates progressive cervical destruction at the C5–6 level in subsequent outpatient images. This patient was noted to have negative blood cultures and even demonstrated no culture growth on biopsy. The patient was later taken for cervical decompression and fusion due to concern for spinal instability. This case emphasizes how unrecognized cervical spine osteoradionecrosis can result in instability necessitating surgical fixation. In addition, magnetic resonance imaging demonstrates no fluid in the intervertebral disc spaces, which is not a specific finding but can support the diagnosis of osteoradionecrosis over osteomyelitis.
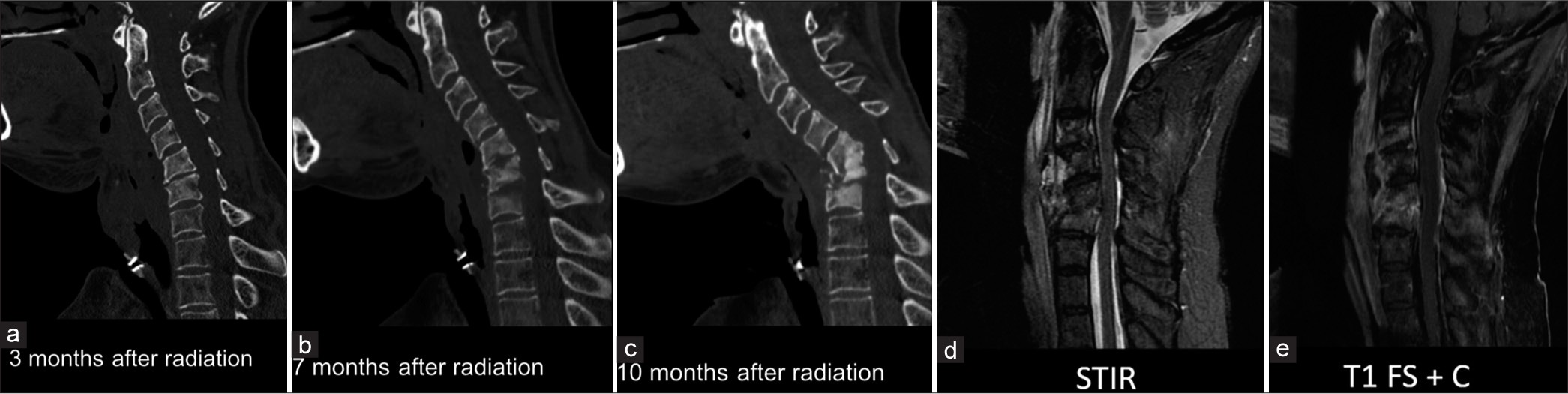
- A 56-year-old woman with a history of laryngeal cancer after total laryngectomy and adjuvant radiation completed 2 years prior presents with neck pain. (a-c) sagittal computed tomography neck in the bone window showing the progression of osteoradionecrosis 3, 7, and 10 months after radiation. (d and e) MRI images show heterogeneous short tau inversion recovery signal, a non-enhancing prevertebral collection spanning C4–C5, mixed sclerosis, and edema/enhancement with the C3–C5 vertebral body marrow. Notably, there is no fluid in the disc spaces, which would be more suggestive of infection.
CONCLUSION
Patients with HNC can present with uniquely challenging imaging features in the emergent setting. The difficulty in discerning the correct diagnosis arises from the complex head and neck anatomy, often compounded by advanced stage at presentation, poor overall functional status, and the potential for disastrous consequences in missed diagnoses. Radiologist familiarity with common HNC emergent presentations is essential for the accurate diagnosis of these patients; and radiologists are uniquely equipped to enable detection, ensuring prompt patient care.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Epidemiology and demographics of the head and neck cancer population. Oral Maxillofac Surg Clin North Am. 2018;30:381-95.
- [CrossRef] [PubMed] [Google Scholar]
- The rising incidence of major salivary gland cancer in the United States. Ear Nose Throat J. 2017;96:E13-6.
- [CrossRef] [PubMed] [Google Scholar]
- Why do head and neck cancer patients visit the emergency department? Am J Emerg Med. 2015;33:1102-5.
- [CrossRef] [PubMed] [Google Scholar]
- Intervals between symptom onset and clinical presentation in cancer patients. Intern Med. 2009;48:899-905.
- [CrossRef] [PubMed] [Google Scholar]
- Emergency presentations of head and neck cancer: A modern perspective. J Laryngol Otol. 2016;130:571-4.
- [CrossRef] [PubMed] [Google Scholar]
- Emergency department visits by head-and-neck cancer patients. Indian J Palliat Care. 2019;25:535-8.
- [CrossRef] [PubMed] [Google Scholar]
- Postoperative airway obstruction after airway tumor debulking. J Anesth. 2006;20:237-9.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging features of postradiotherapy changes in head and neck cancers. Indian J Radiol Imaging. 2021;31:661-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dosimetric predictors of laryngeal edema. Int J Radiat Oncol Biol Phys. 2007;68:741-9.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic laryngeal edema as a late reaction to radiochemotherapy. HNO. 1998;46:731-8.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed radionecrosis of the larynx. Am J Otolaryngol. 1999;20:245-9.
- [CrossRef] [PubMed] [Google Scholar]
- Thrombosis risk associated with head and neck cancer: A review. Int J Mol Sci. 2019;20:2838.
- [CrossRef] [PubMed] [Google Scholar]
- Pattern of tumor invasion, stromal inflammation, angiogenesis and vascular invasion in oral squamous cell carcinoma-A prognostic study. Curr Probl Cancer. 2021;45:100647.
- [CrossRef] [PubMed] [Google Scholar]
- Carotid artery and jugular vein invasion of oral-maxillofacial and neck malignant tumors: Diagnostic value of computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:368-72.
- [CrossRef] [PubMed] [Google Scholar]
- CT angiography findings in carotid blowout syndrome and its role as a predictor of 1-year survival. AJNR Am J Neuroradiol. 2014;35:562-7.
- [CrossRef] [PubMed] [Google Scholar]
- Endovascular therapy for the carotid blowout syndrome in head and neck surgical patients: Diagnostic and managerial considerations. AJNR Am J Neuroradiol. 1996;17:843-52.
- [Google Scholar]
- Carotid blowout syndrome: Modern trends in management. Cancer Manag Res. 2018;10:5617-28.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in the common carotid artery after radiotherapy: Wall thickness, calcification, and atherosclerosis. J Clin Neurol. 2018;14:35-42.
- [CrossRef] [PubMed] [Google Scholar]
- A case of occlusive radiation vasculopathy presenting as bilateral internal carotid artery, left middle cerebral artery occlusion and literature review. Case Rep Neurol. 2020;12:91-6.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanical thrombectomy and stenting for radiation-induced carotid stenosis-related stroke: A case report. Case Rep Neurol. 2020;12:70-5.
- [CrossRef] [PubMed] [Google Scholar]
- Radiology of abnormal globe contour. Clin Neuroradiol. 2021;31:943-51.
- [CrossRef] [PubMed] [Google Scholar]
- Optic nerve stretch in orbital compartment syndrome. Invest Ophthalmol Vis Sci. 2007;48:2482.
- [Google Scholar]
- Cervical spine complications after treatment of nasopharyngeal carcinoma. Eur Spine J. 2013;22:584-92.
- [CrossRef] [PubMed] [Google Scholar]







