Translate this page into:
The Effectiveness of Gelfoam as the Sole and Primary Embolization Agent in the Management of Hemoptysis: A Retrospective Study from a Tertiary Care Center

*Corresponding author: Abhinandan Ruge, Department of Radio Diagnosis, St. John’s Medical College Hospital, Bengaluru, Karnataka, India. abhiruge@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Ruge A, Kumar N, Menezes C. The effectiveness of Gelfoam as the sole and primary embolization agent in the management of hemoptysis: A retrospective study from a Tertiary Care Center. J Clin Imaging Sci 2021;11:10.
Abstract
Objectives:
The objective of this study was to evaluate the role of Gelfoam as an effective embolizing agent in patients with hemoptysis presenting to a tertiary care center in developing nations.
Material and Methods:
A retrospective analysis of data from 30 patients treated by Interventional radiologist at St. John’s Medical College, Bangalore, India, was performed. The study included 22 males (73.3%) and 8 (26.65%) female patients. Gelfoam was used as the sole embolizing agent and arteries with features of abnormal blush and hypertrophy were targeted. Analysis of the etiology, immediate, and short-term outcome and complications, when present, was performed. The median follow-up period was 45 days following an embolization procedure at this center.
Results:
A high short-term efficacy was noted following embolization procedures with Gelfoam as the sole agent. Twenty-eight out of 30 procedures were deemed successful, and post-tubercular changes were noted to be the cause for hemoptysis in 23 patients. The high short-term efficacy (93.3%), evidenced by a complete stoppage of hemoptysis, along with a relatively low rate of complications (spinal cord ischemia in only 2.3%), strengthens the position of Gelfoam as the sole embolizing agent in a resource-limited setting.
Conclusion:
In an economically constrained setting, Gelfoam proves to be a useful first choice single embolization agent, while polyvinyl alcohol particles coupled with microcatheter systems remain within reach of only those who can afford them.
Keywords
Gelfoam
Embolization
Radiological intervention and microcatheter
INTRODUCTION
Coughing up of blood is a dramatic symptom of lung disease when present clinically, its seriousness compounded by the nature of the underlying pathology causing it. Hemoptysis is the expectoration of blood from the airways or lung parenchyma below the level of the glottis.[1,2] While several disease conditions have been listed as being capable of causing hemoptysis – pneumonia, inflammation in the lower respiratory system, chronic obstructive pulmonary disease, bronchiectasis, cystic fibrosis and neoplasia in the respiratory tree, and tuberculosis and its sequelae emerge as the leading cause for hemoptysis in resource-limited settings like India.[1-4] Percutaneous transthoracic needle biopsies of lung masses have also been associated with hemoptysis as a procedure-related complication.[5] In a case report, pulmonary actinomycosis has been documented as a cause for recurrent hemoptysis,[6] while fistulous communication between the aorta and tracheobronchial tree can also result in large volume, life-threatening hemoptysis.[7] Hemoptysis is termed life-threatening when the volume of blood is clinically large enough to bring about respiratory compromise. An 80% mortality rate is associated with life-threatening hemoptysis related mainly to asphyxiation.[8]
Diagnosing the source of bleeding
Hemoptysis most commonly occurs from the bronchial artery and its branches with non-bronchial systemic (NBS) arteries being involved mainly by tubercular etiology.[9,10] Multidetector computed tomography (CT) enabled CT angiography is the imaging modality preferred for the diagnosis of hemoptysis. It enables relatively accurate localization of the source of hemorrhage – bronchial or NBS vessels, provides information about the number and origin of the arteries, and also allows evaluation of the etiology of hemoptysis.[11,12]
Embolization and embolizing agents
Bronchial or NBS vessel embolization has become a safe and effective method in tackling potentially catastrophic hemorrhage in addition to negotiating the morbidity associated with open surgical procedures to check hemorrhage.[11-14] The embolization of the bleeding vessel is carried out by first obtaining access into the arterial system through the femoral artery. Usually, 5 Fr sheath is commonly used through which either Cobra or Simmons catheters were used. The bronchial arteries are cannulated, and a selective arteriogram (ideally digital subtraction angiography) is then performed.[15] Low to iso-osmolar non-ionic contrast agents are preferred as ionic agents are associated with a higher incidence of transverse myelitis.[14]
Vascular hypertrophy and tortuosity, hypervascularity, aneurysm formation, neovascularity, and shunting (bronchial artery to the pulmonary vein or bronchial artery to pulmonary artery) seen on initial arteriography indicate the source of bleeding. These initial angiographic runs can be used as roadmaps during definitive embolization later. It is essential to identify the artery of Adamkiewicz (with its typical hairpin configuration), when present, as accidental blockage of the artery results in catastrophic neurological deficits.[14,15]
A variety of embolization agents are available – polyvinyl alcohol (PVA) (PVA particle with diameters ranging from 250 to 500 microns), microspheres (500–700 microns), n-butyl-2-cyanoacrylate, ethylene vinyl alcohol polymer, Gelfoam, and Gelfoam in combination with micro coils.[14-19] Superselective embolization is carried out using microcatheters passed into the larger catheter in a coaxial fashion.
MATERIAL AND METHODS
Embolization using Gelfoam-experiences at this center
A trained interventional radiologist performed all embolization procedures in the hospital catheterization laboratory. Arterial access was gained through a femoral puncture. Preliminary descending thoracic aortogram provided useful information regarding bronchial artery origins and anatomy. The cobra-type curved catheters/ Simmons catheters were used for selective catheterization of the bronchial artery.
Once the bronchial artery was selectively catheterized, an angiogram was performed, which enabled the detection of the bleeding vessel and localization of the artery of Adamkiewicz. Digital subtraction images were obtained after the injection of iodinated contrast. Abnormal vascularity was identified in the form of the presence of hypertrophied vessels, abnormal vascular blush, areas of arteriovenous shunting, and foci of active extravasation.
Gelfoam powder was mixed with dilute iodinated contrast and injected as a slurry without the need for a microcatheter. The commonly embolized arteries included the bronchial arteries, intercostal arteries, and lateral thoracic artery branches. Embolization was discontinued with early signs of reflux or stasis. All the patients were then observed in a surgical or respiratory care unit for a minimum period of 24– 48 h for immediate control of the bleeding post-procedure and recurrence or any complication.
RESULTS
On immediate follow-up (within 48 h post-procedure), total cessation of hemoptysis was achieved in 27 patients. Partial response with regression in hemoptysis was noted in 3 patients, which slowly improved with medical management [Table 1]. A single major complication was noted, where a patient developed paraparesis following the interventional procedure due to spinal cord ischemia. Care had been taken to avoid the artery Adamkiewicz and the other spinal arteries; however, spinal ischemia could have been caused by the opening of the spinal collateral during the process of embolization. The weakness, however, was transient, and the patient gradually improved with physiotherapy and medical management and regained Grade 4 power around 3 weeks after the procedure. Other minor complications noted were chest discomfort (12) and puncture site hematoma (1).
Repeat bronchial artery embolization (BAE) was required in one patient due to the opening of a prominent feeder, leading to recurrence of significant hemoptysis (this occurred 2 weeks following the procedure) [Figure 1]. It was necessary to undertake a second embolization procedure for the patient; embolization was carried out using PVA particles with no further episodes of bleeding following the second procedure.
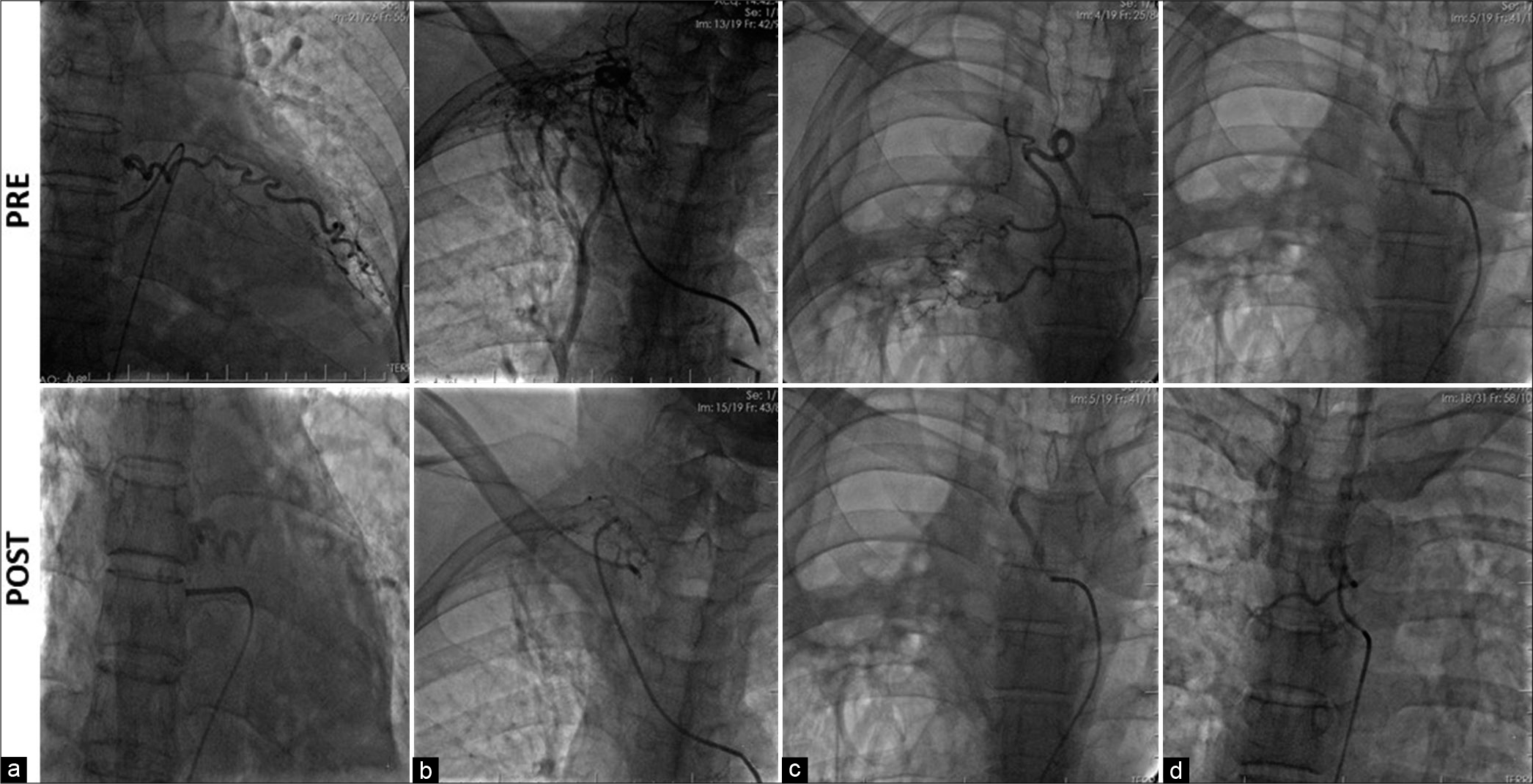
- (a-d) Selective bronchial artery angiograms showing a dilated right bronchial artery with abnormal hypervascularity and tortuosity.
DISCUSSION
Near-complete control of hemoptysis was achieved in 27 patients (90%) following BAE. We compared our data with other prominently cited published literature regarding the BAE with gel foam that focused on the immediate bleeding control rate. The immediate success rates were lower up to the year 2000 (generally <90%). Higher success rates following this could be attributed to newer advances in medical therapy and the availability of better catheter and the cath-lab systems.
The complication rates, as seen in these studies, have generally shown a declining trend over the years.[20-22] Our study had one major complication in the form of spinal cord ischemia leading to transient paraparesis. Other minor complications were chest discomfort and puncture site hematoma. Repeat BAE was required in a patient due to the opening up of a prominent feeder, leading to recurrence of significant bleed 2 weeks following the procedure. Overall, these results show an excellent safety profile of the procedure with a low incidence of clinically significant complications.
Limitations
The present study was a retrospective one from a single center with follow-up carried out for a maximum period of only 3 months.
CONCLUSION
The study reiterates BAE to be an effective technique to control acute, life-threatening hemoptysis. Previous studies have concluded that PVA is preferred over Gelfoam, with Gelfoam even being recommended as a supplementary agent following embolization with PVA due to its temporary occlusive effect. It is imperative still to note that the requirement of a microcatheter system for use with PVA particles coupled with the higher cost of the particles itself raises the financial burden of an embolization procedure. Considering the majority of patients with hemoptysis due to tuberculosis belong to lower strata of society, and expensive embolization procedures may not be within reach of those in greatest need. With a high percentage of complete occlusion of target vessels following initial embolization and low risk of major complications resulting from non-target embolization, as noted in this study, Gelfoam may even be considered as a sole and primary embolization agent in developing nations like India where embolization with PVA particles or embospheres is still reserved for the privileged.
References
- Antifibrinolytic therapy to reduce haemoptysis from any cause. Cochrane Database Syst Rev. 2016;11:CD008711.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and treatment of hemoptysis. Arch Bronconeumol. 2016;52:368-77.
- [CrossRef] [PubMed] [Google Scholar]
- Bronchial artery embolization in treatment of hemoptysis: Treatment efficacy and complications at a tertiary care chest centre. Med J Armed Forces India. 2018;74:352-7.
- [CrossRef] [PubMed] [Google Scholar]
- Bronchovascular injury associated with clinically significant hemoptysis after CT-guided core biopsy of the lung: Radiologic and histopathologic analysis. PLoS One. 2018;13:e0204064.
- [CrossRef] [PubMed] [Google Scholar]
- A case of recurrent hemoptysis caused by pulmonary actinomycosis diagnosed using transbronchial lung biopsy after bronchial artery embolism and a brief review of the literature. Ann Transl Med. 2019;7:108.
- [CrossRef] [PubMed] [Google Scholar]
- Fistulas between the aorta and tracheobronchial tree. Ann Thorac Surg. 1991;51:515-9.
- [CrossRef] [Google Scholar]
- 64-detector row CT evaluation of bronchial and non-bronchial systemic arteries in life-threatening haemoptysis. Br J Radiol. 2012;85:e666-72.
- [CrossRef] [PubMed] [Google Scholar]
- Are there Predictors of Embolization in Patients with Hemoptysis? European Congress of Radiology.
- [Google Scholar]
- Haemoptysis due to chronic tuberculosis vs. bronchiectasis: Comparison of long-term outcome of arterial embolisation. Int J Tuberc Lung Dis. 2007;11:781-7.
- [Google Scholar]
- Radiologic management of haemoptysis: Diagnostic and interventional bronchial arterial embolisation. Rofo. 2015;187:248-59.
- [CrossRef] [PubMed] [Google Scholar]
- Value of multidetector computed tomography angiography before bronchial artery embolization in hemoptysis management and early recurrence prediction: A prospective study. BMC Pulm Med. 2020;20:1-0.
- [CrossRef] [PubMed] [Google Scholar]
- Bronchial artery embolization: First-line option for managing massive hemoptysis. Asian Cardiovasc Thorac Ann. 2017;25:618-22.
- [CrossRef] [PubMed] [Google Scholar]
- Bronchial artery embolization for hemoptysis. Semin Intervent Radiol. 2011;28:48-62.
- [CrossRef] [PubMed] [Google Scholar]
- Bronchial artery embolization. Semin Intervent Radiol. 2004;21:43-8.
- [CrossRef] [PubMed] [Google Scholar]
- Bronchial artery embolization for hemoptysis in primary lung cancer: A retrospective review of 84 patients. J Vasc Interv Radiol. 2019;30:428-34.
- [CrossRef] [PubMed] [Google Scholar]
- Bronchial artery embolotherapy for control of acute hemoptysis: Analysis of outcome. Chest. 1999;115:912-5.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of hemoptysis by embolization of bronchial arteries. Radiology. 1977;122:33-7.
- [CrossRef] [PubMed] [Google Scholar]
- Massive hemoptysis due to pulmonary tuberculosis: Control with bronchial artery embolization. Radiology. 1996;200:691-4.
- [CrossRef] [PubMed] [Google Scholar]
- Bronchial arteriography and transcatheter embolization in management of severe haemoptysis. Med J Armed Forces India. 1999;55:189-92.
- [CrossRef] [Google Scholar]
- Comparison of the effectiveness of embolic agents for bronchial artery embolization: Gelfoam versus polyvinyl alcohol. Korean J Radiol. 2010;11:542-6.
- [CrossRef] [PubMed] [Google Scholar]
- Embolic agents used for bronchial artery embolisation in massive haemoptysis. Expert Opin Pharmacother. 2004;5:361-7.
- [CrossRef] [PubMed] [Google Scholar]







