Testicular Ischemia Due to a Band Around the Spermatic Cord
Address for correspondence: Dr. Suheil Artul, Department of Radiology, Nazareth Hospital, EMMS, Nazareth, Israel. E-mail: suheil_artul@hotmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We present a case of an 18-year-old boy who was admitted to our hospital with a 2-day history of pain in the right scrotum. Ultrasound examination showed signs of ischemia, with dampened testicular arterial flow and bell-clapper deformity. Surgery revealed a constricting fibrous band around the distal spermatic cord resembling the bell-clapper deformity.
Keywords
Band
bell-clapper deformity
ischemia
testis
ultrasound
Color Flow Doppler
INTRODUCTION
Testicular torsion is a surigical emergency. It results from spermatic cord twisting, affecting the blood flow, and ultimately causing ischemia of the testicle. It can occur at any age, but commonly affects boys and young men, with an incidence of 1/4000 in males younger than 25 years. Testicular torsion that is associated with the so-called bell-clapper deformity accounts for 90% of all cases of testicular torsion.[12]
CASE REPORT
An 18-year-old young man was admitted to our hospital due to aggravating pain in the right hemiscrotum that had continued over 2 days. Eight years earlier, he had suffered from right epididymitis that was successfully treated with antibiotics. On presentation, there was no fever or history of trauma. On physical examination, he had an enlarged painful right testis and absent cremasteric reflex.
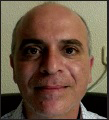
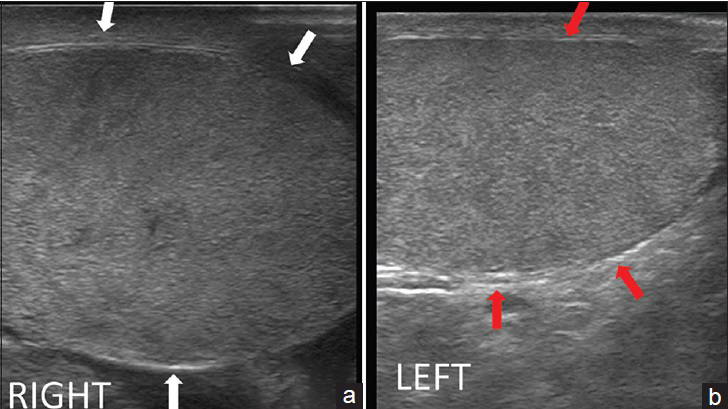
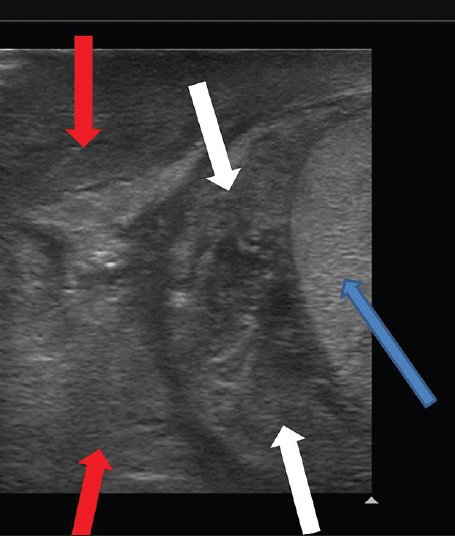
Gray scale ultrasound (US) of the scrotum showed hypoechoic and enlarged right testis [Figure 1], enlarged right epididymis [Figure 2], and normal left testis. Color spectral Doppler US of the right testis showed monophasic arterial dampened blood flow [Figure 3] and decreased flow in the epididymis, suggesting the diagnosis of right incomplete testicular torsion.
- 18-year-old man presented to emergency room with acute right testicular pain diagnosed as caused by a fibrous constricting band around the spermatic cord. (a and b) Gray scale longitudinal ultrasound of the right testis show a enlarged, hypoechoic, edematous right testis (between white arrows), and a normal left testis (between red arrows).
- 18-year-old man presented to emergency room with acute right testicular pain diagnosed as caused by a constricting fibrous band around the spermatic cord. Gray scale ultrasound longitudinal view demonstrates right testis (blue arrow), enlarged right epididymis (white arrows) and spermatic cord (red arrows).
- 18-year-old man presented to emergency room with acute right testicular pain diagnosed as caused by a constricting fibrous band around the spermatic cord. Color flow spectral Doppler of the right testis demonstrates dampened arterial waveform with decreased diastolic blood flow.
Intratesticular monophasic dampened arterial flow pattern suggests significant resistance to arterial inflow.
At surgery, there were signs of ischemia of the right testis without testicular torsion and, surprisingly, a fibrous constricting band was found around the distal spermatic cord, which was released and the testis regained its normal appearance and blood flow. No bell-clapper deformity was found.
DISCUSSION
Acute scrotum is defined as a sudden painful swelling of the scrotum or its contents, accompanied by local signs or systemic symptoms such as nausea and vomiting. In a patient presenting with acute scrotum, it is imperative to rule out testicular torsion, which is a true surgical emergency.[12345]
Generally on physical examination, the hallmark of testicular torsion is a “high riding” testis due to shortening of the spermatic cord. Absence of the cremasteric reflex is characteristic of testicular torsion in the pediatric population. A normal cremasteric reflex would result in elevation of the ipsilateral testis after a gentle stroke of the inner thigh. The cremasteric reflex is rarely seen in patients with testicular torsion.[6789]
The differential diagnosis of acute scrotum includes a variety of conditions such as torsion of the spermatic cord, orchitis, epididymitis, idiopathic scrotal edema, hematoma or bleeding due to trauma, strangulated hernia, and segmental testicular infarction.[456]
Other clinical and sonographic differential diagnoses include Henoch–Schonlein purpura, testicular tumors, and lower back strain. Henoch–Schonlein purpura is a systemic vasculitis that typically affects patients younger than 20 years and has a peak incidence at 4–5 years of age. It involves the scrotum in 2–38% of the cases and should not be confused with testicular torsion. Characteristic US findings include severe edema of the scrotal skin and contents with intact vascular flow in the testicle, epididymal enlargement, and a hydrocele, which help to distinguish this from testicular torsion and prevent unnecessary surgery.
Lower back strain is a diagnosis of exclusion and must be considered after ruling out all other causes of scrotal pain. Lower back strain can be secondary to radiculitis at T10 to L1, causing nerve root irritation and subsequent referred scrotal pain.[789]
The most urgent of these conditions is testicular torsion or ischemia. Immediate causes of testicular torsion are thought to occur several hours after vigorous activity, a minor injury to the testicles, or sleep. Cold temperature or rapid growth of the testicle during puberty might also play a role.
Gray scale ultrasound signs such as hypoechogenicity and enlarged testis are not specific for torsion. On the other hand, the role of color Flow Doppler and power Doppler US in the diagnosis of acute testicular torsion in questioned clinical cases is well established with a sensitivity and specificity of 96.8% and 97.9%, respectively.[2378]
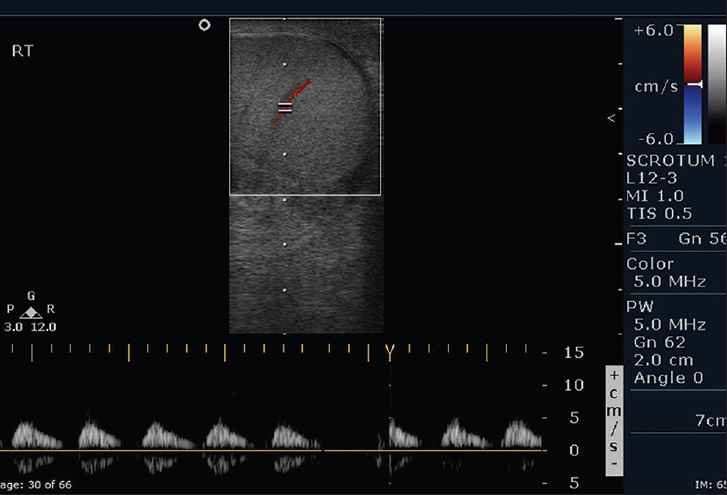
We present the first case report of testicular ischemia caused by a fibrous band around the spermatic cord that was identified on US. We do not know if the band evolved as a sequel of the patient's previous epididymitis 8-years earlier or a rare congenital anomaly. Unfortunately, the surgeon only released the band; hence, no tissue sample was sent for pathological investigations. Re-evaluating the US, we clearly detected the band around the distal cord [Figure 4].
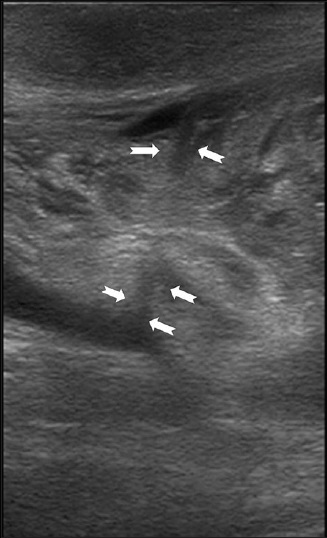
- 18-year-old man presented to emergency room with acute right testicular pain diagnosed as caused by a constricting fibrous band around the spermatic cord. Gray-scale ultrasound of the right hemiscrotum demonstrates a hypoechoic band like structure constricting the distal spermatic cord (between white arrows).
There are two categories of testicular torsions: Intra-vaginal and extra-vaginal. Intra-vaginal torsion is the most common type and is the type commonly found in older children and adults. In fact, this type occurs in patients between 3 and 20 years of age. It is generally associated with a pre-existing anomaly of fixation of the testis, termed “bell-clapper” deformity. Here, the intrascrotal portion of the spermatic cord lacks posterior adhesion to the scrotum and remains surrounded by the tunica vaginalis, predisposing rotation of the testis and cord. This situation allows the testes to swing freely and rotate within the tunica vaginalis like a “clapper inside” a bell.[2345]
Extra-vaginal torsion is a different entity, in which both the contents of the tunica and the tunica itself rotate, and is seen mainly in neonates. This condition is caused by impaired attachments of the tunica to the scrotal wall. As the child grows, the tunical attachments strengthen, lessening the likelihood of this type of torsion after the neonatal period.[78910]
CONCLUSION
Fibrous constricting bands around the epididymis are very rare. The origin of this constricting fibrous band is not known. It may be related to prior incidence of epididymitis as stated in our case or may be of congenital origin. Ultrasound can identify this band and in every case of testicular torsion an attempt should be made to look for such an entity.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/36/157856
Financial support and sponsorship: Nil
Conflict of interest: There are no conflict of interest.
REFERENCES
- Sonographic diagnosis of superior hemispheric testicular infarction. AJR Am J Roentgenol. 2002;179:775-6.
- [Google Scholar]
- Benign intratesticular cystic lesions: US features. Radiographics. 2001;21:S273-81.
- [Google Scholar]
- Retrospective review of diagnosis and treatment in children presenting to the pediatric department with acute scrotum. AJR Am J Rentgenol. 2013;200:W444-9.
- [Google Scholar]
- Anatomic aspects of epididymis and tunica vaginalis in patients with testicular torsion. Int Braz J Urol. 2004;30:420-4.
- [Google Scholar]
- Pack of ice: Grey scale sign of testicular torsion. BMJ Case Rep 2014 2014 pii: bcr2013202734
- [Google Scholar]
- Scrotal ultrasonography in Henoch-Schönlein purpura. Pediatr Radiol. 1992;22:505-6.
- [Google Scholar]
- Surgery of the scrotum and testis in children. In: Walsh PC, Retnick AB, Vaughan ED Jr, Wein AJ, eds. Campbell's Urology (7th ed). Philadelphia: Saunders; 1998. p. :2193-209.
- [Google Scholar]






