Translate this page into:
Supraspinatus fatty infiltration on MRI among older adults receiving physical therapy as initial management for clinically suspected rotator cuff tear: A pilot study

*Corresponding author: Derik L. Davis, Department of Diagnostic Radiology and Nuclear Medicine, University of Maryland School of Medicine, Baltimore, Maryland, United States. ddavis7@umm.edu
-
Received: ,
Accepted: ,
How to cite this article: Davis DL, Almardawi R, Awan OA, Lo LY, Ahmed SR, Jubouri S, et al. Supraspinatus fatty infiltration on MRI among older adults receiving physical therapy as initial management for clinically suspected rotator cuff tear: A pilot study. J Clin Imaging Sci 2022;12:66.
Abstract
Objectives:
Rotator cuff (RC) tear is common among adults ≥60 years, with supraspinatus tear most common. Intramuscular fatty infiltration (FI) on imaging is predictive of long-term outcomes following RC tear. Physical therapists routinely diagnose RC tear only by clinical examination since most do not order imaging studies. Thus, there is limited knowledge about FI in older populations receiving physical therapy (PT) for initial management of RC tear. The primary objective of our pilot study is to determine longitudinal differences in supraspinatus FI over time among older adults receiving PT (PT cohort) for initial management of RC tear relative to older adult volunteers (control cohort), and with secondary objective to evaluate longitudinal self-reported shoulder function over time.
Material and Methods:
This was a prospective longitudinal cohort study. Forty adults, 60–85 years, were enrolled at baseline; one follow-up visit at ≥6 months. Shoulder magnetic resonance imaging and clinical screening for Charlson comorbidity index (CCI), body mass index (BMI), and American Shoulder and Elbow Surgeon (ASES) score were completed at baseline and follow-up visits. Supraspinatus FI was evaluated by 6-point Dixon fat fraction and Goutallier grade. PT (n = 15) and control (n = 25) cohorts were stratified by supraspinatus status: Intact (no tear), partial-thickness tear (PTT), and full-thickness tear (FTT). Comparisons within cohort were performed by Kruskal–Wallis test and between cohorts by Mann–Whitney U-test. Interobserver reliability was performed for Dixon fat fraction and Goutallier grade.
Results:
PT cohort at baseline showed no difference for age, BMI, CCI, and ASES score; supraspinatus FI was highest for FTT by Goutallier grade (no tear, 0.5 ± 0.5; PTT, 1.1 ± 0.2; and FTT, 1.5 ± 0.5; P = 0.033) and by Dixon fat fraction (no tear, 4.6% ± 1.4%; PTT, 6.1% ± 1.9%; and FTT, 6.7% ± 2.5%; P = 0.430). Control cohort at baseline showed no difference for age, BMI, CCI, and ASES score; supraspinatus FI was highest for supraspinatus FTT by Dixon fat fraction (no tear, 5.8% ± 1.2%; PTT, 7.1% ± 6.3%; and FTT, 21.4% ± 10.4%; P = 0.034) and by Goutallier grade (no tear, 0.8 ± 0.5; PTT, 1.0 ± 0.6; and FTT, 2.4 ± 1.7; P = 0.141). No difference between similar PT and control cohort subgroups at baseline except no tear groups for ASES score (PT cohort, 58.9 ± 8.2; control cohort, 84.0 ± 21.9; P = 0.049). No differences were identified for Δ-Dixon fat fraction and Δ-Goutallier grade over time in the PT and control cohorts. PT cohort no tear subgroup showed significant improvement (P = 0.042) for Δ-ASES score over time relative to PTT and FTT subgroups; no difference for Δ-ASES score over time in the control cohort.
Conclusion:
Full-thickness RC tear showed higher levels of FI relative to PTT or no tear at baseline. Our pilot study’s trend suggested that older adults receiving PT for initial management of RC tear have full-thickness RC tear for shorter duration based on relative lower levels of FI at baseline as compared to older adult volunteers with full-thickness RC tear. Our pilot study also found that older adults in the PT cohort with no tear had superior shoulder functional recovery by ASES score over time relative to full-thickness and PTTs.
Keywords
Intramuscular fatty infiltration
Magnetic resonance imaging
Physical therapy
Rotator cuff
Shoulder
INTRODUCTION
Rotator cuff (RC) tear negatively impacts shoulder function in older populations. The prevalence of RC tear is as high as one in four among adults aged 60 years and older, with supraspinatus tear the most common subtype.[1-3] Investigators estimate that adults aged 65–74 years have the highest rate of surgical rotator cuff repair (RCR) utilization in the United States, at an annual rate of 28.3/10,000 persons.[4] Best practices for clinical decision making remain controversial, as orthopedic surgeons consider several patient-specific factors when determining if RCR surgery is indicated.[5-8] However, the current standards of care establish that cross-sectional imaging is a key component in orthopedic surgeons’ decision-making process, with magnetic resonance imaging (MRI) a leading modality in the Unites States. Shoulder MRI is valid and reliable for characterizing RC tear and degree of intramuscular fatty infiltration (FI).[5,9-12] High level of FI is considered a relative contraindication for RCR surgery due to increased risk of poor post-surgical outcomes.[5,12-14]
Management of RC tear in older populations is controversial. Non-operative physical therapy (PT) is currently in a state of equipoise with RCR surgery.[7,15,16] Given this fact, physical therapists routinely evaluate older adults following referral from primary care providers, or by patients’ self-referral, and provide initial management for shoulder dysfunction.[17,18] Physical therapists typically diagnosis RC tear based on clinical examination alone, since most physical therapists do not order imaging studies for their patients.[19,20] Thus, in contrast to patients receiving care from orthopedic surgeons, there is a current gap in knowledge about levels of FI and progression of FI over time in the population of patients receiving initial management for RC tear by physical therapists.
The primary objective of our pilot study is to determine differences in levels of supraspinatus FI, and change in supraspinatus FI over time, in cohorts of older adults receiving PT (PT cohort) for initial management of presumptive RC tear and older adult volunteers (control cohort). We hypothesize that participants with full-thickness supraspinatus tear will demonstrate the highest level of supraspinatus FI at baseline and highest change in supraspinatus FI over time as compared to participants with partial-thickness tear (PTT) or no tear. Supraspinatus FI will be measured both by quantitative Dixon fat fraction and by semi-quantitative Goutallier grade. The secondary objective is to evaluate differences in self-reported shoulder function by the American Shoulder and Elbow Surgeon (ASES) score at baseline, and change in ASES score over time, among subgroups of the PT and control cohorts.
MATERIAL AND METHODS
Study population
This study was approved by the Institutional Review Board of the University of Maryland Baltimore and complied with the Health Insurance Portability and Accountability Act guidelines. Informed written consent was obtained from each participant included in the prospective longitudinal cohort study. The study population included older adults recruited as a convenience sample through advertisement during a 1-year period between February 2019 and February 2020 in an area local to Baltimore, Maryland. The study consisted of two cohorts: A usual care PT cohort and a control cohort. The inclusion criteria for the PT cohort included adults, aged 60–85 years, receiving self-reported usual care shoulder rehabilitation within ≤4 months before enrollment at baseline as primary treatment for a presumptive RC tear based on clinical grounds by their shoulder rehabilitation specialist. Inclusion criteria for the control cohort included adults, aged 60–85 years, not participating in a shoulder rehabilitation program. The exclusion criteria for both cohorts included contraindication to MRI; history of prior RC repair or joint replacement for ipsilateral shoulder; active worker’s compensation claim; ipsilateral upper extremity paralysis; fracture of ipsilateral humerus, clavicle, or scapula in the prior 12 months; and known malignancy involving ipsilateral shoulder. A total of 40 participants were included in the analysis at baseline, with 15 and 25 participants in the PT and control cohorts, respectively [Figure 1].
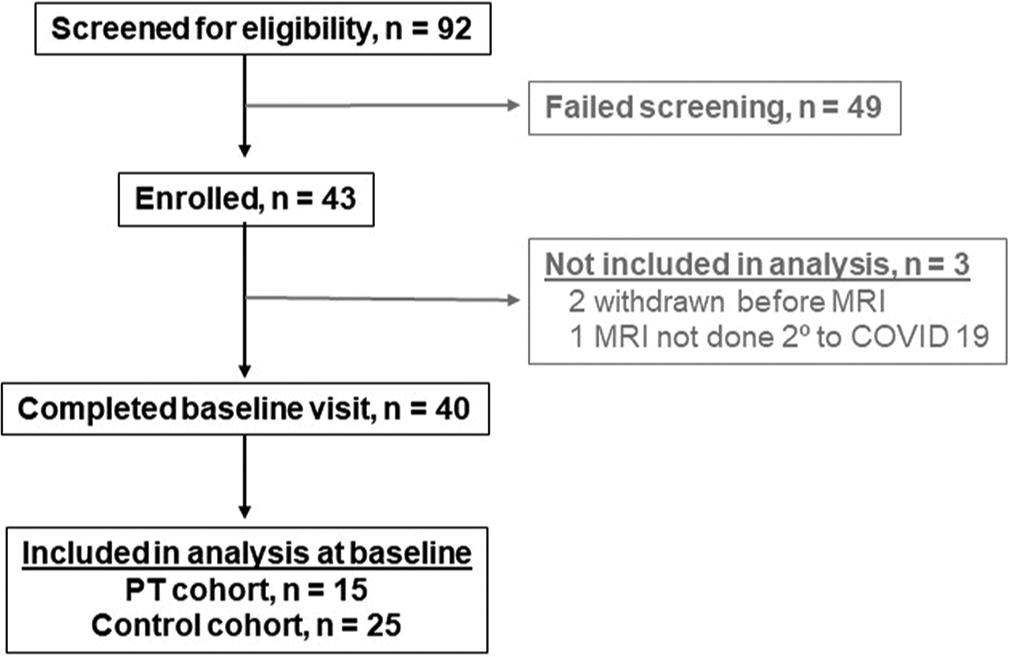
- STROBE diagram.
MRI
Shoulder MRI examinations were performed at 3.0 T (Magnetom Prisma fit, Siemens Healthineers, Erlangen, Germany) using a 4-channel flexible coil, at our institution’s MRI research center. The protocol included a two-dimensional (2D) spin-echo oblique sagittal T1-weighted sequence (matrix, 448 × 202; repetition time ms (TR)/echo time[s] (TE) ms, 600/24; field of view (FOV), 160 × 160 mm2; slice thickness, 4 mm; number of averages, 1). Furthermore, 2D short-tau inversion recovery sequences were acquired in the oblique sagittal, oblique coronal, and axial planes (matrix, 256 × 205; TR/TE ms, 4420/51; inversion time 180 ms; FOV, 160 × 160 mm2; slice thickness, 4 mm; number of acquisitions, 1). A three-dimensional 6-point Dixon sequence was obtained in the sagittal orientation (matrix, 320 × 320; TR, 9.31 ms, TE,1.35, 2.65, 3.95, 5.25, 6.55, 7.85 ms; flip angle, 9; FOV 400 × 312 mm2; slice thickness, 3.5 mm; number of averages, 1). Furthermore, 6-point Dixon fat fraction maps were reconstructed in the oblique sagittal plane in an automated fashion. All study participants received shoulder MRI at the baseline visit. The second follow-up shoulder MRI visit took place ≥6 months following the baseline visit.
MRI analysis
One blinded musculoskeletal radiology fellow and one blinded senior diagnostic radiology resident independently evaluated DICOM image modules that contained the single de-identified oblique sagittal 6-point Dixon fat fraction map MR image for each participant corresponding to the Y-shaped view, the most lateral slice where the scapular body contacts the spine.[21-24] Each blinded rater independently measured quantitative Dixon fat fraction of the supraspinatus muscle by manual placement of a region of interest (ROI) using Medical Image Processing, Analysis and Visualization software (MIPAV, version 8, National Institutes of Health, Bethesda, Maryland). The ROI was placed at the inner margin of the supraspinatus muscle, avoiding inclusion of the adjacent perimuscular fat or bone [Figure 2a and c]. The mean Dixon fat fraction value between raters for the supraspinatus muscle for each participant was used for analysis.

- Example images for the measurement of supraspinatus intramuscular fatty infiltration. A 79-year-old female study participant with a partial-thickness supraspinatus tear. (a) Oblique sagittal magnetic resonance (MR) 6-point Dixon fat fraction map image at the Y-shaped view shows manual placement of a ROI (gold outline) at the supraspinatus muscle for calculation of Dixon fat fraction. (b) Corresponding oblique sagittal T1-weighted image at the Y-shaped view used to determine Goutallier grade. A 67-year-old male study participant with a full-thickness supraspinatus tendon tear. (c) Oblique sagittal MR 6-point Dixon fat fraction map image at the Y-shaped view shows manual placement of a ROI (gold outline) at the supraspinatus muscle for the calculation of Dixon fat fraction. (d) Corresponding oblique sagittal T1-weighted image at the Y-shaped view used to determine Goutallier grade. This second example shows a greater degree of visible supraspinatus intramuscular fatty infiltration relative to the first example.
One blinded musculoskeletal radiologist and another blinded musculoskeletal radiology fellow evaluated DICOM image modules that contained the single de-identified oblique sagittal T1-weighted MR image for each participant corresponding to the Dixon fat fraction map Y-shaped view MR image. Each blinded rater independently determined Goutallier grade for the supraspinatus muscle using MIPAV software [Figure 2b and d]. Goutallier grade is a semi-quantitative 5-point ordinal scale of intramuscular FI: Grade 0, no fat; Grade 1, streaks of fat; Grade 2, muscle > fat; Grade 3, muscle = fat; and Grade 4, muscle < fat.[13,25,26] The mean Goutallier grade between raters for the supraspinatus muscle for each participant was used for analysis.
A second musculoskeletal radiologist independently evaluated each shoulder MRI to classify the status of the supraspinatus tendon. The supraspinatus tendon was assigned to one of three categories: Intact (inclusive of tendinopathy), PTT, or full-thickness tear (FTT) [Figure 3].

- Example images for the three categories of supraspinatus tendon status. A 63-year-old female study participant. (a) Oblique coronal short-tau inversion recovery (STIR) magnetic resonance (MR) image shows an “intact” supraspinatus tendon with no tear. A 61-year-old male study participant. (b) Oblique coronal STIR MR image shows a partial-thickness supraspinatus tendon tear (short arrow). (c) A 67-year-old male study participant shows a full-thickness supraspinatus tendon tear with medial retraction to the scapular glenoid (long arrow).
Clinical evaluation
At baseline, participants completed the Charlson comorbidity index (CCI), an instrument that measures chronic medical conditions to estimate health status among participants in research studies.[7,10,27] Participants also completed the ASES survey to quantify self-reported function of the shoulder ipsilateral to the MRI at baseline.[7,10] Height and weight were recorded to determine body mass index (BMI) at baseline. At the follow-up visit, participants again completed the ASES survey to estimate change in self-reported shoulder function over time.
Statistical analysis
Statistical analysis was performed using SAS statistical software version 9.4 (SAS, Cary, North Carolina). Descriptive statistics were performed to characterize the study sample, with categorical variables reported as n and continuous variables as mean ± standard deviation. Comparisons of subgroups within cohort were performed with the Kruskal–Wallis test, and the Mann–Whitney U-test was used to compare subgroups between cohorts. Interobserver reliability for Dixon fat fraction and Goutallier grade at the baseline MRI visit was assessed by the intraclass correlation coefficient and weighted kappa statistic, respectively. Interobserver reliability was interpreted as 0.00–0.039, poor; 0.40–0.59, fair; 0.60–0.74, good; and 0.75–1.00, excellent.[28] P < 0.05 was considered to indicate statistical significance.
RESULTS
At baseline, there were no differences in age, BMI, comorbidity, or ASES score among groups in the PT cohort [Table 1]. The PT cohort was 53% (8/15) male. The frequency of supraspinatus tendon status was 20% (3/15) intact, 60% (9/15) PTT, and 20% (3/15) FTT. On average, participants ranged from normal weight to overweight. Participants demonstrated evidence of low comorbidity, with the mean CCI index a reflection of the participants’ age. There was a significant difference in supraspinatus FI by Goutallier grade among the groups (P = 0.033), with the FTT group demonstrating the highest supraspinatus FI. The FTT group also showed the highest supraspinatus FI by Dixon fat fraction but without statistical significance.
| Baseline visit | Intact, n=3 | Partial-thickness tear, n=9 | Full-thickness tear, n=3 | P-value |
|---|---|---|---|---|
| Age (years) | 73.0±6.1 | 67.1±7.8 | 74.0±4.0 | 0.195 |
| BMIA(wt/ht2) | 25.2±1.1 | 26.5±5.1 | 24.6±3.8 | 0.895 |
| CCIB | 3.0±1.0 | 3.1±1.6 | 4.0±1.0 | 0.314 |
| ASESCscore | 58.9±8.2 | 65.5±18.9 | 79.9±1.7 | 0.186 |
| Dixon fat fractionD, % | 4.6±1.4 | 6.1±1.9 | 6.7±2.5 | 0.430 |
| Goutallier gradeE | 0.5±0.5 | 1.1±0.2 | 1.5±0.5 | 0.033 |
| Follow-up visit | Intact, n=2 | Partial-thickness tear, n=3 | Full-thickness tear, n=3 | P-value |
| Follow-up time (months) | 13.2±1.9 | 10.2±3.5 | 8.0±0.7 | 0.151 |
| Δ ASES score | 16.7±4.7 | −7.2±0.9 | 4.9±3.5 | 0.042 |
| Δ Dixon fat fraction,% | −0.7±0.7 | −0.1±3.20 | 0.6±2.0 | 0.682 |
| Δ Goutallier grade | −0.3±0.34 | 0.0±0.50 | 0.3±0.3 | 0.292 |
Values are mean±standard deviation unless otherwise noted. A: Body mass index, B: Charlson comorbidity index, C: American Shoulder and Elbow Surgeons, D: Supraspinatus muscle, E: Supraspinatus muscle, ASES: American Shoulder and Elbow Surgeon
At the follow-up visit, there were no differences among groups for change in supraspinatus FI by Dixon fat fraction or Goutallier grade over time in the PT cohort. Furthermore, there was no difference in the length of follow-up among the groups. A significant difference existed among groups for change in ASES score over time (P = 0.042), as participants who lacked supraspinatus tear demonstrated superior recovery in shoulder function relative to participants with a partial-thickness or full-thickness supraspinatus tear in the PT cohort.
At baseline, there were no differences in age, BMI, comorbidity, or ASES score among groups in the control cohort [Table 2]. The control cohort was 40% (10/25) male. The frequency of supraspinatus tendon status was 48% (12/25) intact, 60% (9/25) PTT, and 20% (4/25) FTT. On average, participants were overweight and showed low comorbidity with the mean CCI a reflection of the participants’ age. There was a significant difference in supraspinatus FI by Dixon fat fraction among the groups (P = 0.034), with the FTT group demonstrating the highest supraspinatus FI. The FTT group also showed the highest supraspinatus FI by Goutallier grade but was not statistically significant.
| Baseline visit | Intact, n=12 | Partial-thickness tear, n=9 | Full-thickness tear, n=4 | P-value |
|---|---|---|---|---|
| Age (years) | 67.3±6.8 | 71.1±5.2 | 73.0±8.0 | 0.129 |
| BMIA(wt/ht2) | 29.0±8.1 | 26.6±3.3 | 29.4±5.9 | 0.531 |
| CCIB | 2.8±0.8 | 3.0±1.2 | 2.8±1.0 | 0.969 |
| ASESCscore | 84.0±21.9 | 79.6±17.0 | 78.3±16.8 | 0.448 |
| Dixon fat fractionD, % | 5.8±1.2 | 7.1±6.3 | 21.4±10.4 | 0.034 |
| Goutallier gradeE | 0.8±0.5 | 1.0±0.6 | 2.4±1.7 | 0.141 |
| Follow-up visit | Intact, n=9 | Partial-thickness tear, n=9 | Full-thickness tear, n=3 | P-value |
| Follow-up time (months) | 9.2±3.8 | 9.8±3.5 | 10.4±4.2 | 0.392 |
| ΔASES score | 0.0±9.6 | −0.5±8.7 | −1.7±18.0 | 0.921 |
| ΔDixon fat fraction,% | 0.6±3.2 | 1.1±2.6 | −1.5±2.1 | 0.261 |
| ΔGoutallier grade | 0.2±0.4 | 0.5±0.7 | 0.3±0.6 | 0.713 |
Values are mean±standard deviation unless otherwise noted. A: Body mass index, B: Charlson comorbidity index, C: American Shoulder and Elbow Surgeons, D: Supraspinatus muscle, E: Supraspinatus muscle, ASES: American Shoulder and Elbow Surgeon
At the follow-up visit, there were no differences among groups for change in supraspinatus FI by Dixon fat fraction or Goutallier grade over time in the control cohort. Furthermore, there was no difference in the length of follow-up among the groups or change in ASES score over time.
At baseline, subgroup analyses between similar groups in the cohorts were performed: “Intact” PT cohort versus “intact” control cohort, “partial-thickness tear” PT cohort versus “partial-thickness tear” control cohort, and “full-thickness tear” PT cohort versus “full-thickness” control cohort. There were no differences for age, comorbidity, Dixon fat fraction, Goutallier grade, or frequency of supraspinatus tendon status for all subgroup comparisons. Furthermore, no significant difference in BMI was identified for all PT cohort versus control cohort subgroup comparisons. There was a significant difference identified for baseline ASES score in the “intact” PT cohort versus the “intact” control cohort (58.9 ± 8.2 vs. 84.0 ± 21.9, respectively, P = 0.049), but no difference for ASES score for “partial-thickness tear” or “full-thickness tear” subgroups. Although not reaching statistical significance, one notable trend was the observed lesser degree of supraspinatus FI at baseline in the “full-thickness tear” PT cohort versus the “full-thickness tear” control cohort: Dixon fat fraction, 6.6% ± 2.5% versus 21.4% ± 10.4%, respectively, P = 0.112; Goutallier grade, 1.5 ± 0.5 versus 2.4 ± 1.7, respectively, P = 0.377.
Subgroup analysis was performed for length of follow-up time and also for change in ASES score, Dixon fat fraction, and Goutallier grade over time. There were no differences between similar subgroups for each cohort.
Interobserver reliability for Dixon fat fraction was excellent (0.782, intraclass correlation coefficient). There was good interobserver reliability for Goutallier grade (0.712, weighted kappa statistic).
DISCUSSION
Our study found that older adults with full-thickness supraspinatus tear demonstrated significantly higher supraspinatus intramuscular FI in both the PT and control cohorts at baseline, as compared to those with PTT or no tear. There was also a trend to suggest that full-thickness supraspinatus tears had been present for a shorter time in the PT cohort relative to those in the control cohort, given the observation that symptomatic participants presenting for initial management by PT had lower supraspinatus FI at baseline as compared to the control participants with FTTs. No significant differences were observed for change in supraspinatus FI over time in either the PT or control cohorts. Participants receiving PT for full-thickness and partial-thickness supraspinatus tears reported significantly inferior functional recovery by ASES score relative to those with no tear.
MRI is a leading modality for diagnosis and characterization of RC tear and FI in the United States.[5,10,25] Investigators in animal and human research studies posit that advanced proliferation of FI occurs shortly after FTT.[5,12,29,30] The amount of FI associated with high-grade partial-thickness RC tear as compared to low-grade partial-thickness RC tear is relatively similar.[31] Patients with full-thickness RC tears are associated with higher FI relative to those with partial-thickness RC tears or no tear.[9,21,31] There is growing consensus among orthopedic surgeons to perform early RCR surgery for patients with symptomatic full-thickness RC tear before significant FI occurs, since delayed RCR surgery is associated with higher levels of FI and greater risk of poorer post-operative outcomes.[5,11,12,30,32]
Physical therapists are often the first health-care professionals to assess patients presenting with shoulder dysfunction, but there are little data on physical therapists’ role in ordering imaging studies in the United States.[20] Most physical therapists do not order imaging studies and are dependent on other health-care professionals to provide imaging referrals for their patients. In general, prohibitive state licensing boards or insurance companies’ non-authorization for payment limits physical therapists’ ability to provide imaging referrals for their patients. Most studies of physical therapists’ imaging utilization in the United States are limited to those performed at military facilities where physical therapists have explicit privileges to order imaging studies at federally operated health facilities.[33]
Physical therapists encounter patients through two basic referral patterns: Patients are either referred to a physical therapist by another health-care provider or a patient may report directly for care though self-referral.[17] There are several potential causes of shoulder dysfunction. Physical therapists, in general, establish a diagnosis through the assessment of patient age, history of the present illness, relevant medical history, and physical examination. Given that many shoulder conditions present with similar symptoms and signs, diagnostic imaging examinations are helpful to rule in and rule out potential diagnoses.[34] This presents a problem for patients who “self-refer” to a physical therapists, since physical therapists do not order imaging studies. Our study findings suggest that older adults who present for initial management of symptomatic full-thickness supraspinatus tear by PT are likely early in the course of tendon injury with low level of FI; and, also that this specific patient group is at potential risk for accumulation of significant FI over time if the FTT is not addressed in a timely fashion by RCR surgery in eligible patients.
Investigators have described a change in shoulder function over time by ASES score of ≥12 to represent at a minimally clinically important difference (MCID) in populations receiving non-operative treatment for RC tear.[35] Participants receiving shoulder rehabilitation with intact supraspinatus tendons showed a statistically significant improvement in shoulder function, demonstrating a MCID in ASES score of 17-point increase over time, relative to the 7-point decrease and 5-point increase in ASES score over time in the part-thickness and FTT groups in the PT cohort, respectively. Our study suggests that MRI has potential utility for providing important prognostic information for patients receiving PT for initial management of suspected RC tear as diagnosed by clinical examination only, although future larger studies are needed to verify this hypothesis.
This pilot study is not without limitation. The study sample was small but was still able to identify several statistically significant observations. The study population was a convenience sample, and the results many not be generalizable to the general population. The study may be limited by selection bias, since participants enrolled were only those who responded to recruitment advertising. Although statistically significant differences for supraspinatus FI by Goutallier grade among groups in the PT cohort and by Dixon fat fraction among groups in the control cohort were identified; future larger studies may be needed to show that the FTT group has statistically significant higher supraspinatus FI, relative to no tear or PTT groups, in each cohort by both methods. Participants in the PT cohort did not receive treatment by one experimental PT protocol, but instead received the “usual care” administered by their own shoulder rehabilitation specialists who were not members of the research team. Another limitation was fewer participants completing the follow-up visits relative to the baseline visits for the longitudinal analysis: Two participants in the control cohort were excluded from longitudinal analysis due to change in supraspinatus tendon tear status between baseline and follow-up visits; two participants were lost to follow-up (one in PT cohort and one in control cohort), and the remainder were precluded from the follow-up visit by our institution’s universal shutdown of in-person research during the COVID-19 pandemic (six in PT cohort and one in control cohort). The overall comorbidity of the study sample was low, and our results may not be generalizable to populations with a higher burden of comorbidity.
CONCLUSION
Our pilot study found that full-thickness RC tear is associated with higher levels of FI relative to PTT or no tear for the population of older adults receiving PT for initial management of clinically suspected RC tear. An observed trend suggests that full-thickness RC tears were relatively newer and had lower levels of FI in symptomatic older adults presenting for initial management by PT compared to full-thickness RC tears among older adult volunteers not seeking care, but future larger research studies are needed to further test this observation. Furthermore, future studies are warranted to evaluate the effect of diagnosis by imaging for the population of older adults who typically receive PT for initial management of presumed RC tear based on clinical examination only.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Support provided by the National Institute on Aging (NIA 3P30AG028747) and the University of Maryland Claude D. Pepper Older Americans Independence Center (NIA 3P30AG028747).
Conflicts of interest
There are no conflicts of interest.
References
- Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999;8:296-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19:116-20.
- [CrossRef] [PubMed] [Google Scholar]
- Muscle fatty infiltration in rotator cuff tears: Descriptive analysis of 1688 cases. Orthop Traumatol Surg Res. 2009;95:319-24.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet Disord. 2014;15:4.
- [CrossRef] [PubMed] [Google Scholar]
- Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35:719-28.
- [CrossRef] [PubMed] [Google Scholar]
- Variation in orthopaedic surgeons' perceptions about the indications for rotator cuff surgery. J Bone J Surg Am. 2005;87:1978-84.
- [CrossRef] [Google Scholar]
- Initial medical management of rotator cuff tears: A demographic analysis of surgical and nonsurgical treatment in the United States Medicare population. J Shoulder Elbow Surg. 2016;25:e378-85.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical versus nonsurgical management of rotator cuff tears: Predictors of treatment allocation. Am J Sports Med. 2015;43:2368-72.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability of supraspinatus intramuscular fatty infiltration estimates on T1-weighted MRI in potential candidates for rotator cuff repair surgery: Full-thickness tear versus high-grade partial-thickness tear. Skeletal Radiol. 2021;50:2233-43.
- [CrossRef] [PubMed] [Google Scholar]
- Association of patient self-reported shoulder scores to quantitative and semi-quantitative MRI measures of rotator cuff intramuscular fatty infiltration: A pilot study. AJR Am J Roentgenol. 2019;2013:1307-14.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging of arthroscopic supraspinatus tendon repair. J Bone J Surg Am. 2007;89:1770-6.
- [CrossRef] [PubMed] [Google Scholar]
- Fatty degeneration and atrophy of the rotator cuff muscles after arthroscopic repair: Does it improve, halt or deteriorate? Arch Orthop Trauma Surg. 2014;134:985-90.
- [CrossRef] [PubMed] [Google Scholar]
- Fatty muscle degeneration in cuff ruptures. Pre-and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78-83.
- [CrossRef] [Google Scholar]
- Muscle atrophy as a consequence of rotator cuff tears: Should we compare the muscles of the rotator cuff with those of the deltoid? Skeletal Radiol. 2007;36:841-45.
- [CrossRef] [PubMed] [Google Scholar]
- Tendon repair compared with physiotherapy in the treatment of rotator cuff tears: A randomized controlled study in 103 cases with a five-year follow-up. J Bone J Surg Am. 2014;96:1504-14.
- [CrossRef] [PubMed] [Google Scholar]
- Operative versus conservative treatment of small, nontraumatic supraspinatus tears in patients older than 55 years: Over 5-year follow-up of a randomized controlled trial. J Shoulder Elbow Surg. 2021;30:2455-64.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of patient use of physical therapy after referral for musculoskeletal conditions on future medical utilization: A retrospective cohort analysis. J Manipulative Physiol Ther. 2021;44:621-36.
- [CrossRef] [PubMed] [Google Scholar]
- The presentation and outcomes of shoulder pain in public hospital physiotherapy departments in NSW: An observational study. Physiother Theory Pract. 2014;30:299-305.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of radiographic imaging of the shoulder joint on patient management: An advanced-practice physical therapist's approach. Physiother Can. 2017;69:351-60.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation of quantitative versus semiquantitative measures of supraspinatus intramuscular fatty infiltration to shoulder range of motion and strength: A pilot study. Curr Probl Diagn Radiol. 2021;50:629-36.
- [CrossRef] [PubMed] [Google Scholar]
- Quantification of shoulder muscle intramuscular fatty infiltration on T1-weighted MRI: A viable alternative to the Goutallier classification system. Skeletal Radiol. 2019;48:535-41.
- [CrossRef] [PubMed] [Google Scholar]
- Surgically repaired massive rotator cuff tears: MRI of tendon integrity, muscle fatty degeneration, and muscle atrophy correlated with intraoperative and clinical findings. AJR Am J Roentgenol. 2005;184:1456-63.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation of arthroscopic repairability of large to massive rotator cuff tears with preoperative magnetic resonance imaging scans. Arthroscopy. 2009;25:573-82.
- [CrossRef] [PubMed] [Google Scholar]
- Association of rotator cuff tear patterns and intramuscular fatty infiltration on magnetic resonance imaging. J Clin Imaging Sci. 2019;9:38.
- [CrossRef] [PubMed] [Google Scholar]
- Fatty degeneration of the muscles of the rotator cuff: Assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. 1999;8:599-605.
- [CrossRef] [PubMed] [Google Scholar]
- Identification of community-dwelling older adults with shoulder dysfunction: A pilot study to evaluate the disabilities of the Arm, shoulder and hand survey. Geriatr Orthop Surg Rehabil. 2022;13:21514593221129177.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6:284-90.
- [CrossRef] [Google Scholar]
- Fatty infiltration is a prognostic marker of muscle function after rotator cuff tear. Am J Sports Med. 2018;46:2161-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of tendon release and delayed repair on the structure of the muscles of the rotator cuff: An experimental study in sheep. J Bone J Surg Am. 2004;86:1973-82.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance rotator cuff fat fraction and its relationship with tendon tear severity and subject characteristics. J Shoulder Elbow Surg. 2015;24:1442-51.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of early versus delayed repair of traumatic rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2011;19:1766-70.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic imaging in a direct-access sports physical therapy clinic: A 2-year retrospective practice analysis. Int J Sports Phys Ther. 2016;11:708-17.
- [Google Scholar]
- Comparison of the accuracy of telehealth examination versus clinical examination in the detection of shoulder pathology. J Shoulder Elbow Surg. 2021;30:1042-52.
- [CrossRef] [PubMed] [Google Scholar]
- Minimal clinically important differences in ASES and simple shoulder test scores after nonoperative treatment of rotator cuff disease. J Bone J Surg Am. 2010;92:296-303.
- [CrossRef] [PubMed] [Google Scholar]







