Translate this page into:
Stroke-Like Migraine Attacks after Radiation Therapy Syndrome: Clinical and Imaging Characteristics
Address for correspondence: Dr. Mina S Makary, Department of Radiology, The Ohio State University Wexner Medical Center, 395 W 12th Avenue, 4th Floor, Columbus, Ohio 43210, USA. E-mail: mina.makary@osumc.edu
-
Received: ,
Accepted: ,
Abstract
Stroke-like migraine attacks after radiation therapy (SMART) syndrome is a rare, reversible phenomenon that occurs several years after radiotherapy in patients treated for intracranial neoplastic lesions. Patients typically present with symptoms of headache, seizures, and other focal neurologic deficits concerning for stroke or disease recurrence. In this report, we describe SMART syndrome in a 70-year-old male who developed a persistent right temporal headache, right-sided neck pain, and new-onset seizures 12 years after surgical resection of a temporal anaplastic ependymoma followed by irradiation. We present this case to highlight typical disease presentation, imaging characteristics, and important differential radiologic considerations. Recognition of this delayed complication of brain tumor radiation is paramount given its self-limited course and favorable response to conservative therapy and to avoid misinterpreting imaging findings as tumor recurrence.
Keywords
Complications
radiation therapy
stroke-like migraine attacks
stroke-like migraine attacks after radiation therapy syndrome

INTRODUCTION
Stroke-like migraine attacks after radiation therapy (SMART) syndrome was first reported in four children with brain tumors who presented with unilateral headaches along with other neurological deficits 1–2 years after receiving whole-brain radiation.[1] Since then, other reports have described presentations including seizures and stroke-like episodes such as hemiplegia, aphasia, hemianopia, and migraine symptoms.[2] The occurrence has been reported as delayed as 35 years following high-dose brain irradiation of generally >50 Gy and has been reported in twice as many males as females.[3,4] Despite its worrisome presentation and challenging diagnosis, most patients with SMART syndrome improve clinically within 2 months on average along with reversal of their radiological findings.[5] In this report, we present a case of SMART syndrome with characteristic clinical and radiological findings, with an improvement of symptoms after 9 days of dexamethasone administration.
CASE REPORT
A 70-year-old man with a history of treated right temporal anaplastic ependymoma 12 years prior presented with seizures, progressive right-sided headache, and neck pain. Hospital records from his cancer institution revealed that the patient’s neuro-oncology therapies included surgical resection, neoadjuvant chemotherapy, and brain irradiation. His spouse noted that he was previously stable for the past decade following completion of his therapy until his symptoms developed during the past week. On physical examination, no new focal neurological deficits were elicited other than his stable hearing loss and baseline left superior quadrantanopia. Initial laboratory results were all unremarkable. Routine cerebrospinal fluid studies were within normal limits including cytology and viral tests (West Nile virus, enterovirus, and HSV 1 and 2).
Computed tomography imaging demonstrated chronic right-sided postsurgical changes, without evidence of intracranial hemorrhage, mass effect, or large territorial infarcts. Magnetic resonance imaging (MRI) revealed right-sided temporal and insular fluid-attenuated inversion recovery (FLAIR)-hyperintense signal abnormalities with associated gyriform enhancement. No corresponding diffusion restriction or increased perfusion was identified on diffusion-weighted imaging or perfusion imaging, respectively [Figure 1]. Magnetic resonance angiography and magnetic resonance venography studies did not demonstrate flow-limiting stenoses or occlusion.
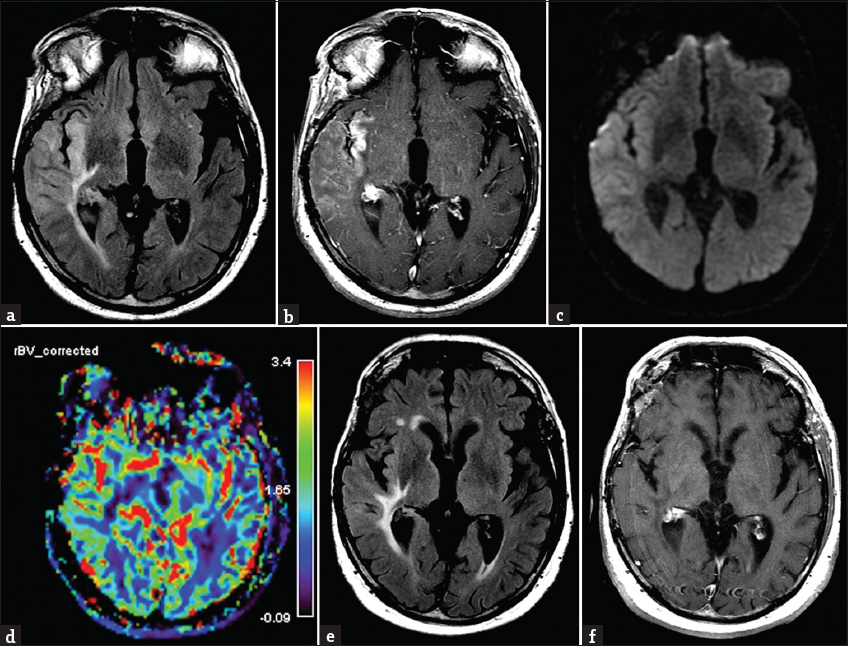
- Brain magnetic resonance imaging demonstrating characteristic findings of stroke-like migraine attacks after radiation therapy syndrome. (a) Fluid-attenuated inversion recovery image demonstrates insular and temporal T2 hyperintensities near the site of prior radiated tumor, with corresponding gyriform enhancement on postcontrast T1-weighted axial image (b) and expected lack of abnormalities noted on diffusion-weighted (c) and perfusion (d) images. Posttherapy imaging at 10 days demonstrates improved signal abnormalities on (e) fluid-attenuated inversion recovery and reduced enhancement on (f) postcontrast T1-weighted sequences.
Given the clinical presentation and imaging findings, the differential diagnosis included focal cerebritis due to an inflammatory or infectious etiology, tumor progression, and SMART syndrome. The patient was treated with antiepileptics as well as a trial of steroid therapy. The patient’s symptoms resolved within 10 days, and repeat imaging demonstrated significant improvement in the FLAIR-signal and gyriform enhancement [Figure 1]. A diagnosis of SMART syndrome was established based on the clinical presentation, imaging findings, and reversal of symptoms sparing the patient invasive testing such as biopsy and aggressive chemotherapeutic agents.
DISCUSSION
SMART syndrome is a rare neurologic complication that appears months to years after radiotherapy of intracranial neoplasms with unilateral headache and possibly along with other symptoms such as nausea, vomiting, hemiparesis, and seizures.[6] Although the pathophysiology of SMART syndrome is not clearly understood, radiation-induced damage of endothelial cells is proposed to be the initial insult,[7] with some considering the pathogenesis similar to posterior reversible encephalopathy syndrome (PRES) due to the insult leading to blood–brain barrier malfunction seen with some vasculopathies.[8] SMART syndrome is usually self-limited; therefore, invasive testing such as angiography or biopsy is not recommended and may even be harmful.[6]
Although there are no established diagnostic criteria for SMART syndrome, the diagnosis is generally made in the setting of (a) history of brain irradiation for cancer, (b) prolonged, reversible symptoms, migraine, seizures, hemiparesis, or other neurological symptoms, (c) characteristic, reversible MRI findings of gadolinium enhancement with abnormal T2 and FLAIR-signal of the previously treated location, (d) eventual complete or partial recovery, (e) lack of evidence of residual or recurrent tumor, and (f) lack of other attributable causes to other diseases (e.g., stroke).[9] Emphasis is typically laid upon the reversibility of not only the clinical symptoms of SMART but also the radiological findings. The radiologic hallmark of SMART syndrome is increased T2 hyperintensity in the previously radiated location and gyral enhancement in the same region evident within 1 week of neurological symptoms.[7]
The radiological differential for T2/FLAIR hyperintensities in the setting of cancer history includes disease recurrence. However, increased perfusion in the affected area and persistent of the abnormal signal on a short-term follow-up study can help distinguish tumor from SMART syndrome. Another consideration in patients presenting with SMART syndrome is a recent infarct. Depending on when the patient presents, diffusion restriction may not be reliable if the timing overlaps with a subacute or chronic stroke timeframe. The lack of a vascular territory and the clinical history can be helpful, but ultimately the resolution of the presenting deficits would rule out this diagnosis. It is important to note, however, that while reversibility of symptoms is the general rule for patients with SMART syndrome, a case series by Black et al., demonstrated that 45% of their patient cohort had incomplete neurologic recovery unlike previous reports.[2] Another consideration is peri-ictal pseudoprogression which can demonstrate similar MRI findings, although the concomitant seizure presentation, epileptiform pattern on electroencephalography, and generally increased perfusion on MRI can distinguish this diagnosis.[10,11] Finally, patients with SMART syndrome often raise suspicion for PRES, particularly when findings occur in a posterior distribution, have the common headache presentation, and typical reversibility. The unilateral distribution of findings and clinical context typically favors SMART syndrome, although it should be noted that up to 12% of patients with PRES present with unilateral MRI findings.[12]
With improved survival trends in patients with brain neoplasms and established role of radiation therapy, awareness and early recognition of SMART syndrome are paramount to spare patients from undergoing invasive interventions such as biopsies or unnecessary chemotherapy. The prognosis is overall favorable with most patients recovering completely within an average of 2 months.[5] While there is no established treatment protocol for this rare, novel entity, corticosteroids have shown promising results in described cases.[13] Other treatment strategies such as antiplatelet agents, propranolol, and verapamil have been used for treatment with unknown utility, while early antiepileptic therapy for seizure control is beneficial and recommended.[14]
CONCLUSION
This report draws attention to the rare but potentially mis- and under-diagnosed occurrence of SMART syndrome as delayed complication of brain tumor irradiation. It often presents as a diagnostic challenge, but accurate and early diagnosis is key in guiding appropriate treatment and optimal clinical outcomes. In addition to suggestive imaging clues such as T2-hyperinsities and gyriform enhancement, the total clinical picture including headache symptoms, history of radiation, and potential responsive to short-term conservative therapy with follow-up should be considered when evaluating a patient for SMART syndrome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Complicated migraine-like episodes in children following cranial irradiation and chemotherapy. Neurology. 1995;45:1837-40.
- [Google Scholar]
- Stroke-like migraine attacks after radiation therapy (SMART) syndrome is not always completely reversible: A case series. AJNR Am J Neuroradiol. 2013;34:2298-303.
- [Google Scholar]
- Headache syndromes. In: Non-epileptic Childhood Paroxysmal Disorders. New York, NY: Oxford University Press; 2009. p. :338-9.
- [Google Scholar]
- SMART syndrome (stroke-like migraine attacks after radiation therapy) in adult and pediatric patients. J Child Neurol. 2014;29:336-41.
- [Google Scholar]
- Stroke-like migraine attacks after radiation therapy syndrome. Chin Med J (Engl). 2015;128:2097-101.
- [Google Scholar]
- SMART (stroke-like migraine attacks after radiation therapy) syndrome responded to steroid pulse therapy: Report of a case and review of the literature. E Neurological Sci. 2018;12:1-4.
- [Google Scholar]
- A 15-year-old girl with sudden onsent reversible neurologic symptoms after cranial irradiation for medulloblastoma. Semin Pediatr Neurol. 2018;26:124-7.
- [Google Scholar]
- SMART syndrome: A late reversible complication after radiation therapy for brain tumours. J Neurol. 2011;258:1098-104.
- [Google Scholar]
- A diagnosis of stroke-like migraine attacks after radiation therapy (SMART) as severe headache with stroke-like presentation. Iran J Neurol. 2016;15:237-9.
- [Google Scholar]
- Peri-ictal pseudoprogression in patients with brain tumor. Neuro Oncol. 2011;13:775-82.
- [Google Scholar]
- Refractory status epilepticus due to SMART syndrome. Epilepsy Behav. 2015;49:189-92.
- [Google Scholar]
- Distinct imaging patterns and lesion distribution in posterior reversible encephalopathy syndrome. AJNR Am J Neuroradiol. 2007;28:1320-7.
- [Google Scholar]
- Acute late-onset encephalopathy after radiotherapy: An unusual life-threatening complication. Neurology. 2013;81:1014-7.
- [Google Scholar]
- Stroke-like migraine attack after cranial radiation therapy: The SMART syndrome. Pract Neurol. 2016;16:406-8.
- [Google Scholar]






