Translate this page into:
Spinal Tumors and Tumor-like Masses: Relevance of Initial Imaging, Karnofsky Performance Status, Age, Location, and Cord Edema

*Corresponding author: Dr. Virendra Singh, Department of Radiotherapy, MLN Medical College, Allahabad, Uttar Pradesh, India. singhv2003@gmail.com
-
Received: ,
Accepted: ,
Abstract
Objective: The aim of this study is to know the relevance of initial imaging, Karnofsky performance status,age,location and cord edema for future score development for radiologists.
Methods: The present study was carried out on total of 32 patients who visited SRN Hospital and Kriti scanning centre between August 2009 to February 2019. General and systemic examination was done. Finally KPS score was given to each patient in accordance with their clinical status. Magnetic resonance imaging was contemplated using scanner – Magnetom SP Vision; Siemens –Supercon 1.0 Tesla system.
Results: The morphologic characterization and specific assessment of various tumors and tumor like masses of spine in view of MR imaging features and their relationship with clinical features have been analyzed with Chi square test which reveal: Age versus location – χ2 = 4.32; df = 4; P > 0.36 (NS), age versus cord edema – χ2 = 4.27; df = 3; P > 0.23 (NS), and location versus cord edema – χ2 = 2.67; df = 2; P > 0.26 (NS). Chi Square test shows there is no any statistically significant association between age and location; age and spinal cord edema, and location and spinal cord edema. Correlation between clinical aggressiveness (change in follow-up KPS) and MR imaging features could not be assessed in our study because majority of patients could not be evaluated after one month because of loss of follow-up.
Conclusion: Poor KPS itself lead to movement during MRI and movement related artifacts affecting initial imaging,which was managed by cotton padded neck strap. KPS depends only on general condition one of the factor for outcome so for future score development age,location and cord edema together may be useful.
Keywords
Spinal tumors
Imaging
KPS score
Age
Location
Cord edema
INTRODUCTION
Magnetic resonance imaging (MRI), myelography, post-myelo-computed tomography, and bone scan are the mainstay of evaluation of tumors of the spine. In the extradural space, MRI is the most sensitive technique for the detection of neoplasms in the vertebrae. The MRI may be tailored specifically toward the question of spinal cord compression and signal changes and cord edema. Clinical aggressiveness of tumors increases at extreme of ages. Clinical aggressiveness also depends on tumor doubling time.
The Karnofsky performance status (KPS) scale has been used as an assessment tool for performance status in oncology since 1948.[1] It is commonly regarded as the gold standard measurement of performance status in cancer.[2,3] The KPS scale assesses three dimensions of health status – activity, work, and self-care and can be administered by any health-care professional for a quick assessment of general functioning and survival.[4] When KPS is low, it is a sensitive predictor of poor prognosis, but when high it is a poor cross-sectional indicator of prognosis.[2] KPS decrease by 20 points over a month time has been suggested as low clinical aggressiveness, 40 points decrease as moderate clinical aggressiveness, and 60 points decrease as high clinical aggressiveness.[1] The aim of this study is to know the relevance of initial imaging, KPS, age, location, and cord edema for future score development for radiologists.
MATERIALS AND METHODS
The present study was carried out on total of 32 patients visiting the Radiology Department of SRN Hospital of MLN Medical College, Allahabad, and Kriti Scanning Centre between August 2009 and February 2019.
Written consent was taken from the patients subjected to this study. A detailed history including back pain, weakness or paralysis, sensory loss, and change of bowel function was taken. General and systemic examination was done followed by neurological examination to localize the level of cord lesion. Finally, KPS score was given to each patient in accordance with their clinical status. Patient was sent for treatment and follow-up KPS was assessed after 1 month.
MRI was contemplated using scanner – Magnetom SP Vision; Siemens – Supercon 1 Tesla system, with only dedicated (body: L and XL for thoracic + lumbar spine and cervical spine) coils. T1W and T2W sequences in sagittal and axial plane were taken for thoracic and lumbar spine and sagittal T1W and T2W and axial T1 and gradient-recalled echo images for cervical spine as standard protocol.
In addition, short inversion time inversion recovery sequences to suppress fat in paraspinal soft tissue, FLASH, and T1W FAT-SAT sequences were also included wherever necessary.
Post contrast study was also carried out with intravenous Gadopenate Dimeglumine when needed.
RESULTS
A total of 32 patients were included in the study, 66% of affected were male and the most common age group involved was 21–40 years (34.47%) age group [Figure 1]. The only diagnosed entity in this age group was neoplastic disease which included – metastasis, cavernous hemangioma, astrocytoma, chordoma, lipoma, lymphoma, three cases of meningioma, and two cases of ependymoma. No tumor-like mass was seen.
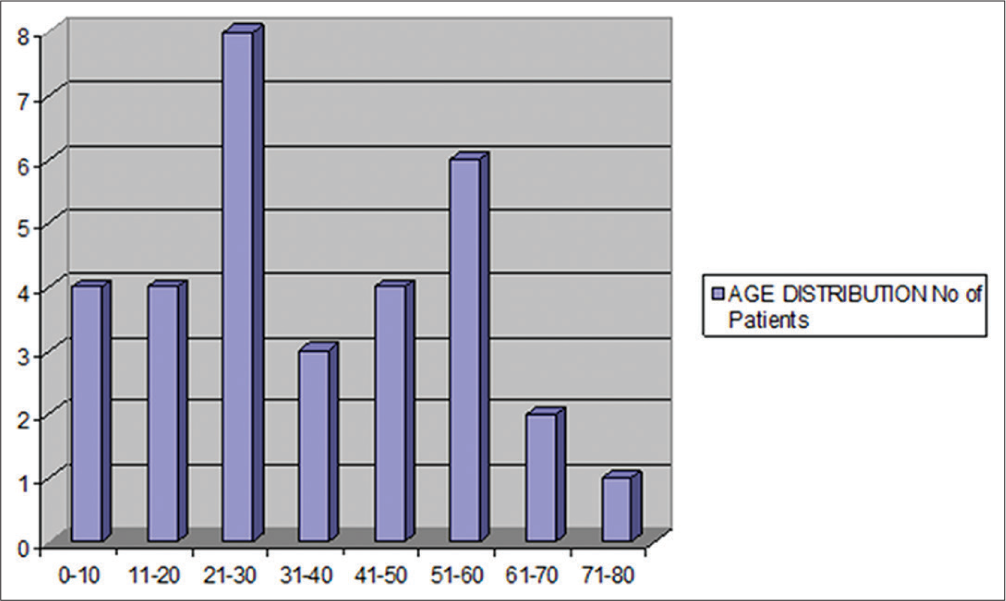
- Age and sex wise distribution of patients.
Overall, the most common neoplasm was meningioma (15.6%) followed by lymphoma (12.5%).
The most common location involved was intradural extramedullary (37.93%) comprising meningioma, nerve sheath tumor, lipoma, epidermoid, and metastasis [Table 1]. 34.48% of cases were seen in extradural compartment and 27.59% of cases in intramedullary compartment. Maximum incidence of secondary neoplasms was seen in extradural compartment (60% of total secondary).
| Location of tumor | Number of cases | ||
|---|---|---|---|
| Tumor (n=29) | Tumor-like mass (n=3) | ||
| Primary | Secondary | ||
| Extradural (n=11) | |||
| Osseous | 5 | 3 | 1 |
| Paraspinal muscles | 1 | 0 | 0 |
| Epidural | 1 | 0 | 0 |
| Intradural extramedullary (n=11) | 10 | 1 | 0 |
| Intramedullary (n=10) | 7 | 1 | 2 |
| Total | 24 | 5 | 3 |
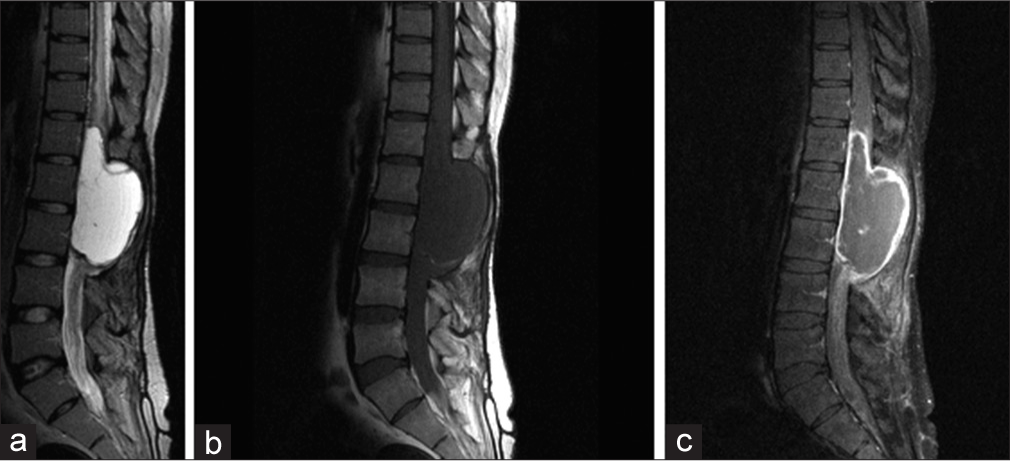
Of the neoplastic cause, secondary tumor, i.e., metastasis was accounting for 17.24% of cases. Extradural osseous location constitutes 60% of metastatic tumors [Figure 2]. Here, destruction of pedicles appears to occur only in combination with involvement of posterior portion of vertebral body.

- Metastasis: Know case of bronchogenic carcinoma presented with sudden onset quadriparesis: sagittal T2 W (a) images show multiple patchy hyperintense signal changes in D3 and D4 vertebral bodies with minimal loss of vertebral body height and presence of large abnormal prevertebral and posterior epidural hypointense soft tissue compressing narrowing spinal cord with foal cord edema.-Sagittal T1 W images (b) shows hypointense signal changes in D3 and D4 vertebral bodies with minimal loss of vertebral body height and presence of large abnormal prevertebral and posterior epidural hypointense soft tissue compressing narrowing spinal cord.
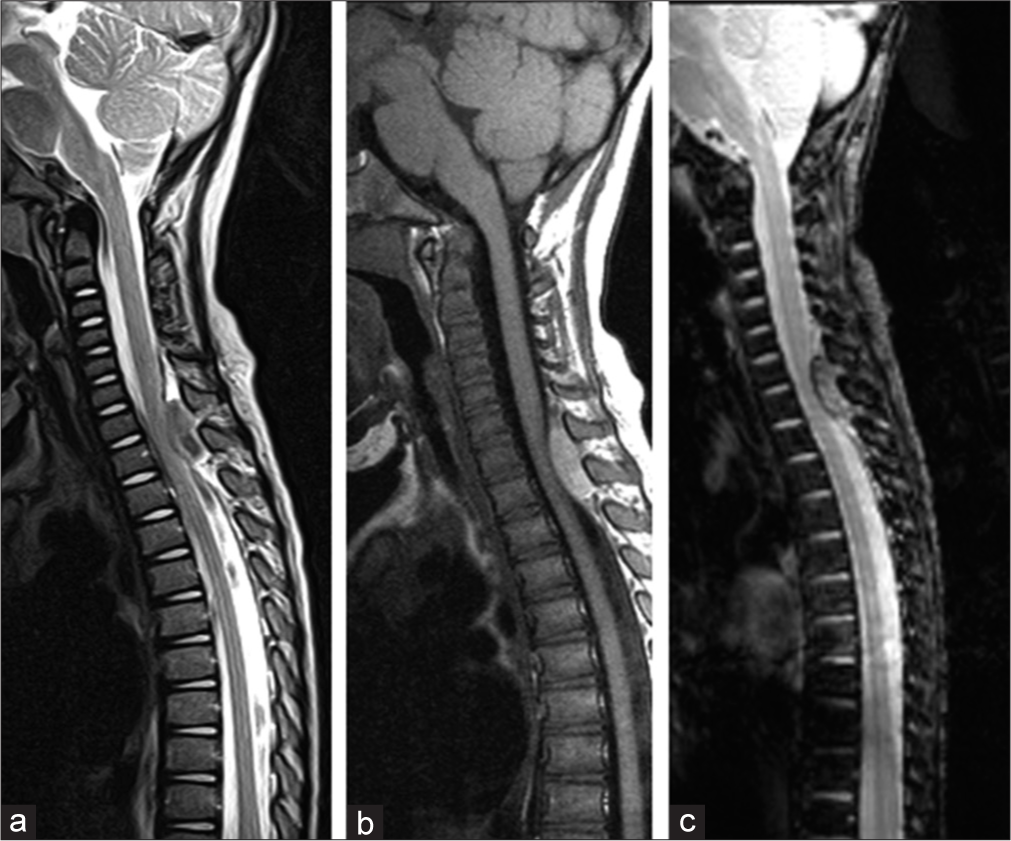
Among primary non-lymphoproliferative tumors (n = 22), the most common entity was meningioma (22.72%) followed by nerve sheath tumors (13.63%), astrocytoma (13.63%), and ependymoma [Figure 3] (13.63%). Besides, these other varieties noted were epidermoid cyst, intradural extramedullary lipoma, paraspinal soft tissue hemangioma, Ewing’s sarcoma, sacrococcygeal chordoma, and intramedullary hemangioma [Table 2].
- Ependymoma Conus medullaris: a) sagittal T2W image shows large well-defined septated intradural extramedullary hyperintense mass related to conus medullaris causing focal scalloping and widening of spinal canal and compressing narrowing conus with focal cord edema. (b) Sagittal T1W images show that lesion is hypointense on T1W images and shows peripheral T1 hyperintense rim suggestive of hemorrhage, (c) sagittal post-contrast fat-sat T1W images reveal peripheral enhancing rim of lesion with subtle patchy intralesional.
| Compartment | Tumor | No (%) | Tumor-like masses | No (%) |
|---|---|---|---|---|
| Intramedullary (n=8) | Ependymoma | 3 (10.34) | Granuloma | 1 (33.33) |
| Astrocytoma | 3 (10.34) | Syrinx | 1 (33.33) | |
| Cavernous hemangioma | 1 (3.44) | |||
| Metastasis | 1 (3.44) | |||
| Intradural extramedullary (n=11) | Meningioma | 5 (17.34) | ||
| Nerve sheath tumor | 3 (10.34) | None | 0 (0) | |
| Lipoma | 1 | |||
| Epidermoid | 1 | |||
| Metastasis | 1 | |||
| Extradural (n=10) | Lymphoma | 4 | Tubercular osteomyelitis | 1 (33.33) |
| Metastasis | 3 | |||
| Ewing’s sarcoma | 1 | |||
| Chordoma | 1 | |||
| Cavernous hemangioma | 1 |
The maximum incidence of spinal neoplasm was noted at dorsal spine (41.38%) followed by eight cases at dorsolumbar and lumbar spine (27.58%) in the present study.
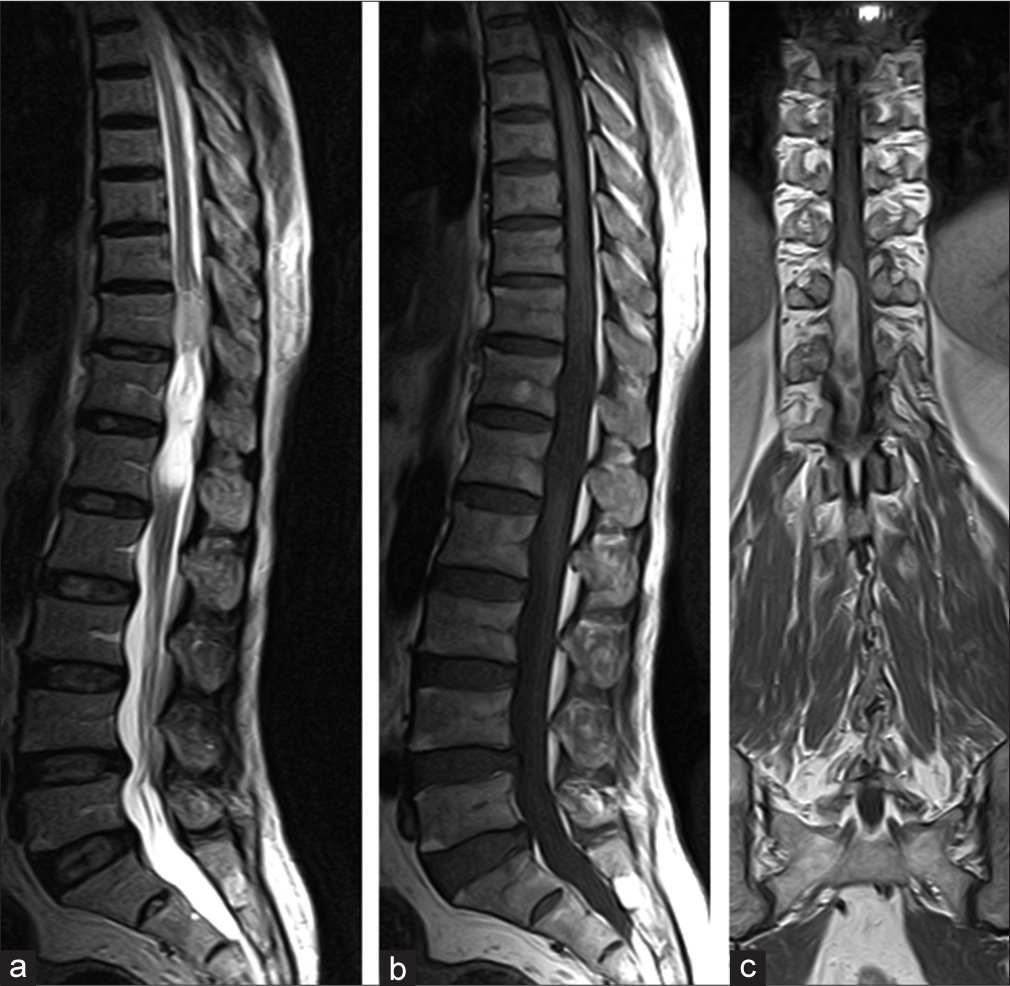
Four non-neoplastic tumor-like masses seen – (i) tuberculous spondylodiskitis (ii) intramedullary granuloma, (iii) syrinx, and (iv) epidural hematoma [Figure 4].
- Epidural hematoma: (a) sagittal T2W image shows small posterior extradural hypointense soft tissue compressing narrowing spinal cord with focal cord edema. (b) Sagittal T1W image shows that lesion is homogeneously hyperintense on T1W images. (c) Sagittal T2 FLASH images reveal peripheral as well as central specks of blooming.
Evidence on MRI of involvement of two consequent vertebrae and the intervening disk is virtually diagnostic of infective spondylitis. In tuberculous spondylitis, the cortical definition of the affected vertebrae was found to be invariably lost, in contradistinction to pyogenic spondylitis.
In the present study, solitary cervical cord granuloma was seen. Intracranial tuberculomas have been described as low-intensity lesions with or without central hyperintensity (due to varying amount of caseous necrosis) on T2WI and as hypo to isointense lesions on T1WI. In the present study, same features were seen.
Syringohydromyelia was observed in association with dorsal dermal sinus. In the present study, cord edema was seen in 19 (59.4% of total) patients, of which 73.68% of patients have >70 initial KPS at the time of MRI, 21.05% have KPS 50–70, and 5.26% have <50 KPS. 61.35% of cases having no spinal cord edema, 13–40.6% of total patients have initial KPS >70, 30.78% have KPS 50–70, and 7.69% of cases have initial KPS <50. Thus, majority of patients of both groups, having cord edema present and absent, have good KPS that is >70 [Table 3]. Thus, there was no significant association between MRI features and initial KPS. Furthermore, no significant correlation was seen between clinical features and MRI features whether they are typical features of particular diagnosis or features are indeterminate.
| Initial KPS | Cord edema present (n=19) (Number of patients) | Cord edema absent (n=13) (Number of patients) |
|---|---|---|
| >70 | 14 (73.68) | 8 (61.53) |
| 50–70 | 4 (21.05) | 4 (30.78) |
| <50 | 1 (5.26) | 1 (7.69) |
KPS: Karnofsky performance status
In the present study, majority of patients of both groups, having cord edema present and absent, have good KPS that is >70. Furthermore, patients with MRI features of all three groups (typical/variable/indeterminate) had same distribution of KPS [Table 4].
| Initial KPS score | Typical MRI features (Number of patients) | Variable/additional finding (Number of patients) | Indeterminate (Number of patients) |
|---|---|---|---|
| >70 | 15 | 5 | 3 |
| 50–70 | 8 | 0 | 0 |
| <50 | 0 | 1 | 0 |
MRI: Magnetic resonance imaging, KPS: Karnofsky performance status
The morphologic characterization and specific assessment of various tumors and tumor-like masses of spine in view of MRI features and their relationship with clinical features have been analyzed with Chi-square test which reveal: Age versus location – χ2 = 4.32; df = 4; P > 0.36 (NS), age versus cord edema – χ2 = 4.27; df = 3; P > 0.23 (NS), and Location versus cord edema – χ2 = 2.67; df = 2; P > 0.26 (NS). Chi-square test shows that there is no statistically significant association between age and location; age and spinal cord edema; and location and spinal cord edema.
KPS decrease by 20 points over a month time has been taken as low clinical aggressiveness, 40 points decrease as moderate clinical aggressiveness, and 60 points decrease as high clinical aggressiveness. Correlation between clinical aggressiveness (change in follow-up KPS) and MRI features could not be assessed in our study because majority of patients could not be evaluated after 1 month due to loss of follow-up [Table 5].
| MRI features | Initial KPS | Median initial KPS | KPS after 1 month | Median KPS after 1 month |
|---|---|---|---|---|
| Indeterminate | 90 (n=1) | 80 | LTF | Cannot be calculated |
| 80 (n=2) | LTF | |||
| Variable/additional (Internet literature search) | 100 (n=1) | 80 | 100 | |
| 80 (n=3) | LTF | |||
| 40 (n=1) | LTF | |||
| 90 (n=1) | LTF | |||
| Typical features | 50 (n=2) | 50 | 50 | 50 |
| 60 (n=1) | 60 | |||
| 50 (n=4) | LTF | |||
| 60 (n=1) | LTF | |||
| 80 (n=9) | LTF | |||
| 90 (n=5) | LTF | |||
| 100 (n=1) | LTF |
LTF: Lost to Follow-up, MRI: Magnetic resonance imaging, KPS: Karnofsky performance status
The primary tumor of spine may exhibit characteristic imaging features that can help in early diagnosis and improved prognosis.
DISCUSSION
The present study focuses on the MRI evaluation in tumors and tumor-like masses of the spine and correlation between MRI features of disease and clinical aggressiveness. MRI has been contemplated as the initial procedure in the evaluation of 32 cases of clinically suspected spinal tumor.
According to Nittner, approximately one-fifth of all central nervous system tumors occur in the spine with frequencies at various level of spinal canal (cervical, thoracic, and lumbar) roughly proportional to the number (and length) of segments at that level.[5,6] The same observation was quoted by Masaryk[6] In the present study, the most common location is dorsal spine (44.83%) followed by lumbar (17.24%) and then cervical (13.79%) and dorsolumbar (10.34%) spine. Chordoma in our study also had predominant large soft tissue mass anterior to sacrum as noted in other studies.[8]
According to their anatomical location, spinal tumors are conveniently classified as extradural, intradural extramedullary, and intramedullary tumors with intradural extramedullary tumors being the most common (50%) followed by extradural tumors (30%) and least common were intramedullary tumors (20%).[9] The present study has same distribution as above and following observation has been summarized below: Intradural extramedullary – 37.93%, Extradural – 34.48%, and intramedullary – 27.59%.
The primary tumor of spine may exhibit characteristic imaging features that can help in early diagnosis and improved prognosis.[10]
Nittner in his 1976 review of 4885 adult spinal cord tumors presented in literature, found nerve sheath tumor [Figure 5] (23%), meningiomas (22%), glial tumors (13.2%), ependymomas (2.5%), sarcoma (8.2%), and metastasis (6%) to be the most common.[7] The remaining 25% of cases were dispersed among a wide variety of miscellaneous mass lesions. In the present study, metastasis and meningioma account for the most common neoplasia (17.24% each), followed by nerve sheath tumor, astrocytoma, and ependymoma (10.34% each). The rest of the entities are lymphoma, lipoma, hemangioma, and chordoma.
- Nerve sheath tumor: (a and b) Sagittal T2 and T1W images show well-defined heterogeneous hyperintense on T2 and hypointense on T1 intradural extramedullary space occupying lesion with mild perifocal cord edema. (c) Post-gadolinium coronal T1W image shows heterogeneous enhancement of lesion lying on the right side with no neural foraminal extension.
Meningiomas are second only to nerve sheath tumors in frequency. However, in the present study, meningioma (17.24%) was more common than nerve sheath tumor (10.34%).
In the present study, from infective group of tumor-like masses, two cases were seen, one case seen of tubercular osteomyelitis and one of intramedullary granuloma.
Spinal tuberculosis can occur at any age and affects both sexes equally. Since dura constitutes an effective barrier against intraspinal spread of infection, extradural lesions are most common while intradural extramedullary lesions are least common.[9] In the present study, one case was intramedullary granuloma.
CONCLUSION
Poor KPS itself leads to movement during MRI and movement-related artifacts affect initial imaging interpretation, this was managed by cotton padded neck strap instead of the use of anesthesia so KPS has relevance to initial imaging interpretation. KPS depends on general condition, only one of the factors related to outcome so for future score development age, location, and cord edema together may be useful.
Acknowledgment
Kriti Scanning Centre Pvt., Ltd., 55 B Lowther Road, Allahabad, for providing MRI facility for the patients included in the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Vertebral osteomyelitis: Assessment using MR. Radiology. 1985;157:1985-157.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging of the spinal cord and canal: Potential and limitations. AJNR Am J Neuroradiol. 1984;5:1984-5.
- [CrossRef] [Google Scholar]
- Infectious and inflammatory processes of the spine. Radiol Clin North Am. 1991;29:809-27.
- [Google Scholar]
- Neoplasms, Spinal Cord. Charlottesville: Multimedia; 2009.
- Spinal meningiomas, neurinomas and neurofibromas and hourglass tumors In: Vinken PJ, Brum GW, eds. Handbook of Clinical Neurology. Vol 20. New York: Elsevier North Holland; 1976. p. :177-322.
- [Google Scholar]
- Clinical and imaging features of cervical chordoma. AJR Am J Roentgenol. 1999;172:1999-172.
- [CrossRef] [PubMed] [Google Scholar]
- The use of nitrogen mustard in the palliative treatment of cancer. Cancer. 1948;1:1948-1.
- [CrossRef] [Google Scholar]
- Imaging features of primary tumors of the spine: A pictorial essay. Ind J Radiol Imaging. 2016;26:2016-26.
- [CrossRef] [PubMed] [Google Scholar]
APPENDICES
| Score (Category) | KPS scale |
|---|---|
| 100 (A) | Normal; no complaints; no evidence of disease |
| 90 (A) | Able to carry on normal activity; minor signs or symptoms |
| 80 (A) | Normal activity with effort; some signs or symptoms of disease |
| 70 (B) | Cares for self; unable to carry on normal activity or to do active work |
| 60 (B) | Requires occasional assistance but is able to care for most of his needs |
| 50 (B) | Requires considerable assistance and frequent medical care |
| 40 (C) | Disabled; requires special care and assistance |
| 30 (C) | Severely disabled; hospitalization necessary; active supportive treatment is necessary |
| 20 (C) | Very sick; hospitalization necessary; active supportive treatment is necessary |
| 10 (C) | Moribund; fatal processes progressing rapidly |
| 0 | Dead |
KPS: Karnofsky performance status






