Translate this page into:
Sonographic Upper Gastrointestinal Series in the Vomiting Infant: How We Do It
Address for correspondence: Dr. Thaddeus W. Herliczek, Department of Diagnostic Imaging, Warren Alpert School of Medicine, Brown University, 355 Eddy Street, Providence, RI 02903, USA. E-mail: thaddeus_herliczek@brown.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Sonography (ultrasound) is used routinely to assess an infant with nonbilious projectile emesis. Fluoroscopic upper gastrointestinal (UGI) series has been the standard method to evaluate infants with bilious emesis. We use sonographic UGI routinely to assess infants with nonbilious emesis as well as infants with bilious emesis. This essay illustrates our technique, the results obtained using this technique for normal anatomy, and the commonly encountered pathology.
Keywords
Malrotation
pediatric
sonographic UGI
ultrasound
hypertrophic pyloric stenosis
INTRODUCTION

Sonography (US) is the imaging modality recommended by the American College of Radiology (ACR) to assess an infant with nonbilious projectile emesis.[1]
As of 2008, the ACR recommends fluoroscopic upper gastrointestinal (UGI) series rather than US to evaluate infants with bilious emesis.[1]
More recently, Yousefzadeh described US as an assessment protocol for infants with bilious emesis.[23] His US technique remains controversial as neither prospective nor retrospective analyses of the technique's sensitivity and specificity are available. Nevertheless, we have used sonographic UGI for years and find it offers direct assessment of the gastroesophageal junction, stomach, pylorus, duodenum, and midgut fixation.
We use sonographic UGI routinely at our institution to assess infants with nonbilious emesis as well as infants with bilious emesis. We use it also to assess infants with persistent or progressive gastroesophageal reflux (GER) or GER complicated by failure to thrive, apnea, or aspiration.
The difference in cost between fluoroscopic UGI and sonographic UGI (US) at our institution is less than 2%. Although US is more expensive, this technique is quick, readily available, nonionizing, and portable, therefore it is valuable to us and we believe it is an alternative assessment tool that can be used by experienced pediatric sonologists.
Sonographic upper gastrointestinal series: Technique
Infants are not given any feed by mouth for 1–2 h prior to examination. However, no preparation or delay is prescribed for an infant with bilious emesis given the possibility of malrotation and midgut volvulus, a surgical emergency.
All sonographic UGI at our institution are performed either by a pediatric radiologist or performed initially by an experienced pediatric sonographer with confirmatory scanning done by the pediatric radiologist.
We use a linear high-frequency probe (9–17 MHz) to insonate two sonographic windows: (1) left and right hepatic lobes, and (2) epigastrum with graded compression.
Images are taken in sagittal and transverse planes. We find a transverse plane with craniocaudal obliquity to give the best results.
Luminal contrast medium is not always necessary, but has proved to be helpful in our experience. We give 30 mL 5% glucose water by mouth or 30 mL sterile water via nasogastric tube. The exam requires real-time assessment to demonstrate the entire course of the duodenum.
We spend 5 min or less performing sonographic UGI. If sonographic UGI for the infant with bilious emesis is equivocal at 5 min, fluoroscopic UGI is performed immediately.
Anatomy to assess
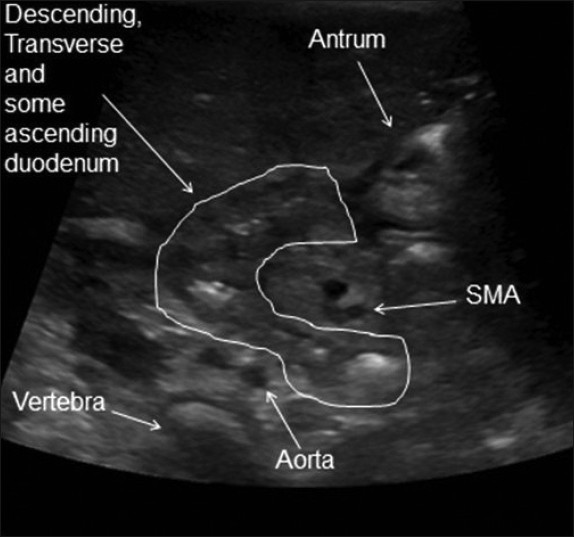
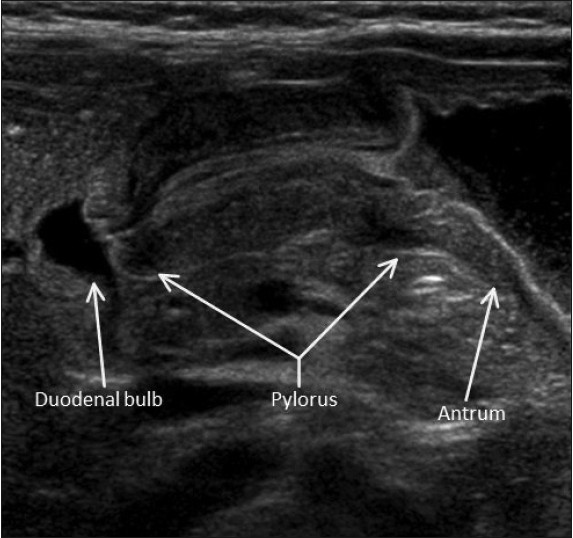
We assess the gastroesophageal junction [Figure 1], stomach, pylorus [Figure 2], and the entire course of the duodenum from pylorus to the duodenojejunal junction (DJJ) [Figures 3–5].
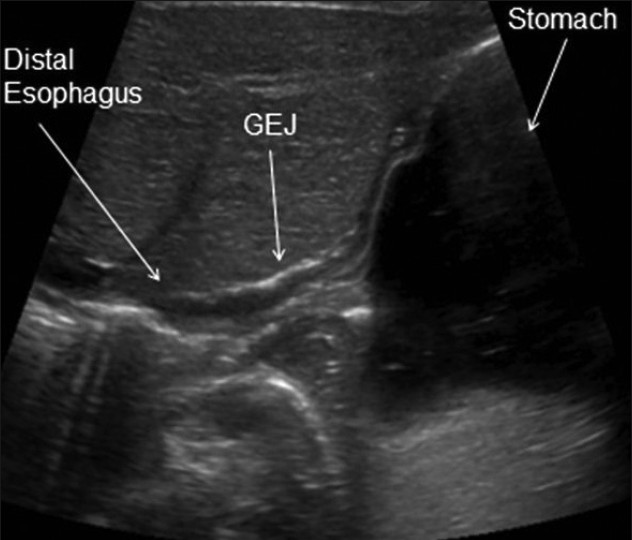
- Sonographic image of a healthy infant shows the gastroesophageal junction (GEJ) in an oblique sagittal plane.
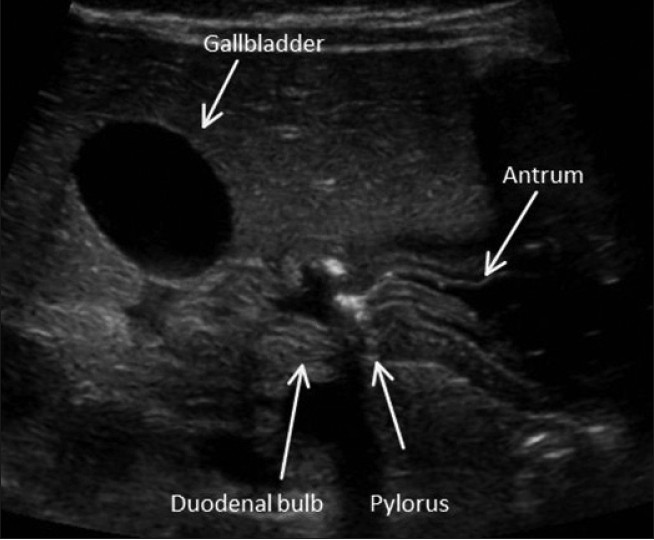
- Sonographic image of a healthy infant shows the gastroduodenal junction in a transverse plane.
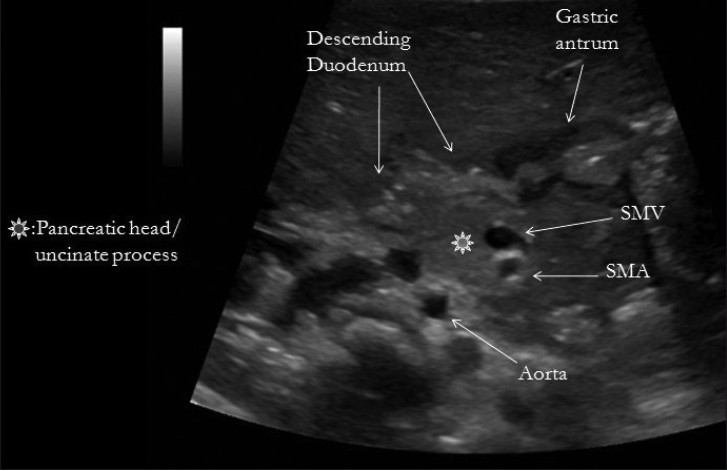
- Sonographic image of a healthy infant shows the retroperitoneum in a transverse plane.
- Sonographic image of a healthy infant shows the transverse portion of the duodenum positioned normally between superior mesenteric artery (SMA) and abdominal aorta.
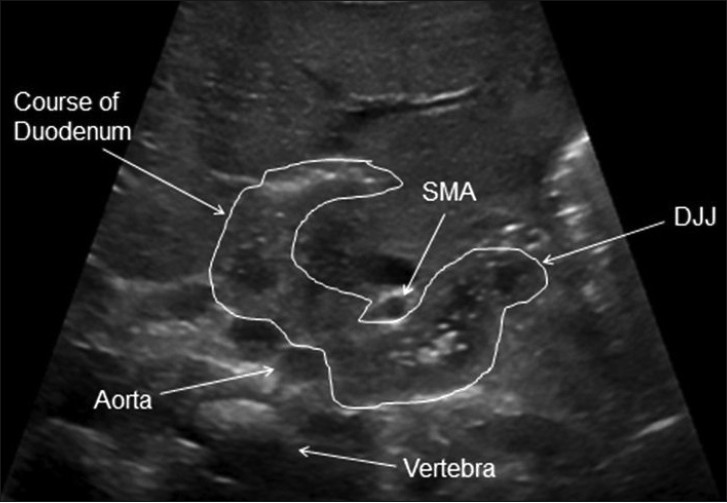
- Sonographic image of a healthy infant shows the normal course of the entire duodenum in a transverse plane with craniocaudal obliquity.
Particular attention is given to the relationship of the transverse, or third portion of duodenum (D3) to the superior mesenteric artery (SMA) and abdominal aorta as described by Yousefzadeh.[23] D3 normally courses between SMA and aorta [Figures 4 and 6].
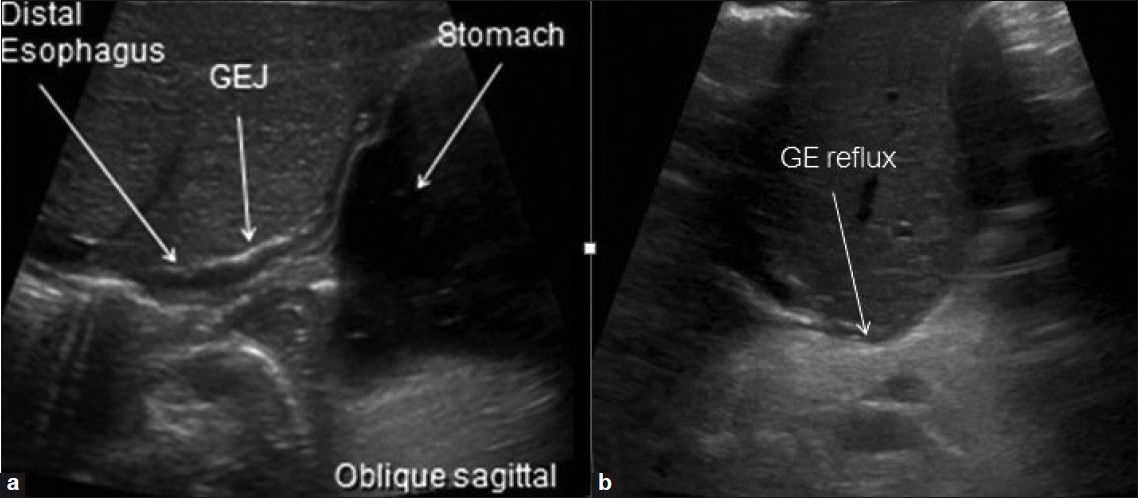
- Gastroesphageal reflux. US in an oblique sagittal plane shows (a) closed GEJ, (b) open GEJ with reflux of gastric contents (arrow).
We confirm if the DJJ is to the left of the vertebral column and reaches the height of the duodenal bulb.
While we routinely assess the normal mesenteric vascular relationship, it neither confirms nor excludes malrotation, as one third of infants with malrotation have a normal mesenteric vascular relationship. Also, an abnormal mesenteric vascular relationship can be seen in cases without malrotation.[4]
COMMON PATHOLOGY
Gastroesophageal reflux
While gastroesophageal reflux (GER) is a common entity in infants less than 6 months of age and often diagnosed clinically, our referring pediatricians and gastroenterologists appreciate real-time confirmation of this entity through observation of the infant's gastroesophageal junction [Figure 6].
Gastritis
While often diagnosed clinically or endoscopically, sonographic UGI can demonstrate diffuse gastritis and document its improvement [Figure 7].
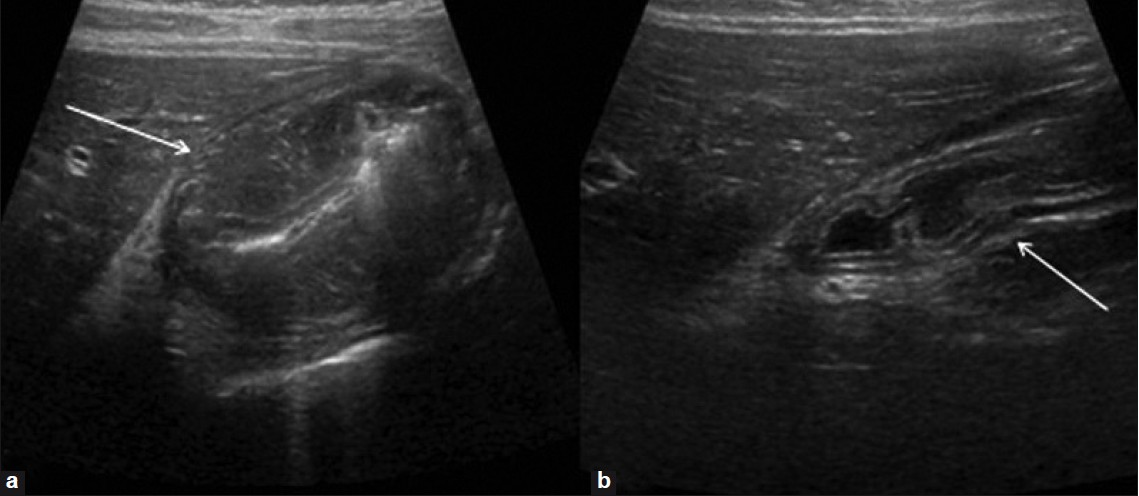
- Gastritis. US in a transverse plane shows (a) marked mural thickening (arrow) and (b) Resolution following appropriate therapy (arrow).
Hypertrophic pyloric stenosis
Sonography is the preferred imaging modality to assess an infant with hypertrophic pyloric stenosis (HPS). Objective criteria for HPS vary. We use a mural muscular thickness of more than 3 mm and a pyloric channel length of more than 16 mm. Real-time observation will demonstrate little, if any, transit of gastric contents into the duodenum. Additionally, real-time observation aids confident distinction of HPS from transient antral spasm [Figure 8].
- Hypertrophic pyloric stenosis. Sonographic image in a transverse plane
Technical tip: We suggest the infant be placed in a right lateral decubitus position for imaging. However, the pylorus may orient posteriorly and be difficult to image if the stomach is markedly distended. In such a case, using the left lateral decubitus position will improve visualization.
Duodenal duplication cyst
Enteric duplication cysts may occur in any location from the mouth to the anus and are most commonly encountered in the ileum. They can be found in the duodenum where they may produce symptoms of duodenal obstruction [Figure 9].
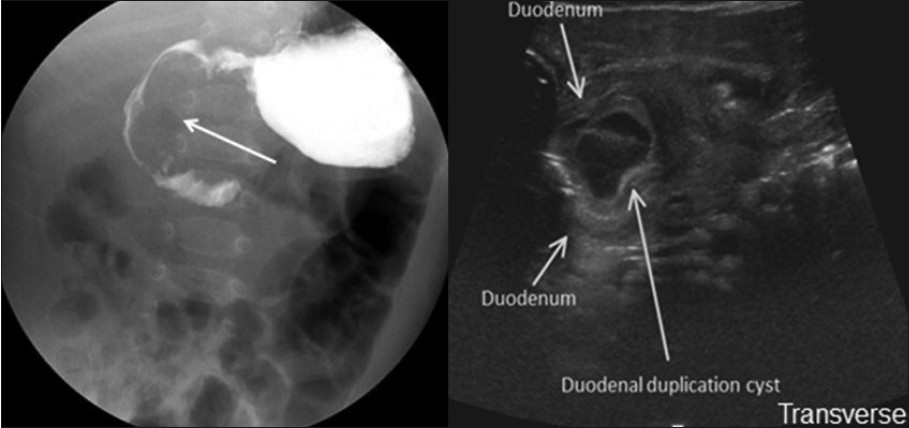
- Duodenal duplication cyst. (a) Frontal fluoroscopic projection demonstrates effacement of the medial aspect of the descending portion of the duodenum (arrow). (b) Sonographic UGI in a transverse plane demonstrates descending portion of duodenum and duplication cyst.
Annular pancreas
Annular pancreas is an uncommon developmental variant that often results in emesis in the neonate [Figure 10].
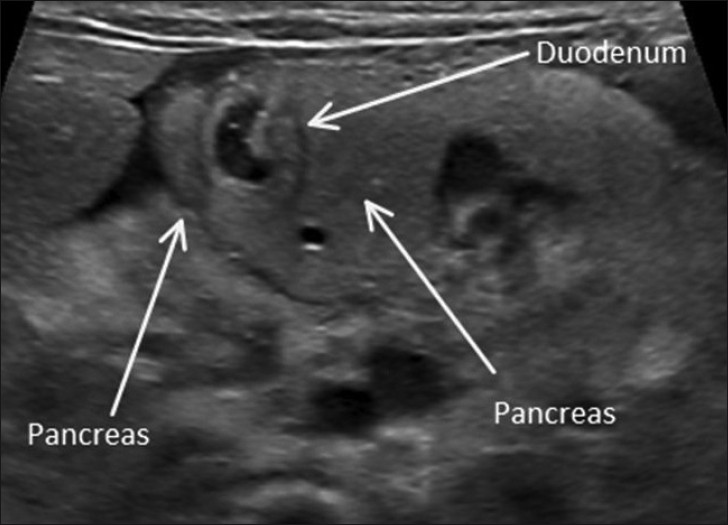
- Annular pancreas. Sonographic image in a transverse plane.
Malrotation
An aberrant midgut fixation predisposes to midgut volvulus. A majority of these infants present with bilious emesis in the neonatal period. Aberrant course of the duodenum with D3 anterior to the SMA, proximal duodenal obstruction, and a whirlpool sign can be seen [Figure 11].
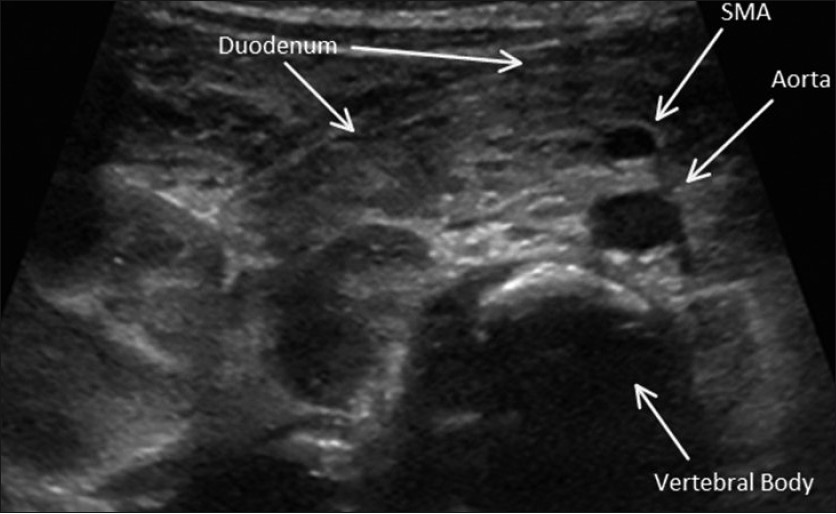
- Malrotation. Sonographic image in a transverse plane shows the transverse portion of the duodenum courses anterior to the superior mesenteric artery (SMA). No small bowel is seen interposed between SMA and abdominal aorta.
CONCLUSION
Sonographic UGI offers direct assessment of the gastroesophageal junction, stomach, pylorus, duodenum, and retroperitoneal anatomy in the vomiting infant.[23] Various pathologic entities of the upper gastrointestinal tract, including malrotation, are well demonstrated or excluded with sonographic UGI investigation of the vomiting infant. While the role of the sonographic UGI is controversial, we and the referring pediatricians and pediatric surgeons at our institution find it a useful tool in the assessment of a vomiting infant.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp? 2011/1/19/78528
REFERENCES
- American College of Radiology Appropriateness Criteria: Vomiting in Infants Up to 3 Months of Age. Available from: http://www.acr.org/SecondaryMainMenuCategories/quality_safety/app_criteria/pdf/ExpertPanelonPediatricImaging/VomitinginInfantsupto3MonthsofAgeDoc11.aspx
- [Google Scholar]
- The position of the duodenojejunal junction: the wrong horse to bet on in diagnosing or excluding malrotation. Pediatr Radiol. 2009;39:S172-7.
- [Google Scholar]
- Assessment of retromesenteric position of the third portion of the duodenum: an us feasibility study. Pediatr Radiol. 2010;40:1476-84.
- [Google Scholar]
- Midgut malrotation, the reliability of a sonographic diagnosis. Pediatr Radiol. 1991;22:21-3.
- [Google Scholar]






