Translate this page into:
Sincipital Encephaloceles: A Study of Associated Brain Malformations
Address for correspondence: Dr. Shashidhar Vedavyas Achar, Department of Radiodiagnosis, Assam Medical College and Hospital, Dibrugarh - 786 002, Assam, India. E-mail: raddrshashi@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
The aim of this study was to evaluate the associated intracranial malformations in patients with sincipital encephaloceles.
Materials and Methods:
A hospital-based cross-sectional study was conducted over 8 years from June 2007 to May 2015 on 28 patients. The patients were evaluated by either computed tomography or magnetic resonance imaging whichever was feasible. Encephaloceles were described with respect to their types, contents, and extensions. A note was made on the associated malformations with sincipital encephaloceles.
Results:
Fifty percent of the patients presented before the age of 3 years and both the sexes were affected equally. Nasofrontal encephalocele was the most common type seen in 13 patients (46.4%), and corpus callosal agenesis (12 patients) was the most common associated malformation. Other malformations noted were arachnoid cyst (10 patients), hydrocephalus (7 patients), and agyria-pachygyria complex (2 patients).
Conclusion:
Capital Brain malformations are frequently encountered in children with sincipital encephaloceles. Detail radiological evaluation is necessary to plan treatment and also to prognosticate such rare malformations.
Keywords
Brain malformations
encephalocele
intracranial anomalies
sincipital encephalocele

INTRODUCTION
Sincipital encephaloceles, also called frontal or anterior encephaloceles, are rare neural tube defects and are more common in South and Southeast Asian populations.[1] In children with sincipital encephaloceles there are often significant associated intracranial anomalies, including intracranial cysts, complete/partial corpus callosal agenesis, interhemispheric lipomas, facial clefts, and migrational anomalies. Occipital encephaloceles may be associated with Chiari or Dandy-Walker malformations and callosal or migrational anomalies. These anomalies are usually not associated with sincipital encephaloceles.[2] It is reported that younger siblings of patients affected with encephaloceles have up to 6% risk of a congenital central nervous system abnormality.[3]
MATERIALS AND METHODS
Study group
After approval from the institutional ethics review committee, a hospital-based cross-sectional study was conducted over 8 years from June 2007 to May 2015 on 28 patients in the departments of radiodiagnosis and pediatric surgery in a tertiary care hospital. The study comprised of outpatients and in patients, of both sexes presenting with sincipital encephaloceles. We have included only children in whom imaging studies were performed. Children in whom imaging studies were not done were excluded from the study. Informed consent was obtained from parents/guardian before undergoing the study.
Patient preparation
Patients were only allowed plain water preceding the imaging so as to keep the patient ready for sedation/anesthesia if needed.
Technique of study
The patients were evaluated by either computed tomography (CT) or magnetic resonance imaging (MRI) whichever was feasible. Of the 28 patients, 23 patients underwent CT and remaining 5 underwent MRI.
Computed tomography
The CT scanner used in this study was Siemens Somatom Spirit Dual Slice CT Scanner (Siemens Healthcare, Erlangen, Germany). Patients were scanned in supine position. Unenhanced CT scans of head and faciomaxillary region were obtained in all patients. Scanning parameters used were spiral mode with slice thickness of 6 mm and collimation 6 mm × 2.5 mm, pitch: 1.4; kVp: 130; mAs: 80. Field of view was kept at 25 cm. The three-dimensional reconstructed and multiplanar reformatted images were obtained. Reconstruction parameters included slice thickness of 3 mm and recon increment of 3 mm.
Magnetic resonance imaging
MRI imaging was performed with a 1.5-T superconducting magnet system 1.5 Tesla Siemens Magnetom Avanto B15 system (Siemens Healthcare, Erlangen, Germany) using a transmit/receive body coil with a 15-mT/m gradient. Patients were scanned in supine position. The imaging parameters were T1, T2, and fluid-attenuated inversion recovery (FLAIR) sequences obtained in all three planes: Axial, Coronal and Sagittal. Parameters for T1-WI (T1-weighted image): 400–600/15 (repetition time ms/echo time ms), 220–240-mm field of view, 256 × 192 matrix, and slice thickness of 5 mm with a gap of 1 mm. Parameters for T2-WI: 3200/428 (repetition time ms/echo time ms), 256-mm field of view, 256 × 256 matrix, and slice thickness of 5 mm with a gap of 1 mm. Parameters for FLAIR: 10,000/70–130 (repetition time ms/echo time ms), 240-mm field of view, 256 × 192 matrix, and slice thickness of 5 mm with a gap of 1 mm. Additional MR sequences were obtained whenever necessary.
The areas of interest in the study were type of encephalocele, its contents, extracranial extension and effect on adjacent structures and to look for associated brain malformations.
RESULTS
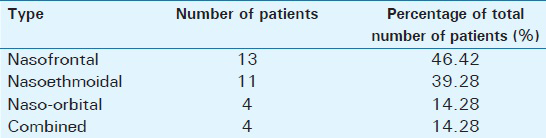
Fifty percent of the patients presented before the age of 3 years, with the youngest presenting on day 7. We had 2 patients (8%) presenting after 10 years. Rest of the patients (42%) presented between 3 and 10 years of age. Our study did not show any gender predominance, with both males and females being affected equally. Nasofrontal encephalocele was the most common type, seen in 13 (46.4%) patients. It was followed by nasoethmoidal type in 11 (39.2%) patients. The naso-orbital and the combined type were the least common with 4 (14.2%) patients each. Two patients had evidence of herniation of lateral ventricle along with brain tissue through the cranium into the encephalocele sac [Table 1].
Associated brain malformations
Corpus callosal agenesis with colpocephaly was the most common associated malformation in our study [Table 2]. It was noted in 12 patients. Archnoid cyst was the second common anomaly present in 10 patients. 6/10 archnoid cysts were hemispheric, 4/10 were inter hemispheric and 2/10 were located in posterior fossa.
Seven patients had evidence of hydrocephalus, of which five cases were due to the obstruction by large arachnoid cysts and two cases were due to aqueduct stenosis. Subdural collection was noted in 6 patients. In 4 patients it was subdural CSF collection due to hyperfunctioning of shunts and in 2 patients it was blood due to rupture of bridging cortical veins. Of these 6 patients, ventriculoperitoneal (VP) shunts were performed in 2 patients and cystoperitoneal shunt in 2 patients with large interhemispheric cysts causing mass effects. Cerebral cortical malformations with pachygyria-agyria complex was seen in 2 patients.
DISCUSSION
Encephaloceles occur due to the failure of surface ectoderm to separate from the neuroectoderm, resulting in a bony defect in the cranial and/or facial bones, which allows herniation of meninges or brain tissue. Encephaloceles occur in one of every 4000 live births and have no sex predilection.[3] According to location, these are occipital (75% of cases), sincipital (15%), or basal (10%).[3] Sincipital encephaloceles involve the mid-face and occur about the dorsum of the nose, orbits, and forehead. These sincipital encephaloceles are more common in South and Southeast Asian populations whereas the occipital encephaloceles are more common in the Western population.
The sincipital encephaloceles are further subdivided into nasofrontal, nasoethmoidal, and naso-orbital types. The nomenclature used for encephaloceles is based on the origin of their roof and floor; thus, for example, the roof and floor of frontonasal encephaloceles are the frontal and nasal bones, respectively.[3] Nasofrontal encephaloceles result from herniation through both the foramen cecum and the fonticulus frontalis and projecting along the nasal bridge between the nasofrontal sutures into the glabella (nasofrontal region). Nasoethmoidal encephaloceles occur when there is persistent herniation through the foramen cecum into the prenasal space and nasal cavity under the nasal bones and above the nasal septum (nasoethmoidal region). Moreover, naso-orbital types occur along the medial orbit at the level of the frontal process of the maxilla and the ethmoid-lacrimal bone junction (naso-orbital region).[145]
Affected children may present with nasal obstruction, mass in the frontal region, proptosis, or cerebrospinal fluid (CSF) leaks from ruptured encephalocele sac with recurrent meningitis. Sometimes, patients may also present with seizure due to associated cortical migration anomalies. The prognosis for the sincipital encephalocele patients is generally good and is usually associated with normal intelligence and motor development.[6]
Surgery is the best treatment option for encephaloceles, and MRI is the choice of imaging modality for defining the contents of an encephalocele prior to surgery.[2] High-resolution CT may also be used to display the bone anatomy, but the intracranial extension is best defined with MRI. The extent of cerebral tissue in an encephalocele is also better defined with MRI, which aids in prognosis and surgical planning. MRI also best depicts associated intracranial anomalies.[2] The aim of the radiologist is to precisely define the type of the encephalocele; delineate the size, contents, extension; and identify associated anomalies.
There are often significant associated intracranial anomalies, including intracranial cysts, complete/partial corpus callosal agenesis, interhemispheric lipomas, facial clefts, and migration anomalies. This study was undertaken to analyze the associated anomalies with sincipital encephaloceles. Unlike other varieties of neural tube defects, anterior encephaloceles are postneurulation defect. Earlier studies postulated theories such as adhesive theory, which suggest failure of mesodermal migration into midline leading to herniation of the brain matter and resulting failure of closure of anterior neuropore.[7] As corpus callosum forms near the site of final closure of anterior neuropore, many of these patients have associated corpus callosal agenesis which was also observed in our series. Rapport et al., postulated that this condition may have several etiological factors because mesodermal abnormalities alone cannot account for the observed abnormalities.[8] Lemire et al., thought that anterior encephaloceles result from abnormal dedifferentiation, whereas some other studies suggest neuroectodermal abnormality.[910] From the array of associated malformations that we have observed in our series, we feel that multiple factors may be responsible for the etiology.
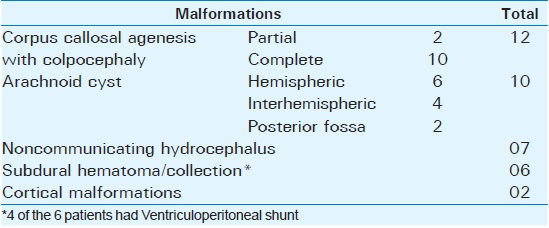
The most common associated malformation with sincipital encephaloceles is the agenesis or hypogenesis of the corpus callosum.[11] Corpus callosum is the largest cerebral commissure connecting neocortical areas and develops between 12 and 20 weeks of gestation. Development occurs from front to back with the exception of the rostrum which develops after the splenium. Callosal agenesis can be partial or complete. Imaging by CT and MR in complete callosal agenesis reveals widely separated and nonconverging lateral ventricles, disproportionately enlarged occipital horns (colpocephaly), and an elevated third ventricle which is continuous superiorly with the interhemispheric fissure [Figure 1]. In sagittal MR studies, corpus callosum, cingulate gyrus, and sulcus are not seen. Gyri on the medial hemispheric surface radiate outward from the high-riding third ventricle. In partial agenesis of corpus callosum, the splenium and rostrum are absent.
- 3-year-old male child with a swelling at nasal bridge, (a) axial computed tomography scan shows a nasofrontal encephalocele (*), (b and c) axial computed tomography sections show corpus callosal agenesis as evidenced by parallel running lateral ventricles with colpocephaly (arrow → in c).
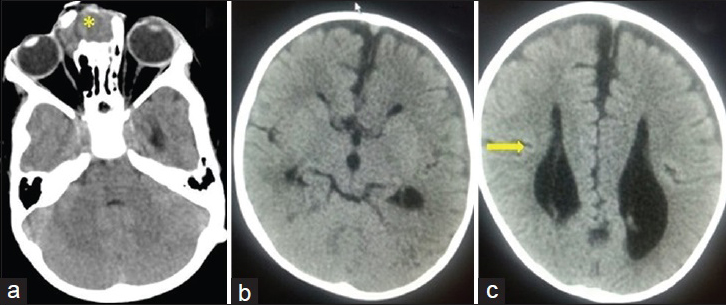
Arachnoid cysts are the most common type of the brain cysts. They are congenital lesions that occur as a result of the splitting of the arachnoid membrane. The cysts are extra-axial fluid-filled sacs, which are sharply marginated somewhat scalloped appearing lesions that parallel the CSF intensity on all sequences of MRI. Patients symptoms vary with size and location of archnoid cysts. Some suprasellar cysts become very large [Figures 2 and 3] and cause obstructive hydrocephalus. The arachnoid cysts, particularly the interhemispheric cysts, are usually associated with corpus callosal agenesis.[12]
- 2-year-old male child with a forehead swelling, (a) axial computed tomography bone window shows nasoethmoidal and naso-orbital type of encephalocele (*). (b) Axial, (c) coronal and (d) sagittal computed tomography sections show associated large hemispheric arachnoid cyst (arrow→). (b) Axial CT section also reveals the parallel orientation left lateral ventricle (upward arrow ↑) suggestive of corpus callosal agenesis.
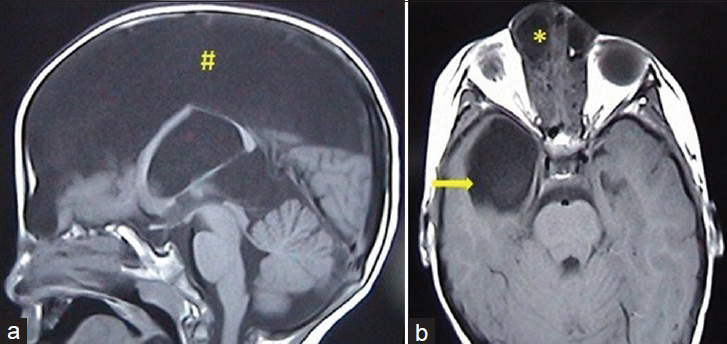
- 2-year-old female child with swelling at nasal bridge, (a) sagittal T1-weighted image shows a large interhemispheric arachnoid cyst (#). (b) Axial T1-weighted image in another patient with nasoethmoidal encephalocele (*) shows an arachnoid cyst in right temporal fossa (arrow→).
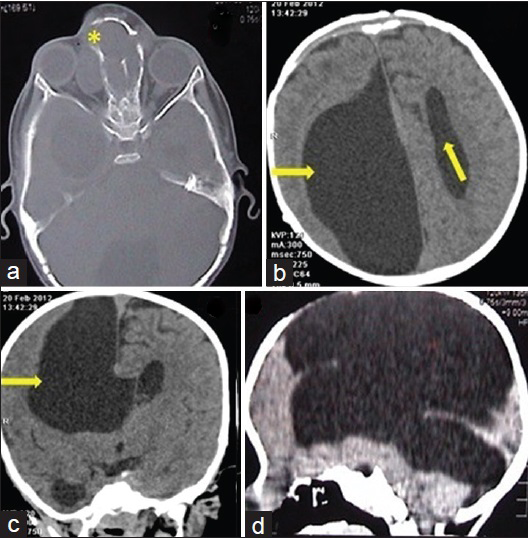
In our series, subdural collection was noted in six patients. Of the six patients four had subdural CSF collection and it was thought to be due to hyperfunctioning of the shunts [Figure 4], (two had been operated with ventriculo-peritonial shunt for obstructive hydrocephalus and in the other two, ventricular catheter of the shunt was placed in the large interhemispheric cysts i.e. cysto-peritoneal shunt which caused mass effects). Other two patients had small subdural hematomas probably due to rupture of bridging cortical veins around the herniation.
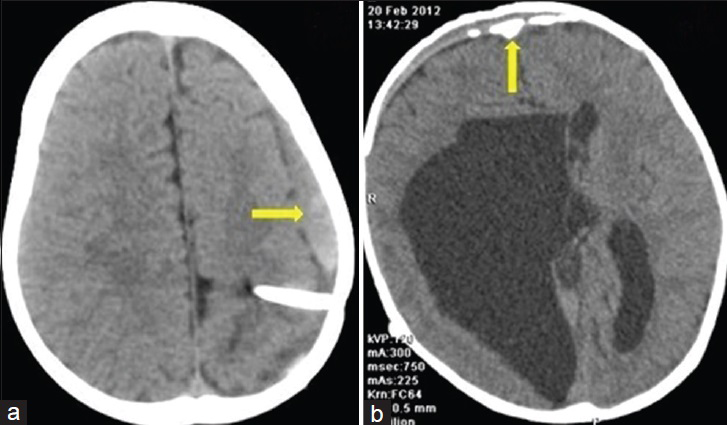
- 2-year-old female child with forehead swelling, (a) axial computed tomography section shows left subdural collection (arrow→) in a patient with ventriculoperitoneal shunt. (b) Axial computed tomography section in another patient with a large arachnoid cyst showing bilateral frontal subdural collection (arrow) with calcification of the arachnoid membrane.
Agyria-pachygyria complex is a defect in migration of cerebral neurons, resulting in failure of cortical gyri to develop [Figure 5]. Better imaging techniques in recent times have improved its diagnosis.[6] The extent, distribution, and detailed structure of agyria-pachygyria vary widely, and the clinical features are accordingly very diverse. Rather than one entity, pachygyric cortical abnormalities form a broad spectrum that raises different clinical and genetic problems.[13] This complex can be of generalized/bilateral or localized/unilateral gyral malformations. Generalized seizures with increased incidence of spastic quadriparesis and microcephaly are associated with the generalized/bilateral type, whereas partial seizures are more common in localized/unilateral gyral malformations and hemiparesis is the most frequent neurologic deficit. Patients with bilateral or generalized gyral anomalies have poor prognosis for outcome of epilepsy and neurologic disability. The recognition of these lesions with high-resolution techniques of MRI is important for planning proper treatment and genetic counseling.[14]
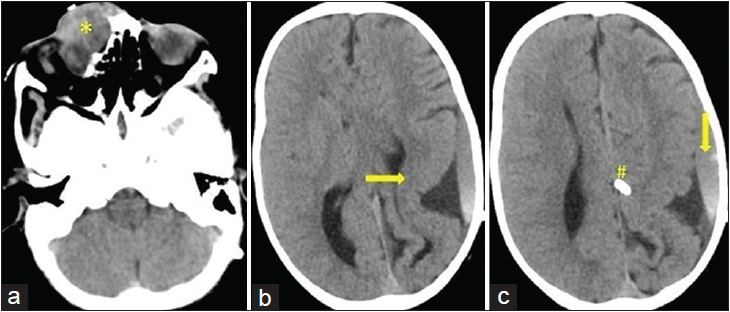
- 4-year-old child presented with swelling over the nose and seizure, (a) axial computed tomography scan shows nasofrontal type of encephalocele (*) with mild orbital extension. (b) Axial computed tomography section also shows agyria and pachygyria complex involving left parietooccipital lobe (arrow →) with corpus callosal agenesis. (c) Higher axial computed tomography section also shows ventriculoperitoneal shunt (#) in interhemispheric fissure with left subdural collection (arrow).
Limitation
We could not perform MRI in many cases, which is the investigation of choice due to cost constraints.
CONCLUSION
Encephaloceles are often associated with significant intracranial anomalies, with agenesis of corpus callosum being the most common. The presentation of the patients may vary depending on the associated brain malformations. Hence, a precise analysis of each case is necessary to recognize the associated malformations and establish the prognosis and risk of recurrence. The recognition of these lesions is important for planning proper treatment and counseling.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2016/6/1/20/183040
REFERENCES
- Lumps and bumps on the head in children: Use of CT and MR imaging in solving the clinical diagnostic dilemma. Radiographics. 2004;24:1655-74.
- [Google Scholar]
- Midface: Embryology and congenital lesions. In: Som PM, Curtin HD, eds. Head and Neck Imaging (3rd ed). St. Louis: Mo: Mosby; 1996. p. :3-60.
- [Google Scholar]
- The child with a cephalocele: Etiology, neuroimaging, and outcome. Childs Nerv Syst. 1996;12:540-50.
- [Google Scholar]
- Agyria-pachygyria and pachygyria in children. Contribution of imaging. Arch Pediatr. 1994;1:551-60.
- [Google Scholar]
- Normal and Abnormal Development of the Human Nervous System. Hagerstown, MD: Harper and Row; 1975. p. :421.
- [Google Scholar]
- A morphological classification of sincipital encephalomeningoceles. J Neurosurg. 1972;36:201-11.
- [Google Scholar]
- Sincipital encephalocele with corpus callosum agenesis and intracranial lipoma: A case report. India J Radiol Imaging. 2005;15:507-10.
- [Google Scholar]
- The agyria-pachygyria complex: A spectrum of cortical malformations. Brain Dev. 1991;13:1-8.
- [Google Scholar]
- Agyria-pachygyria complex: MR findings and correlation with clinical features. Pediatr Neurol. 2004;30:16-23.
- [Google Scholar]






