Translate this page into:
Roadmap to success: Blueprint for enterprise-wide deployment of a point-of-care ultrasound platform, inclusive of governance, policy, education, credentialing, and quality assurance

*Corresponding author: David Waldman, Department of Imaging Sciences, University of Rochester, Rochester, New York, United States. david_waldman@urmc.rochester.edu
-
Received: ,
Accepted: ,
How to cite this article: Waldman D, Pino C. Roadmap to success: Blueprint for enterprise-wide deployment of a point-of-care ultrasound platform, inclusive of governance, policy, education, credentialing, and quality assurance. J Clin Imaging Sci. 2024;14:35. doi: 10.25259/JCIS_96_2024
Abstract
Point-of-care ultrasound (POCUS) has emerged as a cost-effective diagnostic tool that significantly augments physical examinations. Positioned as an extension of traditional examination methods, particularly appealing to the upcoming generation of clinicians, it holds promise in potentially replacing the stethoscope in various medical assessments and procedures. The University of Rochester is deploying 2500 POCUS machines, enhancing compliance for image storage and documentation. Halfway through our 4-year deployment plan, we will discuss our governance structure, educational initiatives, and credentialing strategies. While POCUS adoption has seen organic growth over the past decade, our aim is to implement a comprehensive strategy ensuring adherence to established protocols for image storage and documentation. At present, we have successfully deployed 789 probes, with integration across 64 departments or divisions into our IT platform. Notably, this implementation has resulted in a remarkable 116% increase in hospital charges, underscoring the tangible impact of POCUS integration. However, achieving compliance and education among established providers has proven to be challenging.
Keywords
Point-of-care ultrasound
Enterprise
Compliance
Governance
INTRODUCTION
Ultrasound, revered for its cost-effectiveness and portability, has emerged as a promising imaging modality poised to enhance the efficiency of diagnosis of various diseases thus improving clinical outcomes. Lung point-of-care ultrasound (POCUS), for instance, has garnered acclaim through multiple studies showcasing its superior sensitivity and specificity in detecting pneumonia compared to the traditional “gold-standard” of chest X-ray.[1-4] Similar advantages extend to the detection of gallbladder disease, ascites, effusions, or renal stones.[5-10] Within our institution, there is a firm belief in the transformative potential of this technology to not only reduce overhead costs but also enhance the efficiency of medical care.[11] This program aims to outline the deployment, governance, and educational strategies for integrating POCUS across our healthcare enterprise.
MATERIAL AND METHODS
In January 2022, the University of Rochester Medical System initiated a comprehensive enterprise-wide deployment of a new POCUS platform. Over the course of 4 years, more than 2500 handheld ultrasound probes will be distributed across both inpatient and outpatient settings, available to students, nurses, and healthcare providers alike. Concomitantly, existing POCUS machines are being integrated into the same IT platform to enhance overall institutional compliance with image retention and documentation protocols. The Butterfly Network (Butterfly Network Inc. Burlington, MA) was chosen as our primary probe and IT Vendor. The IT platform uses an encounter-based workflow. The IT infrastructure is shown in Figure 1. They were chosen for their innovative probe design and ease of integration into existing IT systems. This platform allows POCUS machines to upload images into the cloud once credentialed providers document their images and finding. On report signature, the images and documentation are downloaded to our enterprise archive and Electronic Medical Record (EMR). The probe design uses a tunable digital chip comprised of 9000 programmable microsensors. This technology allows for a single probe to have a wide variety of uses, in contrast to the majority of POCUS vendors, who use probes with piezoelectric crystals resulting in the need for multiple probes per system to cover the variety of use cases. Across the country, there is significant variability in image storage, viewing, billing, and documentation. It is our goal to create a standardized system for all of the above components where all images become part of the medical record with all patient facing staff having viewing availability.
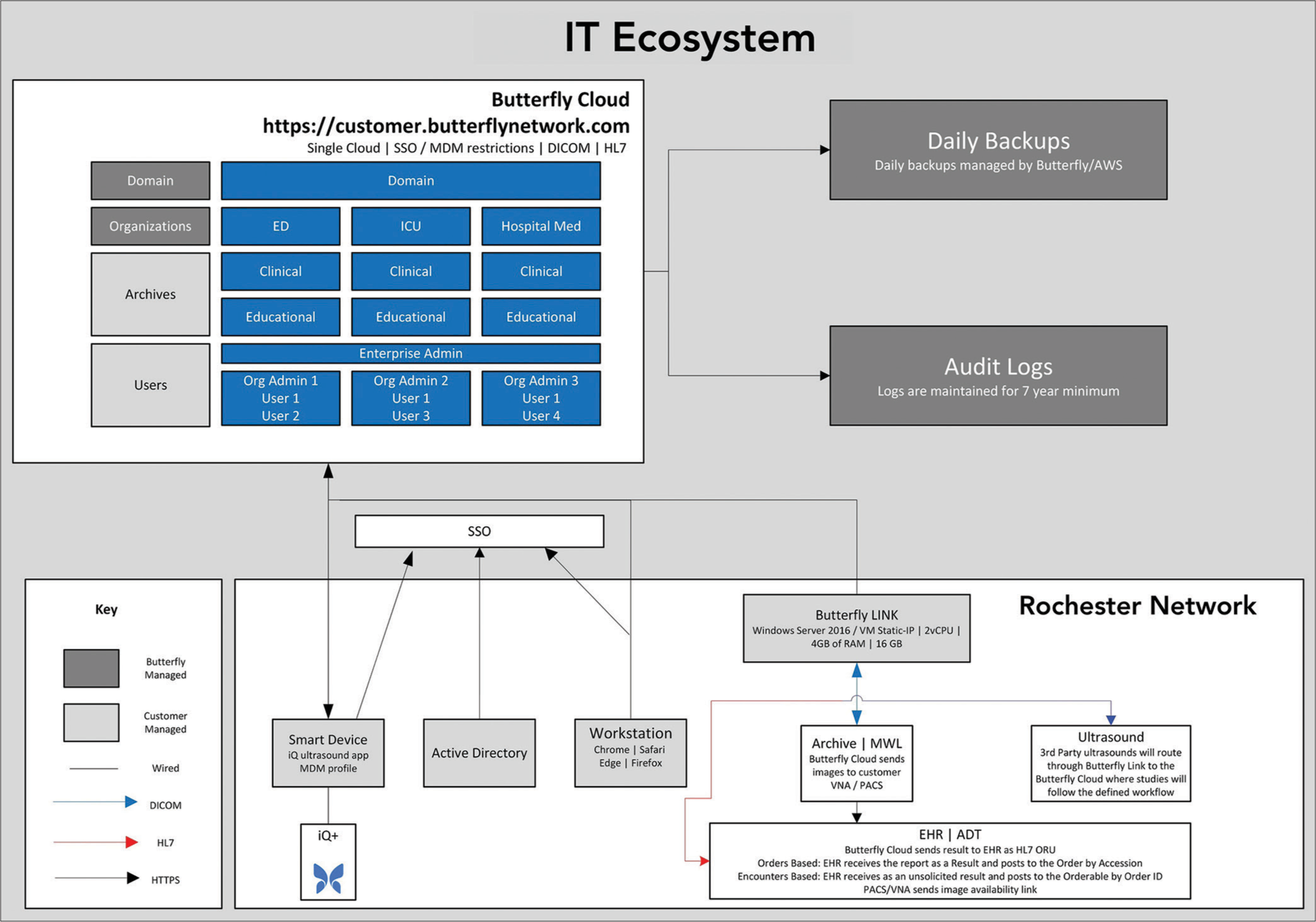
- University of Rochester Medical Center (URMC)/point-of-care ultrasound data flow. Initially, there was one link server; however, data throughput was not acceptable. The data were broken up into Digital Imaging and Communications in Medicine (DICOM) and Interface engine (HL7).
Governance
The institution devised an encompassing governance strategy, centered around the clinical council as its overarching body. Comprising representation from physicians, advanced practice providers, nurses, pharmacy, quality assurance (QA), and legal counsel, this appointed council was tasked with establishing comprehensive guidelines. These guidelines were modeled after the The American Institute of Ultrasound in Medicine (AIUM)[12] and American College of Emergency Physicians (ACEP)[13] recommendations. Specialty use cases dictate types of examinations. Given that variability, POCUS privileging was left to individual departments with the institution dictating minimal standards. During the initial months, a new institutional point-of-care policy was meticulously crafted. This policy delineated clear guidelines and responsibilities to individual departments while maintaining centralized oversight from the program. It covered crucial aspects such as credentialing, QA, infection control, communication protocols, documentation standards, and image retention policies. While some departments had policies already in existence, streamlining a process across the enterprise fostered a more unified and consistent program. Credentialing was granted to a POCUS panel excluding comprehensive cardiac, obstetrics (OB), and breast ultrasound.
Education
Establishing a structured program with designated leadership was imperative to drive the process, ensure quality review, mentor participants, maintain compliance, and foster ongoing education. The director and assistant director of the institution’s POCUS program bear the responsibility for orchestrating the day-to-day operations to ensure the program’s overall success. Leadership is, further, tasked with equipment maintenance, ensuring the economic viability of the program, and providing development and mentorship opportunities for less experienced clinical sonographers within the organization.
Recognizing the need for widespread education spanning beyond medical students, the most suitable location for housing such initiatives was identified as the Center for Experiential Learning. This space offers excellent resources for simulation, facilitating comprehensive training opportunities. In addition, resources from the School of Nursing have been tapped into to further enrich educational endeavors, including their state of the art facility and invested educators and leadership. The medical school redesigned their 1st and 2nd year curriculum’s where POCUS was encorporated into their problem-based learning courses.
Technology and development
To enhance workflow efficiency and optimize probe utilization, a collaborative provider and nurse workgroup was formed. This group collaborates with vendors to tailor hardware requirements, thereby enhancing patient care delivery. A crucial lesson learned underscores the importance of integrating innovative technology seamlessly into existing workflows.
Quality
Efforts to bolster quality initiatives are directed toward individual departments. Initial quality programs are centrally orchestrated to educate departments on credentialing and ongoing QA endeavors. Task forces are established to devise appropriate use cases and mechanisms for monitoring quality. Quality is measured both by image quality (is the study of high enough quality to answer a specific clinical question) and image interpretation. Feedback is given to the provider in both a numerical score and a written assessment.
Nursing
Two primary nursing initiatives have been launched focusing on POCUS applications for bladder scanning and ultrasound-guided IV placement. Nursing is a driving force within the enterprise, and they need access and training to top-tier technology to provide the highest level of care to their patients. Crafting new policies and developing educational platforms were necessary for these initiatives to flourish. It took over 12 months to finalize a new bladder scanning policy. The IV placement policy continues to be a work in progress with education and proficiency being the main drivers.
Billing
Close collaboration with individual departments has been pivotal in understanding their unique billing workflows. Where feasible, automation of billing processes has been implemented. Given the variability in billing practices across departments, individualized testing is imperative for each department’s billing system.
RESULTS
Medical school
The medical school curriculum underwent a significant overhaul to incorporate POCUS into the majority of their problem-based learning classes. As of the latest update, scanning sessions for the classes of 27, 26, and 25 totaled 2490, 1752, and 4307, respectively, with an average class size of approximately 103 students.
Clinical enterprise
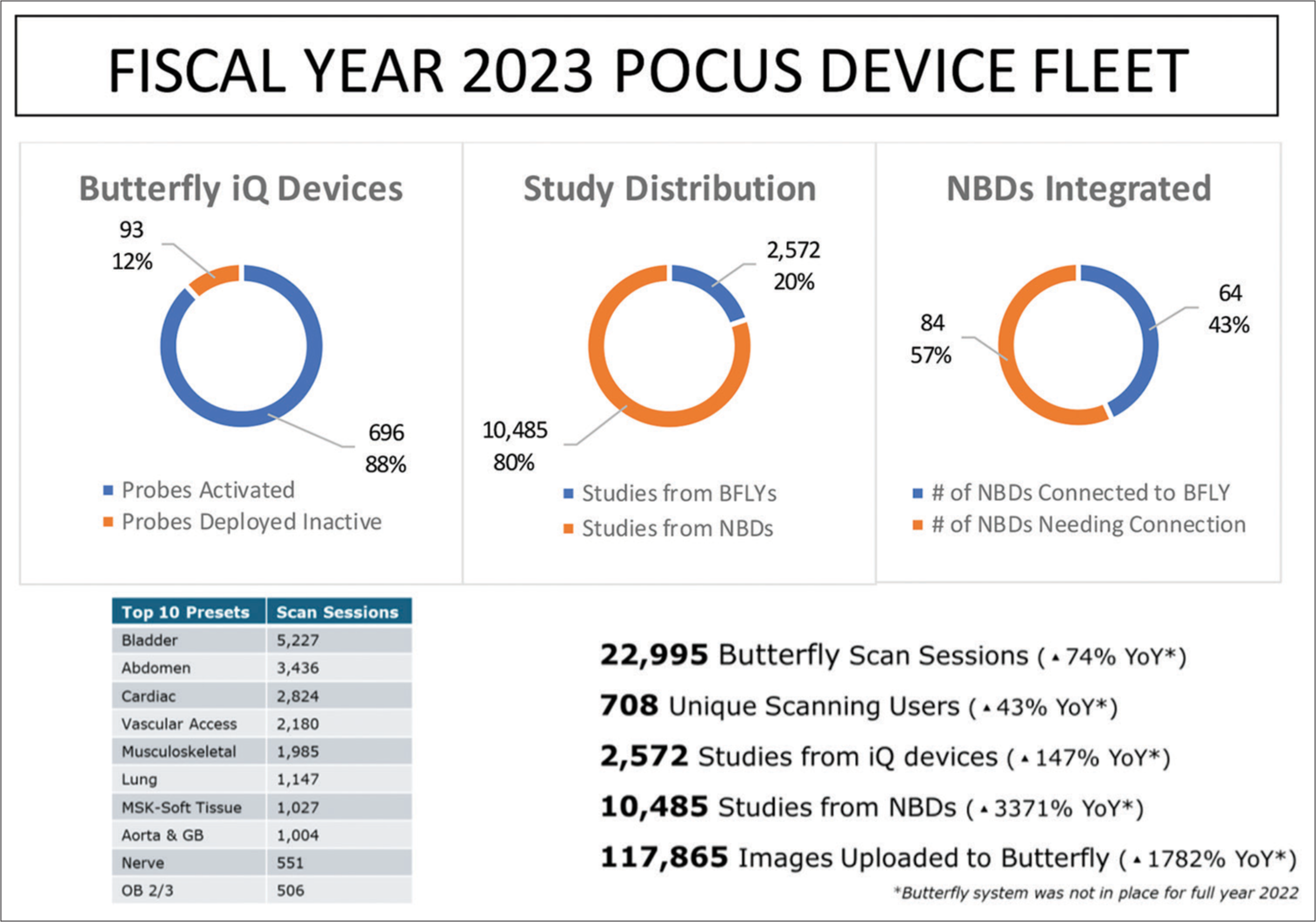
Deployment of 789 probes resulted in 49,492 scanning sessions by 964 unique users across 64 live departments. A total of 1129 study authors contributed to 175,197 images with 19,399 studies created and 15,524 finalized reports. Notably, 9802 studies underwent QA centrally or within departments [Table 1]. In 2023, scanning sessions surged by 74% compared to the previous year, accompanied by a 147% increase in studies uploaded from Butterfly devices and a remarkable 1782% surge in images uploaded from non-Butterfly devices. Hospital charges experienced a 38% rise in the Emergency Department (ED) and a staggering 217% surge from https://www.acep.org/siteassets/new-pdfs/policy-statements/ultrasound-guidelines--emergency-point-of-care-and-clinical-ultrasound-guidelines-in-medicine.pdfnon-ED (Both Butterfly and non-Butterfly https://www.acep.org/siteassets/new-pdfs/policy-statements/ultrasound-guidelines--emergency-point-of-care-and-clinical-ultrasound-guidelines-in-medicine.pdfutterfly) machines ([Figures 2 and 3] depict data through March 2024). Table 1 demonstrates data from fiscal year 2023. Overall, this equates to a total increase of 116% in total hospital charges. The increase in the number of images uploaded stems from the ability to have a mechanism of image storage through the new IT platform that was created. All patient facing staff with EMR priveledges has image access through our enterprise viewer.
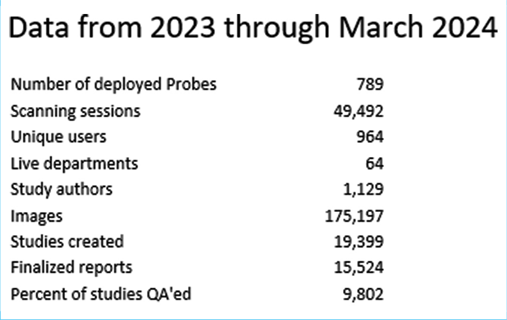 |
- 2023 deployments of US probes with current utilization. (NBD: Non-Butterfly devices, POCUS: Point-of-care ultrasound.)
- There has been a significant increase in billing departments. There has been a remarkable increase of 217% of non-ED billing. (POCUS: Point-of-care ultrasound)
Operational
A plan has been developed to operationalize issues through the IT help desk, addressing departmental onboarding and probe/device concerns. However, full implementation of the institutional policy has been hindered by the incomplete integration of existing ultrasound machines into the POCUS network. This is mostly an issue with provider acceptance of workflow change. It also has to do with a fear of legal issues should a finding be missed.
Initially, a collaborative tool was developed with Butterfly to assess program maturity. As an institution, we conducted evaluations both before and after program initiation across various domains: Education, credentialing, EMR integration, governance, leadership, billing, and rates of adoption. Tables 2 and 3 outline the program’s status pre- and post-initiation, revealing significant early maturation.
| Ultrasound Maturity Assessment 2022 | |||||
|---|---|---|---|---|---|
| Area | Level I | Level II | Level III | Level IV | Level V |
| Devices | Only radiology performed ultrasound | Limited access to shared devices across departments | One device available in select departments | Multiple devices available in select departments | Every provider has access to a device |
| Education | No institution supported education | Individual providers at off-site workshops | Occasional on-site workshops/FOAMED | Limited hands-on training; access to virtual ultrasound education | Access to extensive in-person and virtual ultrasound education |
| Credentialing | No standard credentialing or privileging | Manual QA/QI tracking in select departments | Automated QA/QI tracking in selected departments | Automated QA program with tracking to selected department requirements | Automated QA program with tracking across system |
| EMR Integration | No POCUS performed or integrated for clinical use | 25% of clinical exams are fully documented in patient chart eligible for reimbursement | 50% of clinical exams are fully documented in patient chart eligible for reimbursement | 75% of clinical exams are fully documented in patient chart eligible for reimbursement | 100% of clinical exams are fully documented in patient chart eligible for reimbursement |
| Governance | No documented policies | Documented policies in select departments with limited compliance | Documented policies in select departments with moderate compliance | Documented system-wide policies in moderate compliance | Documented system-wide policies with full compliance |
| Leadership | No defined leadership | One or more POCUS leaders | Volunteer POCUS Director in limited specialties | Funding and training for POCUS Director in limited specialties | Funding and training for POCUS Director for each specialty; system Director |
| Clinical Outcomes | No clinical benefit realized from POCUS | Clinical benefit from limited users | Clinical benefit from moderate adoption | One or more clinical POCUS initiatives | Measurable clinical benefit metrics across system |
| Billing | No exams submitted for reimbursement | 25% of billable studies submitted | 50% of billable studies submitted | 75% of billable studies submitted | 100% of billable studies submitted |
| Rate of Adoption | <25% of potential users are utilizing POCUS | 25% of potential users are utilizing POCUS | 50% of potential users are utilizing POCUS | 75% of potential users are utilizing POCUS | 100% of potential users are utilizing POCUS |
QA: Quality assurance, QI: Quality improvement
| Ultrasound Maturity Assessment 2023 | |||||
|---|---|---|---|---|---|
| Area | Level I | Level II | Level III | Level IV | Level V |
| Devices | Only radiology performed ultrasound | Limited access to shared devices across departments | One device available in select departments | Multiple devices available in select departments | Every provider has access to a device |
| Education | No institution supported education | Individual providers at off-site workshops | Occasional on-site workshops/FOAMED | Limited hands-on training; access to virtual ultrasound education | Access to extensive in-person and virtual ultrasound education |
| Credentialing | No standard credentialing or privileging | Manual QA/QI tracking in select departments | Automated QA/QI tracking in selected departments | Automated QA program with tracking to selected department requirements | Automated QA program with tracking across system |
| EMR Integration | No POCUS performed or integrated for clinical use | 25% of clinical exams are fully documented in patient chart eligible for reimbursement | 50% of clinical exams are fully documented in patient chart eligible for reimbursement | 75% of clinical exams are fully documented in patient chart eligible for reimbursement | 100% of clinical exams are fully documented in patient chart eligible for reimbursement |
| Governance | No documented policies | Documented policies in select departments with limited compliance | Documented policies in select departments with moderate compliance | Documented system-wide policies in moderate compliance | Documented system-wide policies with full compliance |
| Leadership | No defined leadership | One or more POCUS leaders | Volunteer POCUS Director in limited specialties | Funding and training for POCUS Director in limited specialties | Funding and training for POCUS Director for each specialty; system Director |
| Clinical Outcomes | No clinical benefit realized from POCUS | Clinical benefit from limited users | Clinical benefit from moderate adoption | One or more clinical POCUS initiatives | Measurable clinical benefit metrics across system |
| Billing | No exams submitted for reimbursement | 25% of billable studies submitted | 50% of billable studies submitted | 75% of billable studies submitted | 100% of billable studies submitted |
| Rate of Adoption | <25% of potential users are utilizing POCUS | 25% of potential users are utilizing POCUS | 50% of potential users are utilizing POCUS | 75% of potential users are utilizing POCUS | 100% of potential users are utilizing POCUS |
POCUS: Lung point-of-care ultrasound, QA: Quality assurance, QI: Quality improvement, FOAMED: Free open access medical education.
Predictably, we encountered challenges in credentialing, departmental leadership, clinical outcomes, billing, and adoption rates. Given that many POCUS programs evolve organically, credentialing issues are not unexpected. https://www.acep.org/siteassets/new-pdfs/policy-statements/ultrasound-guidelines--emergency-point-of-care-and-clinical-ultrasound-guidelines-inmedicine.pdf https://www.acep.org/siteassets/new-pdfs/policy-statements/ultrasound-guidelines--emergency-point-of-care-and-clinical-ultrasound-guidelines-inmedicine.pdf
In the post-COVID era, health-care providers are exceptionally busy. Improving adoption rates necessitates seamless integration with clinical workflows and a clear demonstration of clinical outcomes. Without tangible outcomes, providers may view POCUS as an additional burden. It will take considerable time to establish robust research-driven clinical outcomes. Showcasing successful cases was demonstrated POCUS’s potential to improve diagnostic accuracy and patient outcomes. Engaging a single proficient provider within a practice encourages further adoption. In addition, ensuring medical students and residents are adept with the technology accelerates faculty engagement.
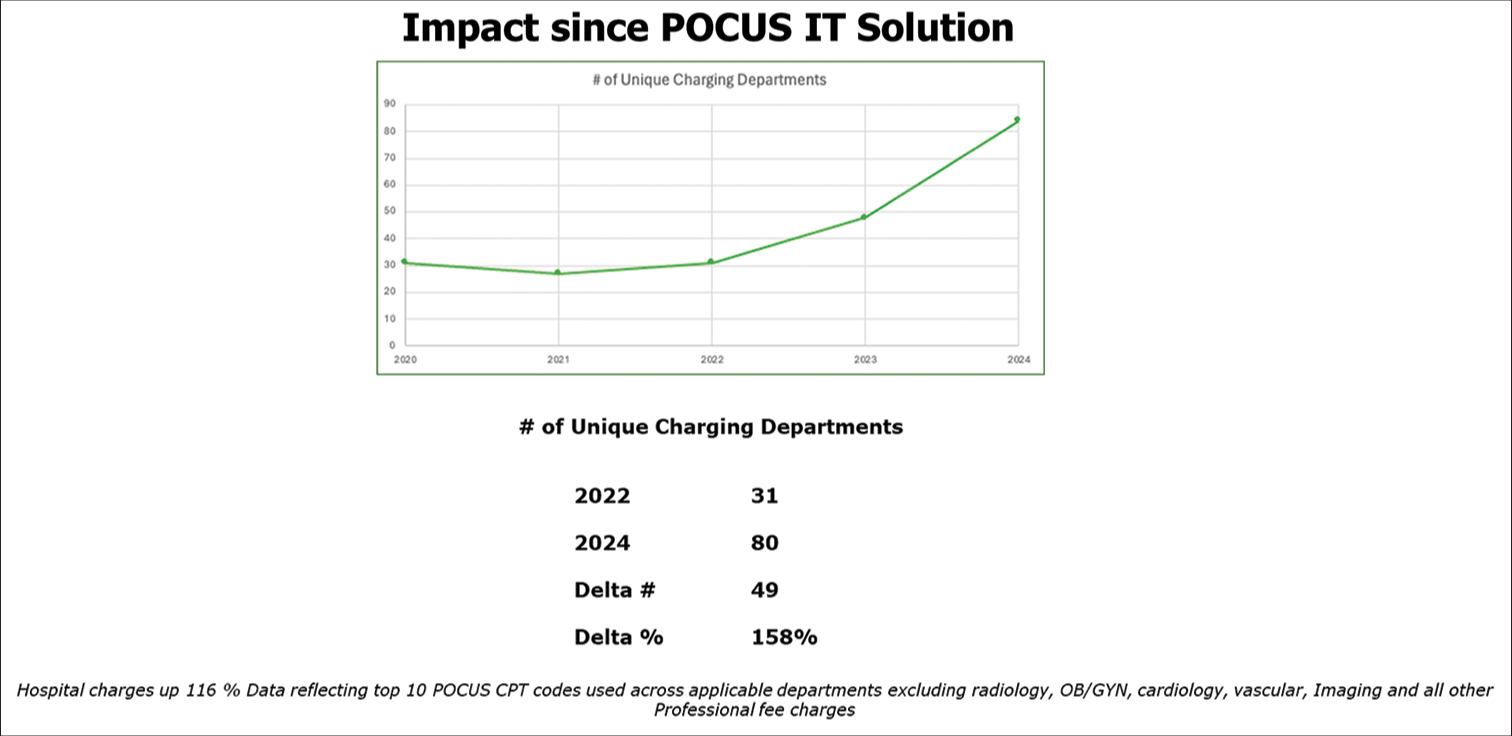
Providers’ concerns regarding legal implications and the paradigm shift from diagnostic imaging to an extension of the physical examination, particularly evident in primary care, underscore the need for robust education and clinical champions. Billing practices have also raised contention, resulting in suggestions for an enhanced billing model inclusive of POCUS within physical examination charges. While we have seen a remarkable increase in hospital charges [Figure 3], overall changes in healthcare have been predictably slow. As a program, we have chosen to highlight some of the documented clinical wins including early detection of bladder tumor, cholecystitis, pneumonia, pleural effusions, endocarditis, and fluid overload to name a few. These are documented on our institution’s intranet. A few image examples are displayed in Figure 4.
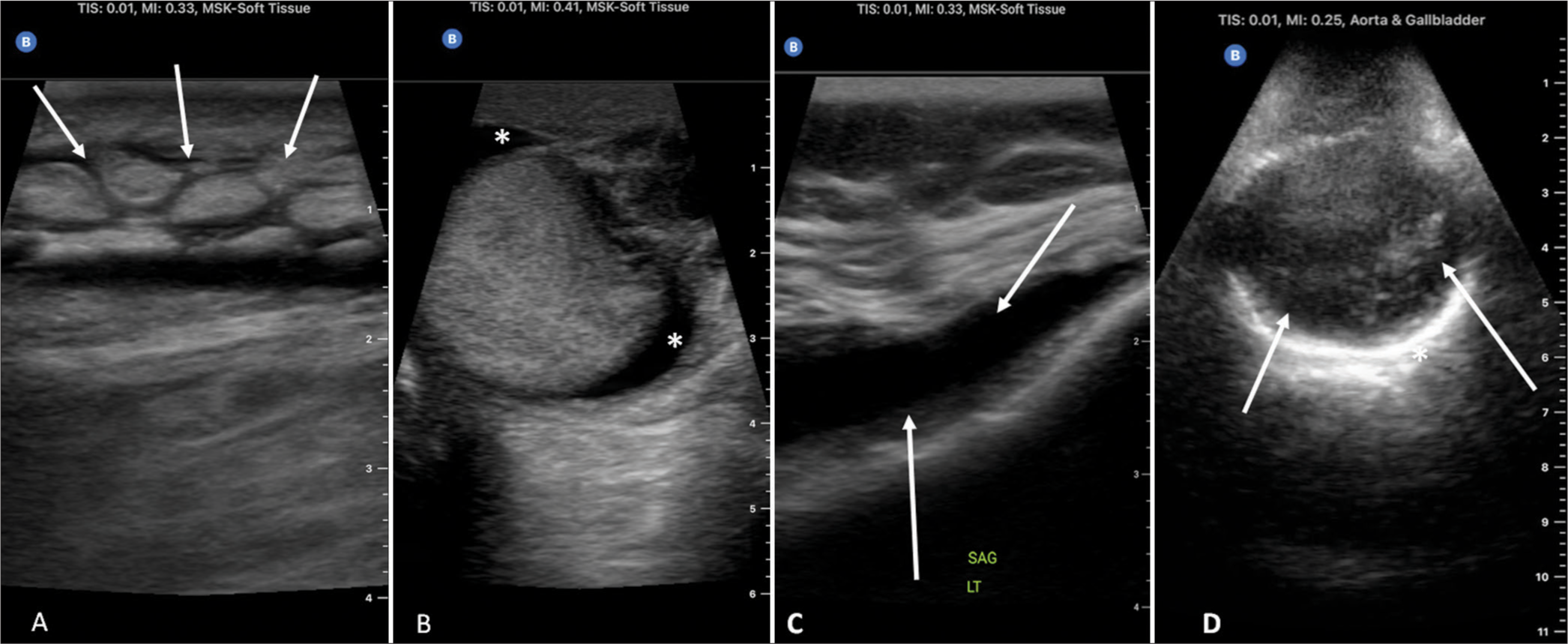
- Representative ultrasound images: (A) Cobblestoning in the right calf with arrows pointing to the edema in the soft tissue, (B) right testicular hydrocele with areas of fluid noted by the asteriks*, (C) left knee effusion with arrows pointing to the anechoic fluid pocket, and (D) abdominal aortic aneurysm with a calcified wall* and intramural thrombus denoted by the arrows.
Below, we delve into the progress made and challenges faced across multiple domains.
Education
As medical students now rotate through various clinics, preceptors have become much more engaged in US education. Educational approaches have evolved based on feedback, shifting toward provider-driven education, intensive care unit (ICU) and hospitalist teaching rounds, and virtual office hours. Feedback was collected through email, surveys, during departmental POCUS meetings, and in-person. Incorporating POCUS training into the School of Nursing Advanced Practice Provider (APP) program has yielded positive feedback and engagement. Medical students continue to push faculty to new levels. For instance, an orthopedic instructor has a student perform a shoulder US in their clinic before the provider appointment, comparing the results to a previously obtained MRI, leading to impressive correlations. Anticipated changes in practice patterns over the next several years are expected. Providers continue to ask for continuing education credits. We continue to work with the medical school to establish programmatic guidelines for continuing medical credit.
Credentialing
While some providers believe that they are credentialed to provide POCUS services, deficiencies have been eye-opening for both providers and departments. Streamlining the credentialing process has been a priority. Initially, the program centralized QA tasks, with eventual transition to departmental control as maturity is reached.
EMR integration
IT integration is straightforward, but operational workflow for providers has posed challenges, particularly for those accustomed to traditional ultrasound machines. Acceptance has been smoother for providers new to POCUS. Providers are now able to see clinical POCUS images alongside of all picture archiving and communication system images. This is inclusive of imaging, cardiology, vascular surgery, and OB/gynecology. Only providers who have credentialing privileges on their delineation of privileges are able to have connectivity to the EMR and PACS. Educational images remain in the cloud separate from the EMR and PACS for those providers working toward completing the credentialing process.
Governance
Our governance model continues to evolve, with the clinical council serving as the overarching governing structure. Subcommittees, including IT and operational, have been developed out of operational necessity. These subcommittees meet quarterly where program progress gets discussed.
Leadership
Departmental maturity varies greatly. The ED boasts a mature program, while the ICU lacks infrastructure despite incorporating POCUS into clinical practice. Significant efforts have been directed toward building program infrastructure, including education, credentialing, and QA. Some departments have established joint programs to enhance sustainability, such as nephrology partnering with medicine for a QA program.
CONCLUSION
Challenges persist in integrating POCUS seamlessly into existing workflows, especially among seasoned providers. Concentrating efforts on students, residents, and APPs has shown promise. Strategic planning and alignment with institutional EMR systems are crucial as seen in the home care nursing context. Providers express concerns over legal challenges and increased medical expenses emphasizing the importance of appropriate use and demonstrating cost-effectiveness through data.
Future efforts should focus on policy enforcement. Administration has not enforced the policy given that all the non-Butterfly devices are connected to the IT Platform. This work will conclude in the spring of 2025 allowing for policy enforcement. Providers will continue to work on credentialing. The most challenging issue with adoption rates stems around image storage and documentation. We continue to work with our vendor to streamline workflow. This appears to be more of an issue surrounding providers who previously preformed POCUS without image storage, documentation, or billing. The real value of the program surrounds improved and more efficient patient care. It will take significant longitudinal studies to ultimately define its value. As an institution, we are taking on an enterprise study to evaluate fluid volume across all phases of care.
The deployment of POCUS has significantly enhanced diagnostic capabilities and patient care despite challenges in adoption and workflow integration. Success hinges on ample resources and funding, coupled with centralized operational oversight initially, gradually transitioning to departmental control. Education and QA remain paramount throughout the process. Planning must account for extended timelines, with deployment and acceptance often taking twice as long as anticipated. Despite the obstacles, the potential benefits make POCUS integration a worthwhile endeavor with transformative implications for patient care.
Acknowledgments
We extend our sincere appreciation to Dr. Peter Weimersheimer and Ross Martin (Butterfly Network, Burlington MA) for their expertise and guidance to help shape and create the Ultrasound Maturity tool used in this document. It is our hope this tool will be used by other programs moving forward.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Systematic review and meta-analysis for the use of ultrasound versus radiology in diagnosing of pneumonia. Crit Ultrasound J. 2017;9:6.
- [CrossRef] [PubMed] [Google Scholar]
- Lung ultrasound for the diagnosis of pneumonia in adults: A systematic review and meta-analysis. Respir Res. 2014;15:50.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic performance of point of care ultrasound compared to chest X-ray in patients with hypoxia at a teaching hospital emergency department in Uganda. Afr J Emerg Med. 2023;13:61-7.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic accuracy of point-of-care lung ultrasonography and chest radiography in adults with symptoms suggestive of acute decompensated heart failure: A systematic review and meta-analysis. JAMA Netw Open. 2019;2:e190703.
- [CrossRef] [PubMed] [Google Scholar]
- Surgeon-performed point-of-care ultrasound for acute cholecystitis: Indications and limitations: A European Society for Trauma and Emergency Surgery (ESTES) consensus statement. Eur J Trauma Emerg Surg. 2020;46:173-83.
- [CrossRef] [PubMed] [Google Scholar]
- Utilization of point-of-care ultrasound as an imaging modality in the emergency department: A systematic review and meta-analysis. Cureus. 2024;16:e52371.
- [CrossRef] [Google Scholar]
- Point of care ultrasound bladder volume calculation on the acute medical unit. Acute Med. 2024;23:37-42.
- [CrossRef] [PubMed] [Google Scholar]
- The accuracy of point-of-care ultrasound (POCUS) in acute gallbladder disease. Diagnostics (Basel). 2023;13:1248.
- [CrossRef] [PubMed] [Google Scholar]
- Earlier point-of-care ultrasound, shorter length of stay in patients with acute flank pain. Scand J Trauma Resusc Emerg Med. 2022;30:29.
- [CrossRef] [PubMed] [Google Scholar]
- Emergency physician-performed point-of-care ultrasound of a renal mass. Cureus. 2023;15:e48547.
- [CrossRef] [Google Scholar]
- Point of care ultrasonography as the new “Laennec Sthetoscope”. World J Nephrol. 2024;13:90542.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound-training guidelines. 2024. Available from: https://www.aium.org/resources/training-guidelines [Last accessed on 2023 Mar 23]
- [Google Scholar]
- Physicians- Ultrasound guidelines: Emergency point-of-care and clinical ultrasound guidelines in medicine. 2024. Available from: https://www.acep.org/siteassets/new-pdfs/policy-statements/ultrasound-guidelines--emergency-point-of-care-and-clinical-ultrasound-guidelines-in-medicine.pdf [Last accessed on 2023 Mar 23]
- [Google Scholar]






