Translate this page into:
Retroperitoneal anatomy with the aid of pathologic fluid: An imaging pictorial review

*Corresponding author: Carlos Ignacio Gonzalez Baerga, Department of Radiology, University of Florida-Jacksonville, Jacksonville, Florida, United States. carlos.gonzalezbaerga@jax.ufl.edu
-
Received: ,
Accepted: ,
How to cite this article: Montanarella M, Gonzalez Baerga CI, Menendez Santos MJ, Elsherif S, Boldig K, Kumar S, et al. Retroperitoneal anatomy with the aid of pathologic fluid: An imaging pictorial review. J Clin Imaging Sci. 2023;13:36. doi: 10.25259/JCIS_79_2023
Abstract
The retroperitoneum, a complex anatomical space within the abdominopelvic region, encompasses various vital abdominal organs. It is compartmentalized by fascial planes and contains potential spaces critical in multiple disease processes, including inflammatory effusions, hematomas, and neoplastic conditions. A comprehensive understanding of the retroperitoneum and its potential spaces is essential for radiologists in identifying and accurately describing the extent of abdominopelvic disease. This pictorial review aims to describe the anatomy of the retroperitoneum while discussing commonly encountered pathologies within this region. Through a collection of illustrative images, this review will provide radiologists with valuable insights into the retroperitoneum, facilitating their diagnostic proficiency to aid in appropriate patient clinical management.
Keywords
Retroperitoneum
Retroperitoneal spaces
Extraperitoneal spaces
Pathologic fluid
Anatomy
INTRODUCTION
The retroperitoneum is a space within the abdominal cavity between the posterior parietal peritoneum and the transversalis fascia of the posterior abdominal wall.[1-3] It is bounded superiorly by the diaphragm and inferiorly by the pelvic inlet. Abdominal organs are retroperitoneal if not suspended by mesentery and are within this space.[4] The retroperitoneum contains further sub-compartments delineated by fascial planes. These fascial planes allow the spaces to communicate with the pelvis.[5] Organs and vessels within the retroperitoneum are labeled as primary or secondary retroperitoneal. Primary retroperitoneal organs remain in the retroperitoneal space throughout the development.[4,6] Primary retroperitoneal structures include the kidneys, adrenal glands, ureters, abdominal aorta, and the inferior vena cava.[4,6] Secondary retroperitoneal structures were initially suspended by mesentery and, later in development, migrated to space. These structures include the pancreas, duodenum, and ascending/descending colon.[4,6]
Pathologies such as trauma, infection, pancreatitis, and neoplasm may manifest within these retroperitoneal spaces. For a radiologist, it is essential to clearly understand such structural anatomy and the communication between spaces within the retroperitoneum. In this article, we describe the interpretation of imaging studies and disease extent concerning these anatomical compartments.
BASIC RETROPERITONEAL EMBRYOLOGY
First, a brief discussion of retroperitoneal embryology is warranted to understand fluid’s anatomic intricacies and distribution within the retroperitoneal spaces. It is essential to consider that the retroperitoneum forms in multiple discrete fascial layers representing opposed embryonic mesentery.[7-9] The outermost layer of a developing embryo, the primary body wall, is formed by mesenchyme, which develops the paraspinal muscles, vertebral bodies, and the psoas musculature.[7] Transversalis fascia and fat layer these structures anteriorly.
Renal tissue initially develops within the first 4 weeks of gestation.[10] The kidneys originate at the sacral level in the embryo, ascend superiorly, and rotate medially to their adult positioning.[10] Due to this movement pattern, the fascia surrounding the kidneys takes on a tapered cone shape. This fascia fuses posterolaterally at the retroperitoneal fat.[7] At this point in development, the perirenal and posterior pararenal spaces (PPSs) are formed. Each space and its contents will be described in their respective sections below. A potential area is formed between these fused layers termed the retrorenal plane.[7,8,11]
The embryologic development of the gut and dorsal explains how several retroperitoneal spaces are formed. The anterior pararenal space (APS) and retro mesenteric plane result from the folding and rotation of the duodenal, pancreatic, and colon mesentery.[7] The developmental rotation of the colon and its mesentery create the APS, lateroconal fascia, and a potential space called the anterior interfascial plane. Further, discussion of this process is beyond the scope of this article.
RETROPERITONEAL COMPARTMENTS
The retroperitoneum is divided into three main compartments, termed the perirenal space (PRS), the APS, and the PPS [Figure 1]. Each compartment is described in its section below, focusing on fluid collections and their potential etiologies.
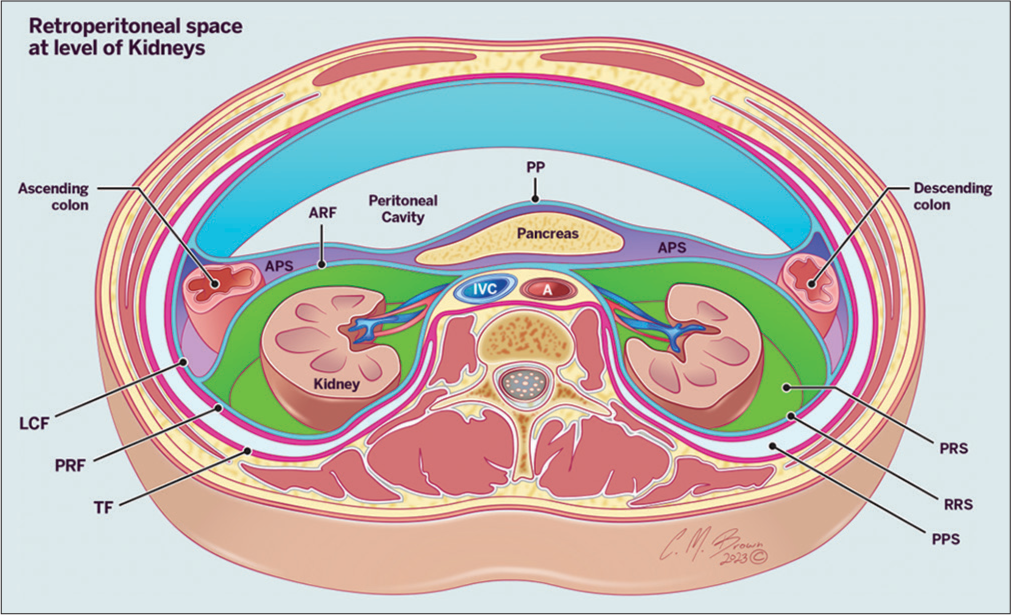
- Illustration of the retroperitoneum at the level of the kidneys demonstrating the retroperitoneal compartments (PP: Parietal peritoneum, APF: Anterior pararenal fascia, LCF: Lateroconal fascia, APS: Anterior pararenal space, PRS: Perirenal space, PPS: Posterior pararenal space, RRS: Retrorenal space, PPS, TF: Transversalis fascia).
PRS
The PRSs are the largest of the three retroperitoneal compartments. The anterior and posterior renal fascia bounds this space, with dense collagenous sheaths surrounding the structures within the space.[1,12-14] Superiorly, the bare area of the liver bounds the space and inferiorly opens into the pelvic retroperitoneal spaces[5] [Figures 1 and 2].

- Illustration of the retroperitoneal space at and below the level of kidneys.
Direct communication of the right and left PRS s is a controversial topic. Initially, it was thought that the two spaces were connected medially.[15-17] However, more recent literature demonstrated that the perirenal fascia also fuses medially, effectively creating an anatomical barrier between the two spaces.[11,18] The PRS contains the kidneys, adrenals, proximal ureters, hilar vessels, and perirenal fat.[2,13,19] The PRS is divided into small compartments and bridging septa by thin fibrous lamellae, which pierce the perirenal fat and connect the renal capsule to the anterior and posterior renal fascia.[7,20-22] Septa are continuous with interfascial planes and allow for the movement of pathologic fluid between the PRS s and fascial planes.[7]
Fluid collections within the PRS may be traumatic (hemorrhage and urinoma) or infectious [Figures 3-5]. A perinephric hematoma is typically described as a blood product confined within the anterior and posterior renal fascia.[19,23] Trauma is the most common cause of perirenal hemorrhage and can happen following blunt injury, penetrating injury, or iatrogenic, following lithotripsy, biopsy, or surgery.[24] Rarely, spontaneous perirenal hemorrhage may occur.[25,26] Urine leaks or urinomas occur following abdominal injury and result from disrupting the urinary collecting system.[27] Urine leaks result from 1% to 7% of renal injuries and over a quarter of patients with grade four renal injuries.[23,28-30]

- A 40 year old woman with sepsis. Computed tomography (CT) axial image at the level of the kidneys demonstrates a perirenal abscess (star) contained by the anterior (white arrow) and posterior (red arrow) perirenal fascia.

- A 49 year old man with blunt abdominal trauma. Computed tomography (CT) of the abdomen (a, c) axial, (b) sagittal reformatted images demonstrating injury to the bare area of the liver (white arrow) with superior perirenal hematoma (star) and adrenal hematoma (red arrow).

- A 40 year old man with acute flank pain. Contiguous axial abdomen computed tomography (CT) images (a, b) demonstrating a left subcapsular urinoma/hemorrhage (star) secondary to obstructing stone (red arrow).
Neoplasms encountered in this space are based on the organs or tissue that occupies it such as sarcomas, pheochromocytomas, renal angiomyolipomas, lymphoproliferative tumors, or metastatic disease.[31,32] Renal cell carcinoma can spread locally through perinephric fat and adjacent viscera and organs.[33] Benign tumors, such as myelolipomas, may be encountered in this space.[34]
APS
The APS contains six borders consisting of the posterior parietal peritoneum anteriorly, the anterior renal fascia posteriorly, the lateroconal fascia laterally, the inferior point of the renal cone inferiorly, and the moment in which the anterior renal fascia and the peritoneum meet is the superior border [Figures 1 and 2]. The APS contains the ascending and descending colon, the duodenum, and the pancreas.[35] Both pararenal spaces communicate behind the duodenum and pancreas. The pelvis is connected through the potential space between the parietal peritoneum anteriorly and the anterior renal fascia posteriorly along the path of the ureter.[2] No communication exists between the intraperitoneal spaces, but communication is present between the infrarenal space and other extraperitoneal spaces within the pelvis.[5]
Fluid collections are more commonly encountered and more accessible to visualize on the left side due to associated pancreatic disease of the tail, extending from the APS to a space between the laminae of the posterior renal fascia [Figures 6-8]. Collections on the right side tend commonly to be a sequela of pancreatitis or bowel perforation. These collections are challenging to identify.[22,36] Schwannomas may be encountered in the pararenal space, as per Liu et al., with a round or oval shape rather than a spindle.[37]

- A 63 year old man with hemorrhagic pancreatitis. Computed tomography (CT) abdomen axial image demonstrating an abscess in the anterior pararenal space with extension into the lateral conal space (star).

- A 65 year-old-man with complications from cardiac catheterization procedure. (a) Arterial angiogram and (b) axial computed tomography (CT) image of the abdomen demonstrating active extravasation from the right external iliac artery (red arrow). Hemorrhage is seen in the right anterior pararenal space (white arrow), which extends into the left anterior pararenal space (green arrow).

- A 39 year old man with acute pancreatitis. Contiguous computed tomographic (CT) abdomen axial images demonstrating inflammatory fluid in the left anterior pararenal space (red arrow), which extends along the root of the mesentery and mesocolon (white arrows).
PPS
The PPS is bordered by the diaphragm superiorly, the posterior renal fascia anteriorly, and the transversalis fascia posteriorly. The posterior renal fascia borders anteriorly to the PPS and lateroconal fascia [Figures 1 and 2]. The PPS extends to the pelvis by following the path of the ureter to the bladder and ends at the potential space between perivesical peritoneal folds. The space communicates with the preperitoneal fat along the lateroconal fascia that fuses with the parietal peritoneum. The PPS communicates to the femoral sheath, prevesical, APS, and PRS through the infrarenal space.
Fluid collections are rarely observed in this space. It is mainly composed of fat.[2,35] Hemorrhage may be encountered in patients with bleeding disorders by the femoral vessels on anticoagulation or catheterization procedures[22,38] [Figures 9 and 10]. Neoplasms may also be encountered in this space. Peng et al. reported a schwannoma located in the PPS.[39]

- A 40 year old man with Pott Disease. Abdominal computed tomography (CT) (a) axial and (b) sagittal images demonstrating a large iliopsoas abscess with extension into the posterior pararenal space (star). Also noted is a destruction of an adjacent vertebral body (red arrow).

- A 53 year old woman with pancreatitis. Abdominal computed tomography (CT) (a) axial and (b) sagittal images demonstrating inflammatory fluid in the posterior pararenal space (red arrow), which extends into the pelvic retroperitoneum (white arrow).
The posterior pararenal and previously described APS and PRSs communicate with the infrarenal space. The communication of this space and the subsequently explained interfascial planes allow pathologic fluid to spread into the pelvis.
Interfascial planes
As stated previously, the retroperitoneum can be divided into three main compartments. It is known that the perirenal fascia is single, multi-laminated structures. The capacity of this space is limited and, once overwhelmed with fluid, may communicate with the interfascial planes. The interfascial planes consist of the retro mesenteric, retrorenal, lateroconal, and a combined plane. These planes are connected with the perinephric bridging septa, through which pathologic fluids can spread.[2,40,41]
The retro mesenteric plane is along the midline between the APS and PRS. It extends superiorly on the right side up to the right inferior coronary ligament connecting to the liver hilum via the subperitoneal space of the hepatoduodenal ligament. On the left, it follows posteriorly to the tail of the pancreas, anteriorly to the fascia of the adrenal gland, and superiorly to the dome of the diaphragm, a posterior segment of the esophagus and phrenoesophageal ligament.[42] The plane is to be described with multiple communications that can eventually reach a trifurcation consisting of between the laminae of the anterior renal fascia, posterosuperior renal fascia, and lateroconal fascia. The surrounded PRS creates the lateroconal and posterior interfascial decompression planes.[2]
The retrorenal plane is a potential space between the PRS and PPS that communicates with the aorta and inferior vena cava.[2] The lateroconal interfascial plane is located between the layers of the lateroconal fascia and communicates the retro mesenteric with the retrorenal interfascial planes at their trifurcation.[20,42] There is a suggestion of an additional plane between the pararenal space and transversalis fascia called the subfascial plane, which allows a narrow communication with the retrorenal plane.[36] The combined interfascial plane is between the anterior and posterior renal fasciae. This potential space extends inferiorly along the psoas muscle and reaches the mesorectal interfascial plane or prevesical space.[42] The disease can spread from the abdominal retroperitoneum into the pelvis through this route.
Multiple pathologic entities can be observed along the fascial planes: necrotizing fasciitis, pancreatitis-related effusions, hematomas, urinomas, bowel inflammation, or perforation[42-44] [Figures 11 and 12].

- A 41 year old woman with perforated diverticulitis of the descending colon. Computed tomography (CT) abdomen axial image demonstrating air tracking in the retro mesenteric space (red arrow).

- A 37 year old man with acute pancreatitis. Computed tomography (CT) abdomen axial image demonstrating inflammatory fluid in the lateral conal plane (red arrow) communicating with the retro mesenteric (white arrow) and retrorenal (star) spaces.
In pancreatitis, inflammatory effusions may involve the interfascial planes and spread inferiorly into the pelvic retroperitoneum. Ishikawa, et al. created a classification that determined the computed tomography (CT) severity of pancreatitis using the concept of interfascial planes and explained the low position of the Grey-Turner sign with pancreatitis.[44] The Grey-Turner sign is spread from the APS to between the two leaves of the posterior renal fascia and lateral edge of the quadratus lumborum muscle.[45] The rupture of great vessels such as the aorta or inferior vena cava is more involved with the retrorenal interfascial planes or combined interfascial planes, but the retro mesenteric is less involved.[42] Thick retroperitoneal fascia may suggest retroperitoneal organ disease and an early manifestation of the checkmark sign is indicative of a severe medical condition.[46]
| Perirenal space | Hemorrhage Urinomas Abscess Hemangiomas Lymphomas Pheochromocytomas Renal carcinomas Liposarcomas |
| Anterior pararenal space | Neurogenic tumors Hematomas Pancreatic effusions Abscess Neurogenic tumors Fibroblastic tumor Adipocytic tumors |
| Posterior pararenal space | Hematomas Neurogenic tumors Fibroblastic tumor Adipocytic tumors |
| Interfascial planes | Necrotizing fasciitis Hematomas Urinomas Perforations Effusions Metastasis |
| Pelvic spaces | Hematomas Urinomas Effusions Colon cancer Bladder cancer Bladder ruptures Prostate cancer Uterine cancer Ovarian cancer |
Through periaortic and pericaval retroperitoneal lymph nodes, metastatic spread of malignant tumors may propagate to the perinephric space along the retro mesenteric and retrorenal planes. Not just metastasis, but primary infiltrating colonic tumors can spread across these planes due to their fused layers with the mesocolon. Pleural and transdiaphragmatic lymphatics provide an alternate route for metastatic disease to the perinephric space through these interfascial planes.[42]
Pelvic spaces
The pelvis is the compartment between the peritoneum and the transversalis fascia within the extraperitoneal space.[47] The pelvic space consists of two compartments, anterior and posterior, separated by the rectovesical fascia of Denonvillier in males or rectovaginal fascia in females.[47,48] The anterior pelvic space is divided by the umbilicovesical fascia, which extends from the umbilicus downward in a triangular fashion enveloping the bladder, umbilical artery, and urachus.[49] The potential space within the umbilicovesical fascia is called the perivesical space, which is not perceptible on imaging.[47,49] Anterior and lateral to the umbilicovesical fascia lies the prevesical space, which is much larger and clinically relevant. The prevesical space also runs posterior to the transversalis. It surrounds the lateral walls of the bladder.[17] The prevesical space is the largest potential space within the retroperitoneal pelvic compartment.[50] Between the pubis and the bladder, there is a space called the space of Retzius, which is contiguous with the prevesical space[48] [Figure 13].
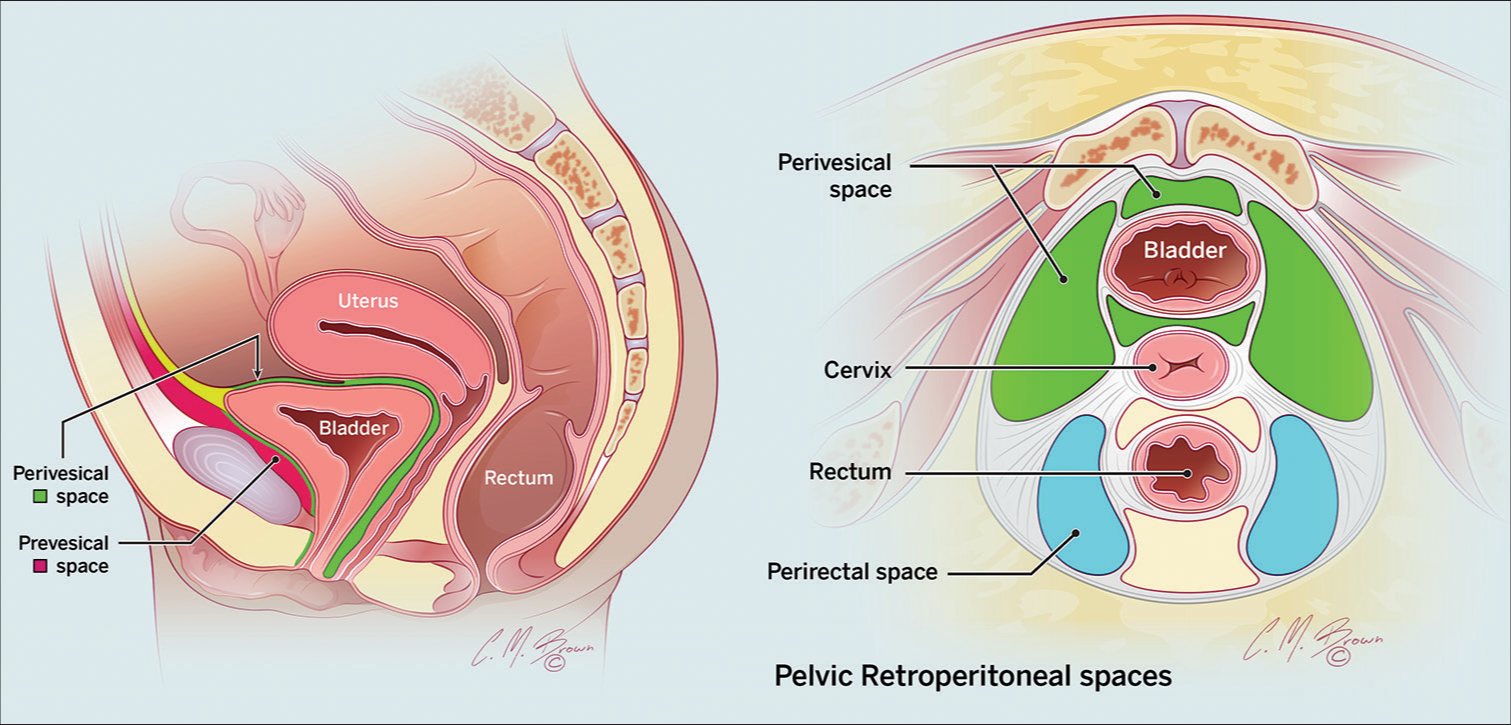
- Illustration of the pelvic retroperitoneal spaces on sagittal and axial views.
The posterior pelvic compartment is divided into perirectal and presacral spaces. The perirectal space is laterally bordered by the mesorectal fascia and posteriorly by the posterior pelvic fascia. Its anterior border comprises the rectovesical fascia in males and the rectovaginal space in females.[51] The presacral space is bordered anteriorly by the posterior rectal fascia, superiorly by the peritoneal reflection of the sigmoid colon, inferiorly by the rectosacral (Waldeyer’s) fascia, and posteriorly by the parietal fascia.[52] A potential space known as the pararectal space between the mesorectal fascia and parietal pelvic fascia exists.[47] The infrarenal space communicates inferiorly with the prevesical, perivesical, and presacral spaces. This extension of fluid occurs through medial extension or a route adjacent to the iliac vasculature [Figure 14].

- A 40 year old man with acute pancreatitis. Contiguous (a and b) sagital reformat and (c and d) axial abdominopelvic images demonstrating an inflammatory fluid collection in the infrarenal space (white arrow) with extension into the pelvis prevesical (star) and presacral (red arrows) spaces. Both medial (green arrow) and iliac vascular (blue arrow) modes of spread are seen.
Among the fluid collections, hemorrhage and bladder ruptures are the most commonly found in the prevesical space. Based on location of the bladder injury, the extravasation of urine may be intraperitoneal, extraperitoneal, or both. The importance of this distinction is that intraperitoneal injury is managed surgically, while extraperitoneal injury is managed conservatively. Injury to the dome of the bladder may lead to extravasation into the intraperitoneal space or space of Retzius resulting in extravasation into paracolic gutters, rectovesical, or rectouterine pouch and surrounding loops of bowel.[53,54] Extraperitoneal bladder ruptures are limited to the perivesical space and visualized in imaging as a “molar tooth” appearance. The “crown” of the “tooth” is anterior to the bladder, while its “root” extends posteriorly. The bladder may be displaced midline when large extraperitoneal pelvic fluid collections occur. The prevesical space is continuous with the rectus sheath, presacral space, and femoral sheath, which is clinically significant with retroperitoneal hematomas after femoral catheterization[22,48,55] [Figures 15-17].

- A 65 year old woman following right femoral catheterization. Contiguous abdominopelvic computed tomography (CT) axial images demonstrating a hematoma surrounding the femoral sheath 9 (red arrow). Hematoma is seen in the prevesical space (white arrow) with retrograde extension into the right infrarenal (star) and anterior and posterior pararenal spaces (green arrows).

- A 69 year old man with blunt abdominal trauma. Pelvic computed tomography (CT) (a) axial and (b) sagittal images demonstrating injury to the anterior bladder wall with contrast seen in the perivesical (red arrow) and prevesical (green arrow) spaces via direct communication.

- A 67 year old man with iatrogenic bladder injury during transurethral resection of the bladder tumor. Computed tomography (CT) cystogram (a) axial, (b) sagittal, and (c) coronal images demonstrating an injury to the anterosuperior bladder wall (white arrow). Contrast extravasation is seen with the perivesical (red arrow) and prevesical (green arrow) spaces. Contrast is seen with the large volume ascites (blue arrow) consistent with intraperitoneal urinoma.
Pelvic tumors are commonly encountered and can arise from gastrointestinal or genitourinary organs as primary lesions or metastatic disease.[56] Pelvic tumors may be intraperitoneal or extraperitoneal. Extraperitoneal tumors may arise from anterior, middle, and posterior compartments of the pelvis.[56] Colorectal cancer may reach to the pelvic space through lymphatic spread and vascular distribution of the colonic vessels.[33]
CONCLUSION
Understanding the intricacies of retroperitoneal anatomy and relevant pathological imaging manifestations is essential in the radiologist’s toolbelt. Describing the extent of abdominopelvic disease requires a thorough understanding of retroperitoneal anatomy, its compartments, and means of intercommunication. This knowledge allows radiologists to accurately characterize the extent of disease within the abdomen and pelvis. In addition, this anatomic insight aids in identifying possible pathologic sources and predicting disease spread, ultimately impacting patient management.
Acknowledgment
We thank Mauricio Hernandez, research manager, for reviewing the article and Christopher M. Brown, medical illustrator, for the illustrations.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Peritoneal and retroperitoneal anatomy and its relevance for cross-sectional imaging. Radiographics. 2012;32:437-51.
- [CrossRef] [PubMed] [Google Scholar]
- Radioanatomy of the retroperitoneal space. Diagn Interv Imaging. 2015;96:171-86.
- [CrossRef] [PubMed] [Google Scholar]
- Normal radiological anatomy of the retroperitoneum In: Radiological imaging of the kidney. Berlin, Heidelberg: Springer Berlin Heidelberg; 2014. p. :75-9.
- [CrossRef] [Google Scholar]
- Anatomy, abdomen and pelvis, retroperitoneum In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023.
- [Google Scholar]
- Anatomic communications between the three retroperitoneal spaces: Determination by CT-guided injections of contrast material in cadavers. AJR Am J Roentgenol. 1995;164:1173-8.
- [CrossRef] [PubMed] [Google Scholar]
- Basic clinical retroperitoneal anatomy for pelvic surgeons. Turk J Obstet Gynecol. 2018;15:259-69.
- [CrossRef] [PubMed] [Google Scholar]
- The great escape: Interfascial decompression planes of the retroperitoneum. AJR Am J Roentgenol. 2000;175:363-70.
- [CrossRef] [PubMed] [Google Scholar]
- Interfascial and perinephric pathways in the spread of retroperitoneal disease: Refined concepts based on CT observations. AJR Am J Roentgenol. 1997;168:639-43.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy of the retroperitoneum: Observations of the distribution of pathologic fluid collections. Radiology. 1996;200:95-103.
- [CrossRef] [PubMed] [Google Scholar]
- Embryology, anatomy, and surgical applications of the kidney and ureter. Surg Clin North Am. 2000;80:381-401, xiv
- [CrossRef] [PubMed] [Google Scholar]
- Why perirenal disease does not extend into the pelvis: The importance of closure of the cone of the renal fasciae. AJR Am J Roentgenol. 1995;164:1179-84.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomical communications of the perirenal space. Br J Radiol. 1998;71:450-6.
- [CrossRef] [PubMed] [Google Scholar]
- The perirenal space: Relationship of pathologic processes to normal retroperitoneal anatomy. Radiographics. 1996;16:841-54.
- [CrossRef] [PubMed] [Google Scholar]
- The perinephric space and renal fascia: Review of normal anatomy, pathology, and pathways of disease spread. Crit Rev Diagn Imaging. 1997;38:325-67.
- [Google Scholar]
- Radiology of perinephric fluid collections. Clin Radiol. 2002;57:339-46.
- [CrossRef] [PubMed] [Google Scholar]
- Perirenal spaces: CT evidence for communication across the midline. Radiology. 1987;164:657-64.
- [CrossRef] [PubMed] [Google Scholar]
- The anatomical compartments and their connections as demonstrated by ectopic air. Insights Imaging. 2013;4:759-72.
- [CrossRef] [PubMed] [Google Scholar]
- Medial border of the perirenal space: CT and anatomic correlation. Radiology. 1997;205:777-84.
- [CrossRef] [PubMed] [Google Scholar]
- Radiological diagnosis of perinephric pathology: Pictorial essay 2015. Insights Imaging. 2017;8:155-69.
- [CrossRef] [PubMed] [Google Scholar]
- Bridging septa of the perinephric space: Anatomic, pathologic, and diagnostic considerations. Radiology. 1986;158:361-5.
- [CrossRef] [PubMed] [Google Scholar]
- CT of the extraperitoneal space: Normal anatomy and fluid collections. AJR Am J Roentgenol. 1992;159:933-42.
- [CrossRef] [PubMed] [Google Scholar]
- Renal emergencies: A comprehensive pictorial review with MR imaging. Emerg Radiol. 2021;28:373-88.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous perirenal hemorrhage: What radiologists need to know. Emerg Radiol. 2011;18:329-34.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous perirenal hemorrhage in systemic lupus erythematosus: A rare case report and literature review. BMC Nephrol. 2021;22:217.
- [CrossRef] [PubMed] [Google Scholar]
- Urine leaks and urinomas: Diagnosis and imaging-guided intervention. Radiographics. 2003;23:1133-47.
- [CrossRef] [PubMed] [Google Scholar]
- Kidney in danger: CT findings of blunt and penetrating renal trauma. Radiographics. 2009;29:2033-53.
- [CrossRef] [PubMed] [Google Scholar]
- Nonoperative management of blunt renal trauma: Is routine early follow-up imaging necessary? BMC Urol. 2008;8:11.
- [CrossRef] [PubMed] [Google Scholar]
- Retroperitoneal tumours: Review of management. Ann R Coll Surg Engl. 2011;93:275-80.
- [CrossRef] [PubMed] [Google Scholar]
- Neoplastic and non-neoplastic proliferative disorders of the perirenal space: Cross-sectional imaging findings. Radiographics. 2008;28:1005-17.
- [CrossRef] [PubMed] [Google Scholar]
- Common primary tumours of the abdomen and pelvis and their patterns of tumour spread as seen on multi-detector computed tomography. Insights Imaging. 2011;2:205-14.
- [CrossRef] [PubMed] [Google Scholar]
- Perirenal extra-adrenal myelolipoma. World J Clin Cases. 2014;2:279-83.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding retroperitoneal anatomy for lateral approach spine surgery. Spine Surg Relat Res. 2017;1:107-20.
- [CrossRef] [PubMed] [Google Scholar]
- Renal fascial pathway: Posterior extension of pancreatic effusions within the anterior pararenal space. Radiology. 1986;158:367-74.
- [CrossRef] [PubMed] [Google Scholar]
- Retroperitoneal schwannomas in the anterior pararenal space: Dynamic enhanced multi-slice CT and MR findings. Abdom Imaging. 2013;38:201-10.
- [CrossRef] [PubMed] [Google Scholar]
- Radiologic features of extraperitoneal effusions. An anatomic approach. Radiology. 1972;104:249-57.
- [CrossRef] [PubMed] [Google Scholar]
- Giant posterior pararenal schwannoma: A case report and review of literature. Mol Clin Oncol. 2018;9:325-8.
- [CrossRef] [PubMed] [Google Scholar]
- Emergencies in the retroperitoneum: Assessment of spread of disease by helical CT. Eur J Radiol. 2004;50:74-83.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of the retroperitoneum. Radiol Clin North Am. 2012;50:333-55, vii
- [CrossRef] [PubMed] [Google Scholar]
- Comprehensive reviews of the interfascial plane of the retroperitoneum: Normal anatomy and pathologic entities. Emerg Radiol. 2010;17:3-11.
- [CrossRef] [PubMed] [Google Scholar]
- Retroperitoneal fasciitis: Spectrum of CT findings in the abdomen and pelvis. Radiographics. 2015;35:1095-107.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic retroperitoneal hematoma spreads through the interfascial planes. J Trauma. 2005;59:595-607.
- [Google Scholar]
- Grey Turner's sign and Cullen's sign in acute pancreatitis. Gastrointest Radiol. 1989;14:31-7.
- [CrossRef] [PubMed] [Google Scholar]
- The retroperitoneal interfascial planes: Current overview and future perspectives. Acute Med Surg. 2016;3:219-29.
- [CrossRef] [PubMed] [Google Scholar]
- Cross-sectional anatomy of the male pelvis. Abdom Radiol (NY). 2020;45:1951-60.
- [CrossRef] [PubMed] [Google Scholar]
- CT of pelvic extraperitoneal spaces: An anatomical study in cadavers. Clin Radiol. 2007;62:432-8.
- [CrossRef] [PubMed] [Google Scholar]
- Communications of the pelvic extraperitoneal spaces and their relation to the abdominal extraperitoneal spaces: Helical CT cadaver study with pelvic extraperitoneal injections. Radiology. 1997;202:523-30.
- [CrossRef] [PubMed] [Google Scholar]
- The prevesical space: Anatomical review and pathological conditions. Clin Radiol. 2013;68:733-40.
- [CrossRef] [PubMed] [Google Scholar]
- The subperitoneal space and peritoneal cavity: Basic concepts. Abdom Imaging. 2015;40:2710-22.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging of presacral masses-a multidisciplinary approach. Br J Radiol. 2016;89:20150698.
- [CrossRef] [PubMed] [Google Scholar]
- Bladder injury in blunt pelvic trauma. Radiology. 1986;158:633-8.
- [CrossRef] [PubMed] [Google Scholar]
- Resident and fellow education feature. Bladder injury: Types, mechanisms, and diagnostic imaging. Radiographics. 2014;34:802-3.
- [CrossRef] [PubMed] [Google Scholar]
- CT and anatomic study of postcatheterization hematomas. Radiographics. 1991;11:247-58.
- [CrossRef] [PubMed] [Google Scholar]
- MRI of tumors and tumor mimics in the female pelvis: Anatomic pelvic space-based approach. Radiographics. 2019;39:1205-29.
- [CrossRef] [PubMed] [Google Scholar]






