Translate this page into:
Renal Granulomatosis Post Intravesical Bacillus Calmette–Guerin Therapy for Non-muscle-invasive Bladder Cancer
Address for correspondence: Dr. Karen Tran-Harding, Department of Diagnostic Radiology, University of Kentucky Chandler Medical Center, 800 Rose Street, HX315E, Lexington, KY, USA. E-mail: karentran@uky.edu
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Intravesical Bacillus Calmette–Guerin (BCG) immunotherapy is a proven, effective treatment for intermediate- and high-risk non-muscle-invasive bladder cancer. Minor side effects are common and expected but systemic effects can occur in <5% of treated patients. We present a rare case of a 49-year-old male that presented with fever and chills after 3 weeks of intravesical BCG therapy post transurethral resection of bladder tumor. New renal lesions were present on contrast-enhanced computed tomography scan which was histologically proven to be necrotizing renal granulomatosis.
Keywords
Bacillus Calmette–Guerin
non-muscle-invasive bladder cancer
renal granulomas
urothelial carcinoma

INTRODUCTION
For over 40 years, intravesical BCG has been the gold standard treatment for intermediate- and high-risk non-muscle-invasive bladder cancer (NMIBC) after transurethral bladder resection.[1] BCG is an attenuated live strain of Mycobacterium bovis, and although its mechanism of action is not completely understood, it is believed that the treatment works through an immune response and a direct tumor response.[2]
Adjuvant BCG is highly effective in reducing the risk of recurrence of high-grade NMIBC by up to 70% compared with transurethral resection.[3] For carcinoma in situ (CIS), BCG has been shown to generate a complete response in up to 70%–90% of cases.[4] Minor toxic reactions such as urinary frequency, urgency, dysuria, and hematuria have been reported in 27%–90% of the patients.[5] Granulomatous complications are very uncommon and include entities such as prostatitis, epididymo-orchitis, cystitis, pyelonephritis, and abscesses.[5] The incidence of significant renal complications is significantly less and varies from 0.2% to 2% with renal granulomatosis occurring in 0.1% of treated patients.[5] We report a rare case of renal granulomas seen on imaging post intravesical BCG therapy for NMIBC.
CASE REPORT
Our patient is a 49-year-old male with a history of high-grade T1 urothelial cell carcinoma of the bladder who underwent induction Bacillus Calmette–Guerin (BCG) immunotherapy, and repeat biopsies of the bladder which were negative. Surveillance with a computed tomography (CT) urogram demonstrated a suspicious nodular focus along the right lateral wall of the bladder. Subsequent two office cystoscopies demonstrated no evidence of tumor recurrence or abnormalities. The patient, however, later underwent partial cystectomy 2 months later where the pathology was negative for malignancy. Repeat bladder biopsies 8 months after surgery revealed urothelial CIS. The patient elected to undergo a second induction course of BCG. After completing 4 of the 6 treatments, the patient developed low-grade fever/chills and low back pain and was seen in the emergency department. Contrast-enhanced CT (CECT) scan of the abdomen which was performed as part of the workup showed a roughly 2 cm mass-like area in the lower pole of the right kidney with moderate perinephric inflammatory changes [Figures 1a and b]. Smaller subcentimeter ill-defined hypodense foci were also seen. A primary renal mass was suspected, and a repeat CECT scan performed 3 weeks later demonstrated a persistent mass-like hypodense lesion in the right kidney with significantly improved perinephric inflammatory changes [Figures 2a and b]. The differential included infection or inflammation. Primary renal malignancies such as renal cell carcinoma and urothelial cell carcinoma and infiltrative masses such as lymphoma continued to be the main suspicions, and a CT-guided biopsy was recommended for histological confirmation [Figure 3a]. Histopathology confirmed marked chronic inflammation and necrotizing granulomas without evidence for malignancy [Figure 3b]. The primary clinical team decided to manage the patient conservatively with close follow-up due to resolution of the symptoms. Although antituberculous therapies are instituted in some cases, there continues to be a lack of consensus regarding appropriate management of renal granulomatosis. The patient then finished his fifth instillation of BCG. Eight months later, a CECT scan showed interval resolution of the right renal lesions with mild residual cortical scarring [Figures 4a and b]. On repeat cystoscopy and biopsy 8 months later, the patient was noted to have recurrent non-invasive high-grade papillary urothelial cell carcinoma. The patient has since had a radical cystectomy with ileal conduit urinary diversion.
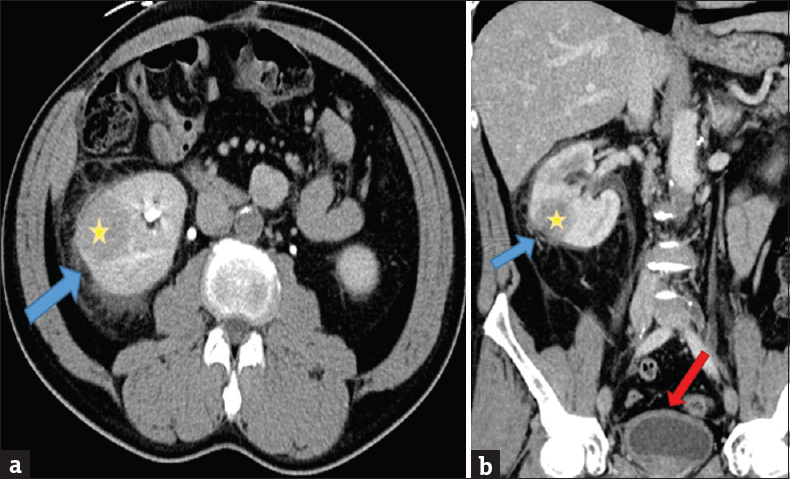
- A 49-year-old male with a history of high-grade T1 urothelial cell carcinoma of the bladder undergoing induction bacillus Calmette–Guerin immunotherapy. Initial presentation with fevers and chills after 3 weeks (4 of 6 treatments) of intravesical bacillus Calmette–Guerin therapy. (a) Axial contrast-enhanced computed tomography scan of the abdomen through the level of the kidney showing mass-like low attenuation lesion (yellow star) in the interpolar region of the right kidney with moderate surrounding perinephric inflammatory changes (blue arrow). (b) Coronal reformat contrast-enhanced computed tomography scan of the abdomen and pelvis showing mass-like low attenuation lesion (yellow star) in the interpolar region of the right kidney with moderate surrounding perinephric inflammatory changes (blue arrow). There is also mild diffuse bladder wall thickening (red arrow).
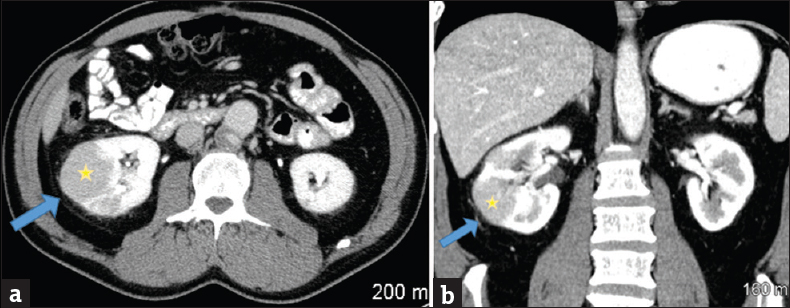
- A 49-year-old male with a history of high-grade T1 urothelial cell carcinoma of the bladder undergoing induction bacillus Calmette–Guerin immunotherapy. Initial presentation with fevers and chills after 3 weeks (4 of 6 treatments) of intravesical bacillus Calmette–Guerin therapy. (a) Axial contrast-enhanced computed tomography of the abdomen through the level of the kidneys shows low attenuation lesions (yellow star) in the interpolar region of the right kidney with improving perinephric inflammatory changes 3 weeks later (blue arrow). (b) Coronal reformat contrast-enhanced computed tomography scan through the abdomen showing low attenuation lesions (yellow star) in the interpolar region of the right kidney with improving perinephric inflammatory changes 3 weeks later (blue arrow).
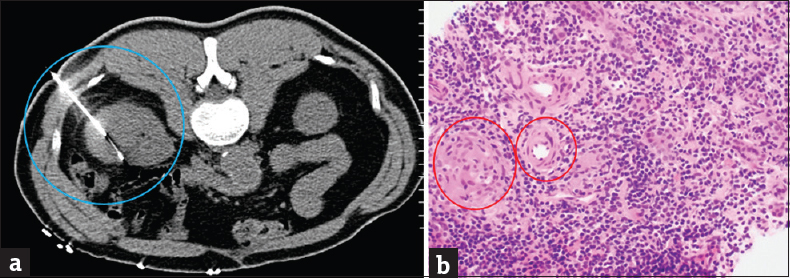
- A 49-year-old male with a history of high-grade T1 urothelial cell carcinoma of the bladder undergoing induction bacillus Calmette–Guerin immunotherapy. Initial presentation with fevers and chills after 3 weeks (4 of 6 treatments) of intravesical Bacillus Calmette–Guerin therapy. (a) Axial computed tomography of the abdomen through the level of the kidneys demonstrates a percutaneous computed tomography-guided biopsy of the lesion (blue circle). (b) Core needle biopsy from right renal mass showing marked chronic inflammation with granulomas (red circles). Special stains for acid-fast bacilli (Fite) and fungi (GMS) were negative (not shown).
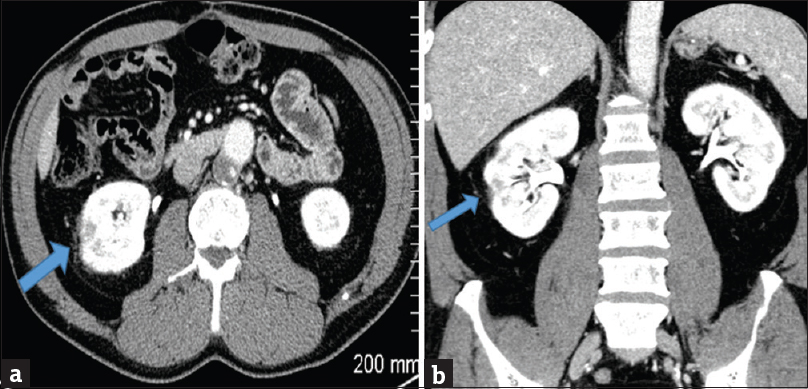
- A 49-year-old male with a history of high-grade T1 urothelial cell carcinoma of the bladder undergoing induction bacillus Calmette–Guerin immunotherapy. Initial presentation with fevers and chills after 3 weeks (4 of 6 treatments) of intravesical bacillus Calmette–Guerin therapy. (a) Axial contrast-enhanced computed tomography scan of the abdomen through the level of the kidneys showing interval resolution of the right renal lesions with mild residual cortical scarring 8 months later (blue arrow). (b) Coronal reformat contrast-enhanced computed tomography scan showing interval resolution of the right renal lesions with mild residual cortical scarring 8 months later (blue arrow).
DISCUSSION
Intravesical BCG has proven to be an effective treatment for intermediate- and high-risk NMIBC.[1] High-risk NMIBC is defined as any transitional cell carcinoma of the bladder with high-grade papillary stage Ta or T1 tumors and any patient with CIS.[1] BCG immunotherapy treatment is scheduled for patients that have had a complete transurethral resection of tumor and consists of once weekly interval treatment for a total of six treatments.[1]
The definition of BCG failure includes high-grade tumor recurrence.[1] Patients considered to be the highest risk are more likely to fail BCG treatment and are recommended an early cystectomy as in the case with our patient.[6] BCG is usually well tolerated with severe systemic complications only occurring in < 5% of patients.[7] It is debatable whether the complications result from a form of hypersensitivity reaction or an active mycobacterial infection.[7] Minor reactions are usually mild, transient, and easily managed. Flu-like symptoms occur in patients within the first 24–48 h following intravesical instillation and are usually explained by the inflammatory reaction triggered by the BCG.[7] Irritative lower urinary tract symptoms and gross hematuria are also common and usually occur after third instillation.[4] A single-dose of quinolone 6 h after instillation might decrease side effects and improve tolerability for minor reactions.[7] Other rare systemic complications include granulomatous reactions, pneumonitis and/or hepatitis, arthralgia, epididymitis, sepsis, rash, ureteral obstruction, contracted bladder, renal abscess, and cytopenia.[4] Severe complications can be prevented by careful patient selection and safe administration practices. Treatment of severe complications can require antituberculous medications for 3–6 months.[7]
The incidence of renal toxicity from BCG is anywhere from 0.2% to 2% with the development of a granulomatous renal mass occurring in < 0.1% of patients.[58] In some reports, renal disease presented as pyelonephritis after the third or fourth instillation doses. It can also present as flank pain or urinary frequency.[8] Other patients such as in our case present with features of renal mass.[8] It has been hypothesized that renal affliction by BCG therapy may be related to vesicoureteral reflux that commonly occurs after transurethral resection of bladder tumor.[9]
Imaging of post intravesical therapy, BCG granulomas can present as enhancing lesions on CECT scans.[5] Renal manifestations may include pyelonephritis or abscesses with a segmental distribution and perinephric stranding.[8] Some may even mimic expansile masses or present as multiple hypodense lesions with the kidney.[5] A “central unaffected calyx sign” has been described that shows BCG granulomatosis as a solid mass in the kidney with a normal calyx centrally.[10] The main differential considerations would, however, include primary renal neoplasms such as renal cell carcinoma or infiltrative conditions such as lymphoma or leukemia. Imaging can be quite inconclusive in the vast majority of the cases of renal granulomatosis such as in our case especially given the extremely low incidence of the condition. It would be prudent to obtain histological confirmation by image-guided percutaneous biopsy if there is no convincing improvement on subsequent follow-up imaging. Once confirmed, renal granulomas may be treated with rifampin and isoniazid for 3–6 months.[8] Sometimes, no treatment is undertaken and these granulomas tend resolve spontaneously as in our case.[8]
CONCLUSION
BCG is the gold standard therapy for NMIBC. Although it is usually well tolerated, a small number of patients can have systemic side effects. As renal granulomas though can present in a variety of different ways, it is essential to have high clinical suspicion to consider post BCG treatment reaction as a possible differential diagnosis. This case demonstrates the prudence of strict follow-up imaging so that prompt therapy can be initiated when necessary while the renal lesions are still asymptomatic. Although extremely rare, recognition of imaging findings of renal granulomas with an appropriate history is important to distinguish it from a primary renal or metastatic neoplastic process to avoid unnecessary surgical procedures and to preserve renal parenchyma.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/18/230280
REFERENCES
- Intravesical bacillus Calmette-Guérin instillation in non-muscle-invasive bladder cancer: A review. Int J Urol. 2018;25:18-24.
- [Google Scholar]
- Bacillus-Calmette-Guerin (BCG) organisms directly alter the growth of bladder-tumor cells. Int J Oncol. 1994;5:697-703.
- [Google Scholar]
- An individual patient data meta-analysis of the long-term outcome of randomised studies comparing intravesical mitomycin C versus bacillus Calmette-Guérin for non-muscle-invasive bladder cancer. Eur Urol. 2009;56:247-56.
- [Google Scholar]
- Maintenance bacillus Calmette-Guerin immunotherapy for recurrent TA, T1 and carcinoma in situ transitional cell carcinoma of the bladder: A Randomized Southwest Oncology Group Study. J Urol. 2000;163:1124-9.
- [Google Scholar]
- Asymptomatic renal BCG granulomatosis: An unusual complication of intravesical BCG therapy for carcinoma urinary bladder. Indian J Urol. 2015;31:259-61.
- [Google Scholar]
- EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: Update 2016. Eur Urol. 2017;71:447-61.
- [Google Scholar]
- Bacillus Calmette-Guérin (BCG) infection following intravesical BCG administration as adjunctive therapy for bladder cancer: Incidence, risk factors, and outcome in a single-institution series and review of the literature. Medicine (Baltimore). 2014;93:236-54.
- [Google Scholar]
- Imaging appearance of granulomatous disease after intravesical bacille Calmette-Guerin (BCG) treatment of bladder carcinoma. AJR Am J Roentgenol. 2009;192:1494-500.
- [Google Scholar]
- Vesicorenal reflux and intravesical chemotherapy. Prog Clin Biol Res. 1989;303:517-22.
- [Google Scholar]
- Granulomatous renal masses following intravesical bacillus Calmette Guérin therapy: The central unaffected calyx sign. Br J Radiol. 2007;80:e230-3.
- [Google Scholar]






