Translate this page into:
Post biopsy Liver Hemorrhage Successfully Controlled by Ultrasound-guided Percutaneous Microwave Ablation
Address for correspondence: Dr. Ophelia Ka Heng Wai, Department of Radiology and Organ Imaging, United Christian Hospital, 130 Hip Wo Street, Kwun Tong, Kowloon, Hong Kong, China. E-mail: ophelia.k.h.wai@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Percutaneous microwave coagulation therapy has been one of the major new developments in tumor ablation. Microwave ablation has also been used intraoperatively to achieve hemostasis at surgical margins in laparotomy. However, the use of microwave ablation for coagulation and hemostasis through percutaneous approach has not been described in the literature. Here, we report a case of hepatic amyloidosis with massive post biopsy liver hemorrhage, which could not be by transarterial embolization, and subsequently controlled by ultrasound-guided percutaneous microwave ablation. To the best of our knowledge, this is the first reported case of this technology application in human.
Keywords
Liver biopsy
liver hemorrhage
microwave ablation

[SHOW_RELATED_PUBMED_ARTICLES]

INTRODUCTION
Percutaneous liver biopsy is known to have risk of major complications, in particular, hemorrhage, due to the highly vascular liver tissue and limited access for hemostasis at biopsy site. Transarterial embolization and laparotomy are the mainstay of management in the current practice in case of massive post biopsy hemorrhage. However, they require special angiographic suite or operation theater which may not be easily accessible or readily available. We report a case of massive post biopsy hemorrhage, which could not be controlled by trans arterial embolization and patient could not undergo laprotomy. We performed this innovative application of ultrasound (US)-guided percutaneous microwave ablation to the post biopsy bleeding site to achieve hemostasis.
CASE REPORT
A 61-year-old man, smoker and social drinker with beta-thalassemia trait, who presented with painless jaundice for 1 month. On admission, his liver function was severely deranged (bilirubin: 532, alkaline phosphatase: 876, alanine transaminase: 98). Magnetic resonance imaging showed mild hepatosplenomegaly. Hepatitis serology, alpha-fetoprotein, and carcinoembryonic antigen tests were all negative. International normalized ratio (INR) and platelet count were normal, but prothrombin time (PT) and activated partial thromboplastin (APTT) were moderately raised. An urgent US-guided percutaneous liver biopsy was arranged. A 20-gauge Temno needle via coaxial system was used for liver biopsy. Three samples of tissue were obtained from the same site at segment 5 of the liver, followed by gelfoam injection along the track biopsy tract to reduce post biopsy hemorrhage. There was no hemorrhage observed immediately after the biopsy.
The patient went into shock after eight hours during the observation period after liver biopsy. Urgent contrast enhanced computed tomography (CT) revealed large intraperitoneal hemorrhage and contrast extravasation from biopsy site [Figure 1]. Urgent trans arterial embolization via femoral artery approach attempted but failed due to marked stenosis at origin of the celiac trunk [Figure 2]. Tortuous and stenosed hepatic arteries were also noted on angiogram [Figure 2]. Laparotomy was contraindicated due to high risk of mortality as the patient developed disseminated intravascular coagulopathy (DIC) with severely deranged clotting profile. After discussion between the intervention radiology team and surgical team, urgent US was arranged to localize the site of bleeding from biopsy tract on color Doppler study. Urgent US-guided percutaneous microwave ablation was performed after localization of active bleeding site by color Doppler US [Figure 3]. Under US guidance, microwave needle was inserted into the bleeding zone percutaneously through subcostal approach [Figure 4]. Coagulation was done with the Acculis MTA system, using 140 kW for 6 min, aiming at ~ 4.5 cm × 5.5 cm. Successful hemostasis was observed on both color Doppler US and contrast enhanced CT performed immediately after microwave ablation.
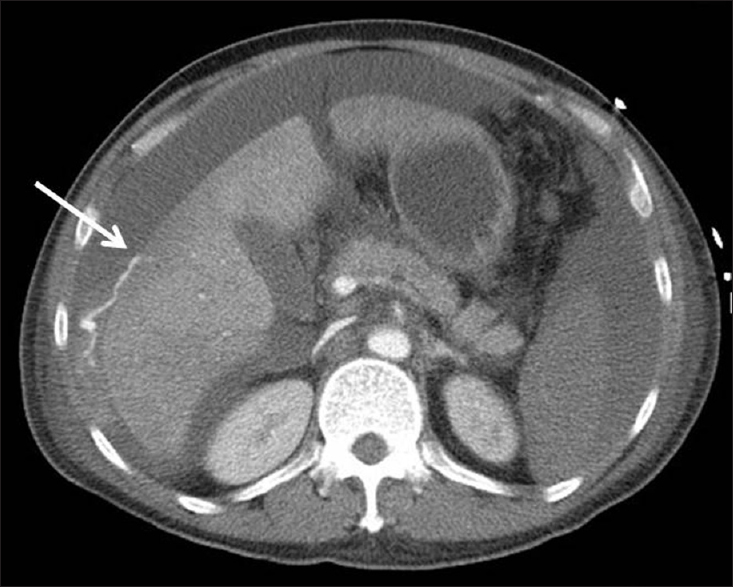
- A 61-year-old man with shock after liver biopsy. Contrast enhanced computed tomography of the abdomen demonstrates massive hemoperitoneum and active contrast extravasation from the anterior surface of segment 5 of the liver (arrow).
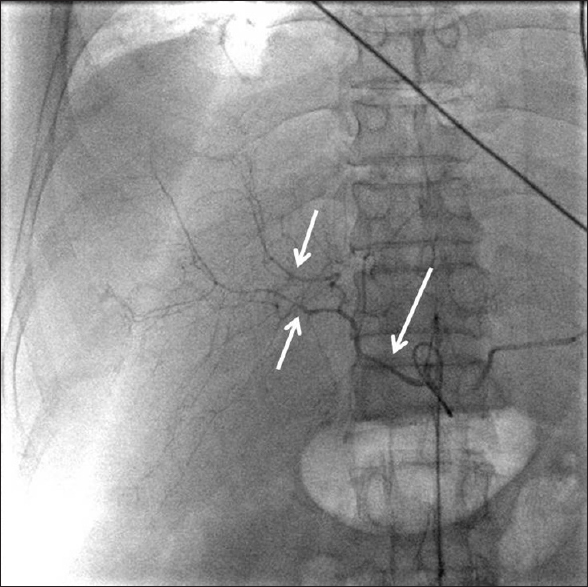
- Celiac angiogram of the patient showed marked stenosis and tortuous course of the celiac trunk, common and main hepatic arteries, and the intrahepatic arteries (arrows).
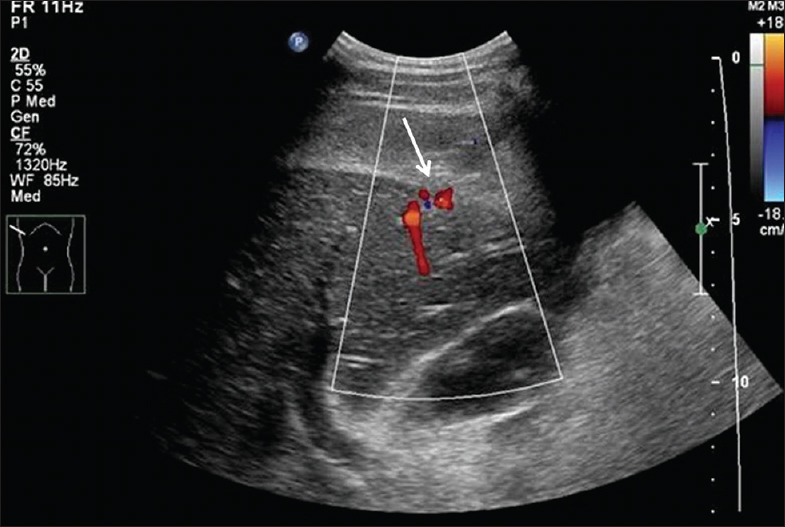
- Gray scale sagittal ultrasound image of liver with color flow Doppler demonstrates active bleeding from the segment 5 of liver corresponding to the biopsy site (arrow).
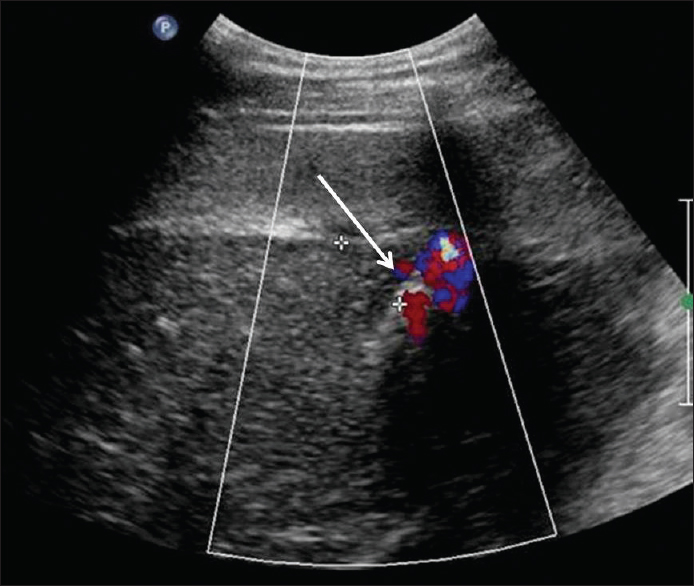
- Ultrasound-guided percutaneous microwave ablation performed with microwave needle targeted at the bleeding zone at segment 5 of the liver (arrow) demonstrates post ablation changes with cessation of bleeding.
The patient showed improved hemodynamics on the following day with stable hemoglobin level and improved clotting profile. Subsequently, liver biopsy report revealed hepatic amyloidosis, and the patient was wait listed for liver transplant. Unfortunately, patient's liver function showed continued rapid deterioration and had developed multiorgan failure after admission and unfortunately, succumbed due to cardiac arrest on day eleven after admission.
DISCUSSION
Liver biopsy is an important diagnostic procedure for investigation of liver disease and liver tumors. However, it is associated with known risks including major bleeding, bile leak, bowel and gallbladder perforation, and pneumothorax. It is estimated that the complication rate for major bleeding requiring blood transfusion or other procedures is about 1.0–1.7% and overall mortality rate is about 0.13–0.33%.[12] The risk of bleeding is higher in patients with impaired clotting profile and increases serum bilirubin.[1]
Currently, angiographic embolization and surgery remain the major treatments of choice for control of post biopsy liver bleeding. Microwave ablation has been initially developed to achieve hemostasis in laparotomy patients during hepatic resection and is a simple, rapid, and definite hemorrhage control method.[3] Percutaneous microwave coagulation therapy (PMCT) is now mainly used in tumor ablation therapy including liver, lung, renal, and bone malignancies.[4] No report regarding application of percutaneous microwave ablation for treatment of active bleeding in solid organs has been reported in the literature. An experimental study in 2008, using rabbit liver models with active bleeding produced by biopsy needle, showed that percutaneous microwave ablation could significantly decrease blood loss in animal models, and it is a simple and fast method to control blood loss in liver injuries with active bleeding.[5] Comparing microwave ablation and existing thermo ablative technologies including radiofrequency ablation, microwave has the advantage of achieving a consistently higher tissue temperature and covering larger tissue volume, thus theoretically allowing faster ablation time and larger area of coagulation.[4]
In this case, active contrast extravasation was demonstrated on CT and angiogram. However, angiographic embolization failed due to difficult vascular access and anatomy, with atherosclerosis and calcifications along the aortic wall, and irregular stenosis of the hepatic arteries. With DIC and unstable hemodynamic, the patient was not suitable for laprotomy. Thus, we attempted to do an US-guided percutaneous microwave ablation, which not been previously reported. The prerequisite for this procedure is that the site of bleeding has to be identifiable on US, which in this case could be demonstrated by color Doppler study showing a focus of active bleeding from the hepatic surface [Figure 2]. The highest power (140 W) and longest duration (6 min) recommended for liver ablation by the Acculis MTA system were applied to reach the largest tissue volume of ablation in the shortest period. After the first 6 minutes of ablation, no further active bleeding from the previous site of biopsy could be demonstrated on color Doppler US. Contrast enhanced CT done after percutaneous microwave ablation confirmed that homeostasis was achieved successfully.
Regarding the risk of bleeding, we suspect that the cause of massive post biopsy hemorrhage in our case could be related to underlying coagulopathy associated with amyloidosis. The patient had normal INR and platelet count, but the PT and APTT were abnormal. Coagulopathy is frequent in patients with amyloidosis due to factor X deficiency, decrease vitamin K-dependent clotting factors, and increase antithrombin activity fibrinolysis and DIC.[6] Amyloid can also deposit in vascular wall, resulting in weak and stenosed vessels; thus, angiographic embolization was difficult.
Percutaneous microwave ablation is a simple and fast procedure to achieve hemostasis. We believe that it has wide potential applications in solid organ hemostasis, especially in cases with contraindications for transarterial embolization, such as severe liver failure, portal vein thrombosis, and difficult vascular access or laparotomy (e.g., coagulopathy, unstable hemodynamic, risk of general anesthesia). Moreover, percutaneous microwave ablation may be performed at bedside without the need for going to the operation theater or patients not suitable to undergo angiographic suite; thus, it can be readily used when the previously mentioned setups are not available and in nonmajor hospitals or even in the emergency department. It may also play a role in other causes of solid organ hemorrhage, such as in trauma or ruptured vascular tumors including hepatocellular carcinoma and renal angiomyolipoma. However, there are several limitations regarding the use of PMCT for hemostasis. The bleeding site needs to be identifiable on US and reachable by percutaneous method. Moreover, the long-term efficacy and whether there will be delayed bleeding remain unknown. So far, this is the first reported case using PMCT for liver hemostasis; thus, our experience is very limited.
CONCLUSION
This is the first reported case of massive post biopsy liver hemorrhage successfully controlled by US-guided percutaneous microwave ablation.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
Acknowledgement
We would like to express our gratitude to our colleagues from the Department of Radiology and Organ Imaging, United Christian Hospital, who provided guidance and comments on the case management and manuscript preparation.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2016/6/1/34/190859
REFERENCES
- Indications, methods, and outcomes of percutaneous liver biopsy in England and Wales: An audit by the British Society of Gastroenterology and the Royal College of Physicians of London. Gut. 1995;36:437-41.
- [Google Scholar]
- Twenty-year audit of percutaneous liver biopsy in a major Australian teaching hospital. Intern Med J. 2006;36:692-9.
- [Google Scholar]
- Surgical treatment of liver injury with microwave tissue coagulation: An experimental study. J Trauma. 2004;56:984-89.
- [Google Scholar]
- Microwave ablation: Principles and applications. Radiographics. 2005;25(Suppl 1):S69-83.
- [Google Scholar]
- Hemostasis of active bleeding from the liver with percutaneous microwave coagulation therapy under contrast-enhanced ultrasonographic guidance: An experimental study. J Ultrasound Med. 2008;27:867-74.
- [Google Scholar]
- Acquired factor X deficiency in patients with amyloid light-chain amyloidosis: Incidence, bleeding manifestations, and response to high-dose chemotherapy. Blood. 2001;97:1885-7.
- [Google Scholar]





