Translate this page into:
Pixels to precision: Neuroradiology’s leap into 3D printing for personalized medicine

*Corresponding author: Thomas Stirrat, Department of Radiology, Georgetown University, Washington, United States. tps68@georgetown.edu
-
Received: ,
Accepted: ,
How to cite this article: Stirrat T, Martin R, Baek G, Thiru S, Lakhani D, Umair M, et al. Pixels to precision: Neuroradiology’s leap into 3D printing for personalized medicine. J Clin Imaging Sci. 2024;14:49. doi: 10.25259/JCIS_119_2024
Abstract
The realm of precision medicine, particularly its application within various sectors, shines notably in neuroradiology, where it leverages the advancements of three-dimensional (3D) printing technology. This synergy has significantly enhanced surgical planning, fostered the creation of tailor-made medical apparatus, bolstered medical pedagogy, and refined targeted therapeutic delivery. This review delves into the contemporary advancements and applications of 3D printing in neuroradiology, underscoring its pivotal role in refining surgical strategies, augmenting patient outcomes, and diminishing procedural risks. It further articulates the utility of 3D-printed anatomical models for enriched comprehension, simulation, and educational endeavors. In addition, it illuminates the horizon of bespoke medical devices and prosthetics, illustrating their utility in addressing specific cranial and spinal anomalies. This narrative extends to scrutinize how 3D printing underpins precision medicine by offering customized drug delivery mechanisms and therapies tailored to the patient’s unique medical blueprint. It navigates through the inherent challenges of 3D printing, including the financial implications, the need for procedural standardization, and the assurance of quality. Prospective trajectories and burgeoning avenues, such as material and technological innovations, the confluence with artificial intelligence, and the broadening scope of 3D printing in neurosurgical applications, are explored. Despite existing hurdles, the fusion of 3D printing with neuroradiology heralds a transformative era in precision medicine, poised to elevate patient care standards and pioneer novel surgical paradigms.
Keywords
Three-dimensional printing
Neuroradiology
Precision medicine
Surgical planning
Anatomical models
INTRODUCTION
Precision medicine, alternatively known as personalized medicine, is dedicated to tailoring treatment strategies to the unique genetic, environmental, and lifestyle intricacies of individual patients. This approach finds utility across diverse domains, from modeling prosthetics and educating stakeholders to replicating abnormal organs for better understanding.[1]
In radiology, three primary technologies are utilized for three-dimensional (3D) depiction: Volumetric rendering (VR), cinematic rendering (CR), and 3D printing. VR is widely available in most centers and creates 3D visualizations on screens, while CR represents a newer technology that offers life-like images [Figure 1]. However, unlike VR and CR, which are limited to screen-based visualization, 3D printing transforms these images into physical, tangible models. These models are particularly valuable in surgical planning and patient education, as they provide a more interactive understanding of complex anatomical structures.
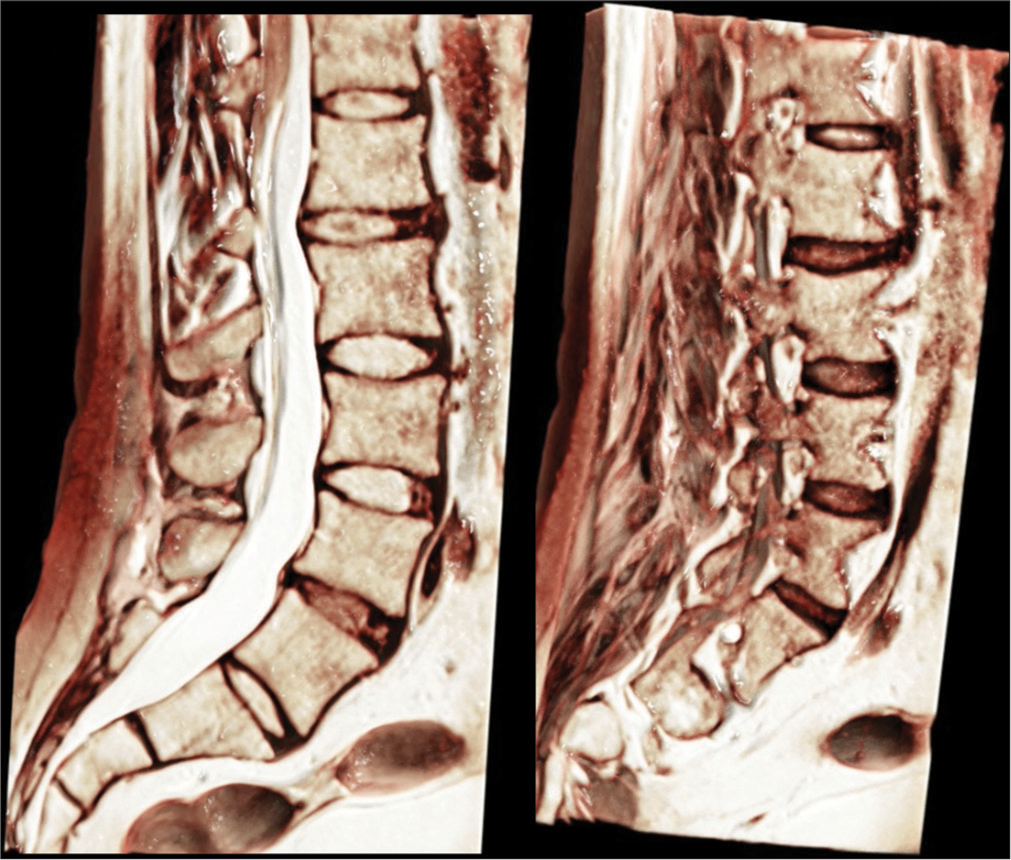
- Cinematic rendering of volumetric magnetic resonance data. These images illustrate the detailed anatomy of the lumbar spine, highlighting the vertebrae, intervertebral discs, and surrounding structures. The cinematic rendering algorithm enhances the visualization of bone and soft-tissue interfaces, providing a life-like representation ideal for surgical planning and educational purposes.
A notable frontier in this endeavor is the integration of 3D printing technology within the field of radiology, distinct from other 3D visualization methods such as VR and CR. While VR and CR provide visual depictions of anatomical structures on screens, 3D printing brings these images into the physical realm, creating patient-specific anatomical models that can be physically interacted with. This transition from digital to physical models in neuroradiology represents a significant advancement in precision medicine and surgical innovation, enabling more meticulous surgical planning and the development of customized medical devices [Figure 2].[2]

- Cinematic reconstruction of lower thoracic and lumbar spine volumetric computed tomography data. These images provide multiple perspectives of the lumbar spine, showcasing the complex anatomy and the relationship between the vertebral bodies, ribs, and spinal cord. The cinematic rendering technique allows for a more intuitive understanding of the three-dimensional spatial relationships, critical for both diagnostic and surgical applications.
Conventionally, neuroradiologists have depended on two-dimensional (2D) imaging modalities such as computed tomography (CT) and magnetic resonance imaging (MRI) for visualizing the brain and nervous system’s intricate structures. While these imaging techniques are invaluable, their portrayal of the brain’s complex 3D anatomy often falls short, posing challenges in the accurate diagnosis and management of intricate neurological disorders, especially those necessitating surgical interventions.[3]
For instance, in neuroradiology, a 3D printed model of a patient’s brain can be created from MRI or CT scans. This model allows surgeons to better visualize and plan the resection of complex tumors by offering a tangible representation of the brain’s intricate anatomy, which can be particularly difficult to fully comprehend through 2D images alone. This tangible model facilitates enhanced pre-operative planning, leading to better surgical outcomes and reduced intraoperative risks.[4]
MATERIAL AND METHODS
This paper offers a perspective on the integration of 3D printing in neuroradiology, drawing from a selective review of the literature. To inform this perspective, a targeted search of key databases, including PubMed, Google Scholar, and Scopus, was conducted using terms such as “3D printing,” “neuroradiology,” “radiology 3D printing,” and “3D printing in medicine.”
For this review, we selected studies relevant to the clinical applications, surgical planning, and educational impact of 3D printing in neuroradiology [Table 1]. Emphasizing methodological rigor and practical insights, we prioritized studies that addressed the challenges and future potential of these technologies. To ensure reliability and validity, we assessed study design quality, sample sizes, and alignment with established findings. We used the STROBE checklist for observational studies and the CASP tool for systematic and qualitative reviews, including only studies with robust methodologies to support our conclusions on advancements in neuroradiology.
| Reference | Key points | Application/impact |
|---|---|---|
| Delpierre and Lefèvre, 2023[1] | Defines and critiques the model of health promoted by precision medicine | Provides foundational understanding of precision medicine |
| Markovitz et al., 2021[2] | Role of 3D printing in neuroradiology education for medical trainees | Enhances medical education through practical models |
| Larsson and Wikström, 2017[3] | Overview of neuroradiology imaging techniques | Contextualizes the limitations of traditional imaging |
| Chen et al., 2020[4] | Advances in 3D printing technology for biomedical engineering | Highlights technological developments in 3D printing |
| Saenz et al., 2024[5] | Implementation of 3D modeling for improved understanding of AVM morphology, facilitating safer microsurgical excision. | Enhances spatial visualization and planning for complex pediatric AVM surgeries, potentially reducing surgical complications and improving outcomes. |
| Le Bras et al., 2023[6] | Simulation of endovascular embolization on patient-specific 3D-printed aneurysm models reduced procedure times | Improves procedural efficiency, minimizes radiation exposure, and enhances patient safety in neurovascular interventions. |
| Bartikian et al., 2019[7] | Customization of skull bone models using CT scans for 3D printing | Improves surgical planning and outcomes |
| Andronikou et al., 2018[8] | 3D printing of brain models for visual-aid in hypoxic ischemic injuries | Enhances communication and education in complex cases |
| Chacko et al., 2023[9] | Fidelity of 3D printed brains from MRI scans in children | Focuses on the accuracy and educational value of 3D models |
| Conti et al., 2016[10] | 3D printing of AVMs for radiosurgical treatment | Enhances precision in complex neurosurgical planning |
| Yang et al., 2024[11] | Systematic review on the use of 3D models in pediatric surgery | Emphasizes the educational and planning benefits in pediatrics |
| Parthasarathy et al., 2020[12] | 3D printing with MRI in pediatric applications | Demonstrates the utility in understanding complex craniofacial anatomy |
| Frölich et al., 2016[13] | Accuracy of 3D printed intracranial aneurysms using FDM | Assists in personalized treatment planning |
| Tack et al., 2016[14] | Review on 3D printing techniques in medical settings | Summarizes the benefits and challenges of 3D printing in surgery |
| Ulmeanu et al., 2023[15] | Use of bespoke cranial implants for surgery | Shows reduction in surgery time and improved outcomes |
| Mian et al., 2022[16] | Personalized cranial implant design using PEEK and 3D printing | Demonstrates advancements in implant design and customization |
| Lee and Kim, 2023[17] | Virtual surgical planning and 3D printing in orthognathic surgery | Increases accuracy and efficiency in complex surgeries |
| CHU de Brest, 2024[18] | Use of Stratasys J5 MediJet 3D printer for vascular surgery | Enhances surgical precision with multi-material models |
| Bücking et al., 2017[19] | Transitioning from medical imaging data to 3D printed models | Provides an overview of the workflow for creating anatomical models |
| Cappello and Potts, 2024[20] | Anatomy of the pterygopalatine fossa | Focuses on the educational use of 3D models in complex anatomy |
| Marciuc et al., 2021[21] | Use of 3D models in endovascular treatment of intracranial aneurysms | Improves understanding of aneurysm morphology and planning |
| Martínez-Galdámez et al., 2019[22] | Use of 3D-printed vascular models for optical coherence tomography | Enhances device testing and patient-specific planning |
| Ramirez et al., 2022[23] | 3D plastic modeling for cost-effective neuroanatomy teaching | Demonstrates accessibility and practicality of 3D printing in education |
| Souza et al., 2020[24] | 3D-printed endovascular simulator for training | Facilitates hands-on training in neuroradiology and vascular surgery |
| Bisighini et al., 2022[25] | Fabrication of transparent hollow cerebral vascular phantoms | Advances in vitroexperimentation and device testing |
| Yazgan et al., 2023[26] | AI in 3D printing and bioprinting | Explores the role of AI in enhancing 3D printing workflows |
| Chang et al., 2019[27] | 3D printing for procedure rehearsal and planning in interventional radiology | Aids in pre-operative simulation and improves surgical outcomes |
| Pinto-Coelho, 2023[28] | Innovations in medical imaging technology through AI | Surveys AI applications in enhancing 3D printing accuracy |
| Sidabutar et al., 2023[29] | Low-cost and open-source 3D printing in neurosurgery | Demonstrates feasibility of cost-effective 3D printing solutions |
| Sears and Morris, 2022[30] | Establishing point-of-care virtual planning and 3D printing programs | Discusses the logistics and benefits of on-site 3D printing |
| Ballard et al., 2018[31] | Clinical applications of 3D printing in radiology | Provides a primer on the integration of 3D printing in clinical practice |
| Haleem et al., 2021[32] | Overview of 3D printing applications in radiology | Summarizes the uses and benefits of 3D printing across radiology |
| Martín-Noguerol et al., 2022[33] | Management of 3D printing units in radiology departments | Advocates for centralized management to ensure consistency and quality |
| Cantré et al., 2020[34] | 3D imaging and printing for plastic preparation in interventions | Focuses on the precision and utility of 3D printing in surgical planning |
| Rogers-Vizena et al., 2017[35] | Cost-benefit analysis of 3D craniofacial models for surgery | Demonstrates cost savings and reduction in surgical times |
| Jovic et al., 2020[36] | Future of 3D bioprinting in surgery | Discusses the potential of bioprinting for creating bioengineered tissues |
| Meyer-Szary et al., 2022[37] | Role of 3D printing in complex medical procedures | Reviews the cross-specialty benefits of 3D printing for planning and training |
| Medellin-Castillo and Zaragoza-Siqueiros, 2019[38] | Design and manufacturing strategies for FDM in additive manufacturing | Addresses challenges and strategies in FDM printing for medical applications |
| Wüthrich et al., 2021[39] | Novel slicing strategy for printing overhangs without supports | Advances techniques for more efficient 3D printing processes |
| Parsons, 2022[40] | Harvard research advancements in 3D printing | Highlights innovations and future directions in 3D printing technology |
| 3D Solved, 2024[41] | Guide on resin 3D printing and support structures | Provides practical advice on using resin printers for medical applications |
3D: Three-dimensional, AVMs: Arteriovenous malformations, CT: Computed tomography, MRI: Magnetic resonance imaging, FDM: Fused deposition modeling, AI: Artificial intelligence
The focus is on synthesizing these key insights to present an informed viewpoint on how 3D printing is shaping the future of neuroradiology, highlighting both its current impacts and the challenges that must be addressed for broader clinical integration. This perspective is based on a comprehensive understanding of the available evidence, aiming to provide a balanced discussion of the benefits and limitations of 3D printing in neuroradiology.
RESULTS
Enhanced surgical visualization and precision planning
The application of 3D printing technology in producing bespoke models of the skull and brain has significantly advanced the treatment and surgical preparation for various conditions. Through the generation of a tangible replica of a patient’s skull, surgeons gain an unparalleled view of the intricate anatomy, enabling more precise surgical strategizing. This approach has been instrumental in elevating patient outcomes, minimizing the likelihood of surgical mishaps, and enhancing life quality. Implementation of 3D brain modeling in the microsurgical excision of complex pediatric arteriovenous malformations (AVM) has shown promising results. Specifically, studies demonstrate a reduction in complication rates when 3D modeling is used for pre-operative planning and intraoperative navigation, though the reduction was not statistically significant. This benefit is attributed to enhanced spatial understanding provided by the 3D model, which aids in the precision of pre-operative planning and navigation during surgery.[5]
Utilizing patient-specific 3D-printed brain models to rehearse endovascular embolization of complex intracranial aneurysms has demonstrated substantial benefits in both procedural efficiency and patient safety. By significantly reducing fluoroscopy time and overall procedure duration, this approach minimizes patient exposure to radiation while enhancing the precision and effectiveness of treatment. These advancements underscore the critical role of 3D modeling in pre-operative planning, leading to improved patient safety and setting a higher standard for quality in neurovascular care.[6] A notable investigation revealed the feasibility of customizing skull bone models for 3D printing by employing continuous axial volumetric acquisition via CT scans. This method underscores the potential for creating more intricate anatomical replicas, including those of vascular and nervous systems, offering a dissection-like experience.[7]
Moreover, 3D printing offers a bridge to demystify specific pathologies for non-radiologists and the general public. For instance, conveying the nuances of hypoxic ischemic brain damage in children through 2D imagery poses challenges. However, 3D printed models can vividly display the volumetric loss and ensuing pathology from hypoxic injuries in a child’s brain.[6] These models, created to a precise 1:1 scale based on MRI scans, preserve the fidelity of linear dimensions, crucial for medical education, consultations, legal evidence, and clinical discussions. The advancement in 3D printing fidelity promises to further bolster its application in surgical rehearsals, demonstrations, and planning.[8]
The comprehension of intricate neuroanatomy is greatly enhanced through the use of 3D printed models, assisting radiologists in deciphering complex brain or spinal structures [Figure 3]. This is particularly beneficial in diagnosing and planning treatment for challenging neurosurgical cases, such as tumors, aneurysms, and AVMs. AVM treatment, known for its complexity, benefits from precise volume contouring to ensure successful obliteration and minimize risks. A study leveraging 3D rotational angiography for AVM volume modeling demonstrated that contouring with the aid of a 3D printed model reduced the time required and increased spatial accuracy, with volumes closely matching those of the digital models. This precision and confidence in contouring underscore the value of these custom phantoms in treatment simulation and dosimetric analysis. By allowing clinicians to accurately replicate complex anatomical structures, these models provide a critical bridge between theoretical planning and actual surgical execution [Figure 4]. Furthermore, the enhanced visualization and interaction with 3D models facilitate a deeper understanding of spatial relationships, crucial for minimizing operative risks and optimizing patient outcomes.[9] Concurrent research supports the utility of 3D printed models in depicting functional and anatomical features of the pediatric brain, aiding in surgical planning and patient education, especially in cases of intractable epilepsy requiring surgical intervention.[10]

- Detailed cinematic rendering of the lumbar spine anatomy in multiple views, illustrating the vertebral alignment, intervertebral discs, and surrounding bony structures. These images highlight the intricate anatomy of the lumbar region from both lateral and posterior perspectives, enhancing spatial understanding critical for diagnostic evaluations and surgical planning.

- Cinematic reconstruction of cross-sectional views through the lumbar and sacral spine, providing a detailed representation of the muscular and soft-tissue structures surrounding the vertebrae. These images reveal the layered anatomy and spatial relationships within the lumbar region, facilitating an in-depth comprehension ideal for both educational and clinical applications in spinal surgery and pathology assessment.
The use of 3D printing also extends to head, neck, otolaryngology, and craniofacial surgeries, offering significant insights into complex anatomical relationships. Conditions like encephaloceles, potentially complicated by cleft palates, highlight the multidisciplinary utility of 3D models in understanding the spatial dynamics of lesions or abnormalities relative to critical structures.[11] In exploring vascular anomalies, another study showcased the precision of fused deposition modeling – a widely-used and cost-effective additive manufacturing method – in recreating cerebral aneurysms with high anatomical fidelity in most cases, enhancing the tools available for educational, clinical, and research purposes in personalized treatment planning, although necessitating post-processing for improved surface integrity.[12]
Refined surgical strategies and enhanced patient outcomes
A comprehensive review discovered that the integration of 3D printing in surgical processes notably reduced operation times in 42 out of 227 evaluated studies. This time efficiency was predominantly observed in the creation of surgical guides for maxillofacial interventions, preparatory models for spinal and maxillofacial surgeries, and the customization of implants in maxillofacial procedures, significantly benefiting from 3D technology. In particular, the fabrication of bespoke cranial implants led to an average operation time reduction between 15 and 69 min as reported in the review.[13]
Beyond facilitating meticulous surgical planning, 3D printing has been instrumental in decreasing surgical complications and enhancing patient recovery outcomes. The use of anatomically precise cranial models for pre-surgical implant molding has resulted in better implant fits, superior medical results, and reduced time in surgery and improved patient outcomes.[14,15] Research focusing on spinal and maxillofacial surgeries highlighted the benefits of using 3D models to lessen the exposure to ionizing radiation and shorten surgical times, thereby optimizing operational efficiency and patient care.[13]
Virtual surgical planning (VSP) and 3D printing have revolutionized orthognathic surgery, enhancing accuracy and efficiency. VSP enables precise pre-operative assessments and adjustments, crucial for surgeries demanding millimeter-level accuracy. This synergy not only shortens planning time but also increases outcome predictability, improving safety and efficiency in complex surgeries while reducing risks and aiding recovery.[16] The Stratasys J5 MediJet 3D printer at Brest University Hospital Centre has greatly enhanced surgical precision and efficiency, especially in vascular surgeries requiring high accuracy. Its ability to produce high-fidelity, multi-material models helps surgeons understand patient-specific anatomies, reducing surgical errors and improving safety. In addition, the use of ElasticoTM photopolymer for soft tissues replication is crucial for complex surgeries.[17]
DISCUSSION
Advancements in medical education and skill development
The adoption of 3D printing in neuroradiology significantly enriches hands-on learning experiences, deepening the understanding of neuroanatomy. By translating specific imaging data into 3D models, medical trainees can gain a more profound comprehension of imaging pathologies and their anatomical correlations.[18] Complex cranial regions like the pterygopalatine fossa are elucidated more effectively through this method.[19] Furthermore, detailed models of the middle ear, including the membranous and bony labyrinth along with ossicles, are made available for in-depth exploration by trainees.[20]
3D printed models have become invaluable tools for surgical simulation and education, particularly in the domain of neurovascular pathologies. These models provide a tangible reference for students, patients, and surgeons, illustrating the precise morphology of conditions such as aneurysms, including the dimensions of the neck and dome, as well as the branching vessels.[2] Comparisons between normal anatomical structures, like the circle of Willis, and their aneurysmal variants foster a richer understanding of spinal interventions including lumbar punctures, myelography, and facet injections. Demonstrating different approaches to the spinal canal, 3D models equipped with a fluid-filled channel mimic the feedback necessary for mastering lumbar puncture techniques affordably.[2]
3D printing extends its utility to the evaluation of vascular formations, aiding pre-surgical testing of catheters and stent placements in neurointerventional radiology. One study focused on printing models of the cervical internal carotid artery and carotid siphons, both standard and tortuous, to assess device performance and inform stent selection.[21] Another research project highlighted the advantage of 3D printed models in providing realistic anatomical replicas, superior to preserved cadaver specimens, for hands-on procedural training. These models facilitate the development of manual dexterity and the simulation of surgical techniques, offering a cost-effective and accessible learning tool. The study also explored the use of a 3D printing pen for creating models that can be easily integrated and removed from a cadaver base without damage, supporting a variety of educational needs. Such models are invaluable for patient consultations, showcasing custom pathologies like aneurysms or skull base tumors, and enhancing the anatomical understanding for both educators and learners. This approach proves beneficial across diverse resource settings, circumventing the limitations associated with cadaver-based training.[22]
The evolution of 3D printing technology further contributes to the enhancement of surgical proficiency and expertise. A particular study employed a 3D-printed endovascular technique simulator to train specialists in neuroradiology, neurosurgery, and vascular surgery. This simulator facilitates the mastery of endovascular maneuvers, potentially reducing patient trauma and improving surgical outcomes. Despite concerns regarding model durability and flexibility, this training tool represents a significant step forward in the replication of specific vascular lesions for tactile learning.[23] Additional research into the mechanical behavior of endovascular devices utilized 3D-printed, water-soluble molds covered in silicone, creating transparent, anatomically accurate models suitable for in vitro experimentation and device testing.[24]
Enhancements in 3D printing materials and technological innovations
The fusion of artificial intelligence (AI) with machine learning techniques is poised to revolutionize 3D printing in neuroradiology. AI systems can streamline the transformation of Digital Imaging and Communications in Medicine (DICOM) data into printable Standard Tessellation Language (STL) files, a process that currently requires manual intervention and can extend over several days.[25] By incorporating AI based solutions into CT and MRI scanners, images can be automatically postprocessed into finely segmented DICOM slices, facilitating their conversion into 3D printing-ready formats.[26] AI automatically distinguishes tissue densities in cranial CT scans, pinpointing areas such as tumors and blood vessels accurately. This segmented data are then used to create highly precise 3D models. Similarly, in spinal MRI scans, AI segments complex structures such as intervertebral discs and nerves, simplifying their conversion into 3D printable formats. These advancements expedite the transition from scan to model, cutting preparation time and bolstering the usefulness of 3D prints for surgical planning and education. Furthermore, AI can enhance print accuracy through real-time adaptive feedback mechanisms, identifying potential errors and adjusting print settings accordingly to ensure optimal outcomes.[27]
Advancements in 3D printing technology have also made entry-level printers increasingly accessible, challenging the notion that high-end printers and sophisticated segmentation software are prerequisites for neurosurgical planning. Research utilizing low-end 3D printers, in conjunction with open-source software like Cura Ultimaker, has demonstrated the feasibility of producing patient-specific models that accurately represent various neuroanatomical and axial skeletal variations, although with longer printing times.[28]
A comparative study on printer performance revealed distinct challenges associated with different printer models and software functionalities. While certain printers exhibited slower operation, they provided dependable results. In contrast, others achieved faster printing speeds but suffered from a higher failure rate. However, printers with open-source designs allow for extensive experimentation with printing parameters and materials. This highlights the evolving nature of 3D printing technology, with printers continuously improving in performance and accessibility.[29]
Point-of-care surgical planning and on-site 3D printing programs emerge as cost-effective solutions for producing bespoke anatomical models and surgical tools directly from patient imaging data. Yet, the pathway from imaging to patient-specific products is intricate, demanding utmost precision at every stage to ensure safety and efficacy. This end-to-end process requires robust safeguards, comprehensive quality control measures, and thoughtful consideration of logistics, including spatial, financial, and equipment needs, as well as specialized staff training. Personnel responsibilities span a wide range, covering areas from sterilization and billing to legal compliance in medical imaging acquisition and segmentation.[30]
Radiologists are uniquely positioned to lead the creation of 3D Medical Units, as advancements in imaging and related technologies continue to unfold.[31] By spearheading multidisciplinary collaborations with bioengineers, radiographers, and clinicians, radiologists can significantly extend the value of their expertise beyond traditional reporting. 3D printing offers a tangible extension of radiological analysis, providing critical, additional insights for referring physicians. With their specialized knowledge, radiologists are ideally suited to select the most appropriate imaging techniques for 3D printing based on specific clinical needs, whether it involves choosing the optimal CT acquisition phase, window level, or MRI sequence.[32]
Radiologists as pioneers in ensuring model accuracy
As guardians of imaging fidelity and consistency, radiologists are pivotal in minimizing discrepancies between imaging studies, radiological interpretations, and the resultant physical 3D models.[33] The precision of patient-specific anatomical replicas facilitates tangible interactions, offering surgeons a way to physically navigate through and understand complex spatial relationships, which is a clear advantage over traditional 3D imaging techniques. The necessity for further multicenter randomized control trials is highlighted to determine the precise value and potential reimbursement strategies for medical 3D printing.[34] Meanwhile, analyses in facial reconstruction through midfacial distraction have shown a significant decrease in operative times and complications in groups utilizing surgical models, translating to considerable cost savings estimated at $1036 for a 31.3 min reduction in surgery time.[35] Nonetheless, 3D printing enriches anatomical and physiological knowledge, reduces surgery duration, enhances patient recovery, and yields cost savings that outweigh the investment in the technology.[32] With continued innovation, the prospect for 3D printing within neuroradiology remains optimistic. Research is pushing the boundaries by exploring biodegradable materials and bioinks for the development of medical devices and implants designed to be absorbed by the body over time safely. Moreover, advancements in AI and machine learning are refining the process of converting medical imaging data into 3D models, enhancing accessibility and cost-effectiveness of the technology.[36]
Challenges and quality control in 3D printing
Despite its potential, 3D printing in neuroradiology faces several hurdles. The cost of 3D printing remains a significant barrier for some healthcare institutions. Moreover, there is an urgent need for establishing standardized protocols and guidelines to ensure the safe and effective application of 3D printing in clinical settings.[37]
A study examining the use of 3D reconstruction for planning and rehearsing interventional radiology procedures encountered technical obstacles in achieving a functional model. The goal was to replicate a patient-specific aorta with significant stenosis accurately. Enhancing print quality involves meticulous segmentation and selecting characteristics such as high contrast differentiation, use of IV contrast with CT scans, and reduced slice thickness for finer 3D reconstructions.[38] In addition, the use of extrusion printers presents challenges for models requiring internal support due to overhangs.[39,40] For instance, creating an aorta model necessitated the laborious manual removal of support structures, risking damage to the model’s exterior. Resin printers, although more expensive, can fabricate such models without needing supports.[41] Alternatively, dual-nozzle deposition printers can use one nozzle for the model and another for soluble support materials, simplifying postprocessing.[19] A related study detailed the extensive timeline from model design to completion, including segmentation, printing, support removal, and finishing processes.[24]
The selection of materials also plays a crucial role. Using transparent polylactic acid, for example, allows for better visualization of a vessel’s interior, aiding radiologists and surgeons in intervention planning and potential complication anticipation. This foresight can streamline surgical processes and optimize the use of angiography suites.[35]
Future perspectives in 3D printing and precision medicine
Delpierre and Lefèvre (2023) emphasize that precision medicine’s strength lies in tailoring interventions to individual patient needs, a concept exemplified by 3D printing’s ability to create bespoke anatomical models for personalized care. Markovitz et al. (2021) highlight the educational value of these models, noting their utility in enhancing spatial understanding for medical trainees and improving the practical application of imaging data. By integrating patient-specific models into both clinical practice and education, 3D printing not only advances precision medicine but also addresses gaps in training, offering a tangible approach to complex anatomy that traditional imaging cannot achieve. With ongoing advancements in materials and AI-driven workflows, 3D printing is poised to further refine surgical planning, enhance outcomes, and revolutionize medical education.
CONCLUSION
The introduction of 3D printing applications in neuroradiology heralds a new era in precision medicine, offering groundbreaking opportunities for surgical planning and the crafting of bespoke medical devices. By generating patient-specific models of the brain and nervous system, 3D printing enhances the precision and safety of surgeries, alongside fostering educational and training advancements. While challenges persist, ongoing research and technological developments promise to refine 3D printing applications further, ensuring continued improvement in patient care and opening new frontiers in precision medicine.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Precision and personalized medicine: What their current definition says and silences about the model of health they promote. Implication for the development of personalized health. Front Sociol. 2023;8:1112159.
- [CrossRef] [PubMed] [Google Scholar]
- Role of 3D printing and modeling to aid in neuroradiology education for medical trainees. Fed Pract. 2021;38:256-60.
- [CrossRef] [PubMed] [Google Scholar]
- Overview of neuroradiology. Handb Clin Neurol. 2017;145:579-99.
- [CrossRef] [PubMed] [Google Scholar]
- Freeform 3D printing of soft matters: Recent advances in technology for biomedical engineering. Biomed Eng Lett. 2020;10:453-79.
- [CrossRef] [PubMed] [Google Scholar]
- Implementation of 3D modelling to improve understanding and conceptualisation of arteriovenous malformation (AVM) morphology for the execution of safe microsurgical excision of complex paediatric AVMs. Childs Nerv Syst. 2024;40:2431-42.
- [CrossRef] [PubMed] [Google Scholar]
- Rehearsals using patient-specific 3D-printed aneurysm models for simulation of endovascular embolization of complex intracranial aneurysms: 3D SIM study. J Neuroradiol. 2023;50:86-92.
- [CrossRef] [PubMed] [Google Scholar]
- 3D printing anatomical models of head bones. Surg Radiol Anat. 2019;41:1205-9.
- [CrossRef] [PubMed] [Google Scholar]
- Technical report: 3D printing of the brain for use as a visual-aid tool to communicate MR imaging features of hypoxic ischaemic injury at term with non-physicians. Childs Nerv Syst. 2018;34:1573-7.
- [CrossRef] [PubMed] [Google Scholar]
- Fidelity of 3D printed brains from MRI scan in children with pathology (prior hypoxic ischemic injury) J Digit Imaging. 2023;36:17-28.
- [CrossRef] [PubMed] [Google Scholar]
- 3D-Printing of arteriovenous malformations for radiosurgical treatment: Pushing anatomy understanding to real boundaries. Cureus. 2016;8:e594.
- [CrossRef] [Google Scholar]
- The utility of three-dimensional modeling and printing in pediatric surgical patient and family education: A systematic review. 3D Print Med. 2024;10:1.
- [CrossRef] [PubMed] [Google Scholar]
- 3D printing with MRI in pediatric applications. J Magn Reson Imaging. 2020;51:1641-58.
- [CrossRef] [PubMed] [Google Scholar]
- 3D printing of intracranial aneurysms using fused deposition modeling offers highly accurate replications. AJNR Am J Neuroradiol. 2016;37:120-4.
- [CrossRef] [PubMed] [Google Scholar]
- 3D-printing techniques in a medical setting: A systematic literature review. Biomed Eng Online. 2016;15:115.
- [CrossRef] [PubMed] [Google Scholar]
- Bespoke implants for cranial reconstructions: Preoperative to postoperative surgery management system. Bioengineering (Basel). 2023;10:544.
- [CrossRef] [PubMed] [Google Scholar]
- Adaptive mechanism for designing a personalized cranial implant and its 3D printing using PEEK. Polymers (Basel). 2022;14:1266.
- [CrossRef] [PubMed] [Google Scholar]
- Redefining precision and efficiency in orthognathic surgery through virtual surgical planning and 3D printing: A narrative review. Maxillofac Plast Reconstr Surg. 2023;45:42.
- [CrossRef] [PubMed] [Google Scholar]
- CHU de Brest surgical planning with STRATASYS technology. Available from: https://www.stratasys.com/en/resources/case-studies/patient-specific-anatomicals-models [Last accessed on 2024 Apr 24]
- [Google Scholar]
- From medical imaging data to 3D printed anatomical models. PLoS One. 2017;12:e0178540.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomy, pterygopalatine fossa In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513269 [Last accessed on 2022 Sep 19]
- [Google Scholar]
- 3D Printed models-a useful tool in endovascular treatment of intracranial aneurysms. Brain Sci. 2021;11:598.
- [CrossRef] [PubMed] [Google Scholar]
- Optical coherence tomography: Translation from 3D-printed vascular models of the anterior cerebral circulation to the first human images of implanted surface modified flow diverters. Interv Neuroradiol. 2019;25:150-6.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional plastic modeling on bone frames for cost-effective neuroanatomy teaching. Cureus. 2022;14:e27472.
- [CrossRef] [Google Scholar]
- Endovascular technique simulator for Neuroradiology learning. Arq Neuropsiquiatr. 2020;78:535-40.
- [CrossRef] [PubMed] [Google Scholar]
- Fabrication of compliant and transparent hollow cerebral vascular phantoms for in vitro studies using 3D printing and spin-dip coating. Materials (Basel). 2022;16:166.
- [CrossRef] [PubMed] [Google Scholar]
- Artificial intelligence for 3D printing and bioprinting In: Orhan K, Jagtap R, eds. Artificial intelligence in dentistry. Cham: Springer; 2023.
- [CrossRef] [Google Scholar]
- Three-dimensional printing for procedure rehearsal/simulation/planning in interventional radiology. Tech Vasc Interv Radiol. 2019;22:14-20.
- [CrossRef] [PubMed] [Google Scholar]
- How artificial intelligence is shaping medical imaging technology: A survey of innovations and applications. Bioengineering (Basel). 2023;10:1435.
- [CrossRef] [PubMed] [Google Scholar]
- Low-cost and open-source three-dimensional (3D) printing in neurosurgery: A pilot experiment using direct drive modification to produce multi-material neuroanatomical models. Clin Neurol Neurosurg. 2023;228:107684.
- [CrossRef] [PubMed] [Google Scholar]
- Establishing a point-of-care virtual planning and 3D printing program. Semin Plast Surg. 2022;36:133-48.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical applications of 3D printing: Primer for radiologists. Acad Radiol. 2018;25:52-65.
- [CrossRef] [PubMed] [Google Scholar]
- 3D printing applications for radiology: An overview. Indian J Radiol Imaging. 2021;31:10-7.
- [Google Scholar]
- 3D printing units should be centrally managed in the radiology department. Eur J Radiol. 2022;148:110161.
- [CrossRef] [PubMed] [Google Scholar]
- Three-dimensional imaging and three-dimensional printing for plastic preparation of medical interventions. Radiologe. 2020;60(Suppl 1):70-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cost-benefit analysis of three-dimensional craniofacial models for midfacial distraction: A pilot study. Cleft Palate Craniofac J. 2017;54:612-7.
- [CrossRef] [PubMed] [Google Scholar]
- 3D bioprinting and the future of surgery. Front Surg. 2020;7:609836.
- [CrossRef] [PubMed] [Google Scholar]
- The role of 3D printing in planning complex medical procedures and training of medical professionals-cross-sectional multispecialty review. Int J Environ Res Public Health. 2022;19:3331.
- [CrossRef] [PubMed] [Google Scholar]
- Design and manufacturing strategies for fused deposition modelling in additive manufacturing: A review. Chin J Mech Eng. 2019;32:53.
- [CrossRef] [Google Scholar]
- A novel slicing strategy to print overhangs without support material. Appl Sci. 2021;11:8760.
- [CrossRef] [Google Scholar]
- Harvard researchers help 3D printing take its next step. 2022. Harvard Gazette. Available from: https://news.harvard.edu/gazette/story/2022/04/harvard-researchers-help-3d-printing-take-its-next-step [Last accessed on 2024 Sep 05]
- [Google Scholar]
- Do Resin 3D printers need supports? - 3D solved. Available from: https://3dsolved.com/do-resin-printers-need-supports [Last accessed on 2024 Apr 24]
- [Google Scholar]






