Translate this page into:
Pelvic Pheochromocytoma Mimicking as Urinary Bladder Pheochromocytoma: Looking Beyond the Obvious
Address for correspondence: Dr. Santosh Kumar, Department of Urology, Postgraduate Institute of Medical Education and Research, Chandigarh, Punjab and Haryana, India. E-mail: santoshsp1967jaimatadi@yahoo.co.in
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Pheochromocytomas located outside the adrenal glands are called paragangliomas. A pelvic location is rare, the most common location for a paraganglioma being the retroperitoneal space. Paragangliomas arise from neural crest cells. Pelvic pheochromocytomas may mimic urinary bladder pheochromocytomas on imaging studies. Patients may present with hypertensive crisis during micturition. We present a 26-year-old female who presented to us with accelerated hypertension with episodes of severe headache and palpitation during micturition. Based on imaging studies, she was diagnosed to have a urinary bladder pheochromocytoma. However, on exploration, the patient was found to have an extravesical pheochromocytoma arising from the left posterolateral pelvic wall, which was excised while preserving the bladder. We present this case report as pelvic pheochromocytomas can mimic bladder pheochromocytomas and are difficult to differentiate on radiological imaging and can lead to inadvertent cystectomy.
Keywords
Cystectomy
hypertension
pheochromocytoma
urinary bladder
INTRODUCTION

Pheochromocytomas are chromaffin cell tumors derived from the adrenal gland and sympathetic nervous system.[1] Extra-adrenal pheochromocytomas, also known as paragangliomas, account for 10–20% of all pheochromocytomas. More than 85% of these extra-adrenal lesions are found below the diaphragm, especially along the sympathetic chain or the organs of Zuckerkandl. Pelvic organ and urinary bladder involvement is rare.[2] The urinary bladder pheochromocytomas may present with paroxysmal hypertension induced by micturition and hematuria.
CASE REPORT
A 26-year-old female patient presented to our institute with a 3-month history of uncontrolled hypertension. She had accelerated hypertension, diabetes mellitus, and eclampsia during pregnancy, which were controlled after delivery with antihypertensive medication. The patient also complained of episodic attacks of headache and palpitation during micturition. No history of hematuria or lower urinary tract symptoms was present. The patient's pulse was 90 bpm and BP was 188/96 mm Hg. General physical examination was within normal limits. Routine biochemical and hematological work-up was normal. In view of uncontrolled hypertension in a young patient, further work-up revealed serum metanephrines to be elevated (660 pg/ml), normal range being 12–60 pg/ml. Contrast-enhanced computed tomography (CECT) abdomen revealed a large, lobulated, heterogeneously enhancing soft tissue mass measuring 6 × 4.5 × 5 cm in size, arising from the left posterolateral wall of the urinary bladder, with a few non-enhancing areas suggestive of necrosis [Figure 1]. The soft tissue had predominant endoluminal component projecting into the urinary bladder lumen. Bilateral adenexa were normal. Cystoscopy was done after optimizing the patient, which revealed a large bulge from the left postero-lateral wall of the urinary bladder with normal overlying mucosa, giving the impression of an intramural growth. Positron emission tomography (PET)/computed tomography (CT) using 68 Ga DOTANOC (111In-DOTA-1-Nal3-octreotide) showed intense tracer uptake (SUVmax 9.8) with somatostatin receptor expression in a large heterogeneously hyperenhancing soft tissue lesion 5 × 6 × 5 cm in size, seen arising from the left posterolateral wall of the urinary bladder [Figure 2]. With the diagnosis of bladder pheochromocytoma and in view of the large mass with involvement of trigone and bladder neck, the patient was prepared for radical cystectomy. After pre-operative optimization with alpha and beta blockers, the patient underwent exploratory laparotomy via an infraumbilical midline incision. During mobilization of the urinary bladder from its lateral attachments, there was an accidental rent in the anterior wall of the urinary bladder, which was extended intentionally for better exposure. The mass was seen arising from the left lateral pelvic wall closely abutting the urinary bladder [Figure 3]. The mass was dissected meticulously and completely excised [Figure 4]. Bladder was preserved and closed in two layers with absorbable sutures. Post-operative recovery was uneventful and patient remained normotensive without antihypertensive medications. Histopathological report of the specimen revealed a circumscribed tumor with cells arranged in an organoid pattern separated by thin fibrovascular septae. Tumor cells were monomorphic containing round to oval nuclei with finely dispersed chromatin, inconspicuous nucleoli, and abundant granular eosinophilic cytoplasm. Immunostain for synaptophysin, chromogranin, and CD56 were positive, consistent with paraganglioma [Figure 5].
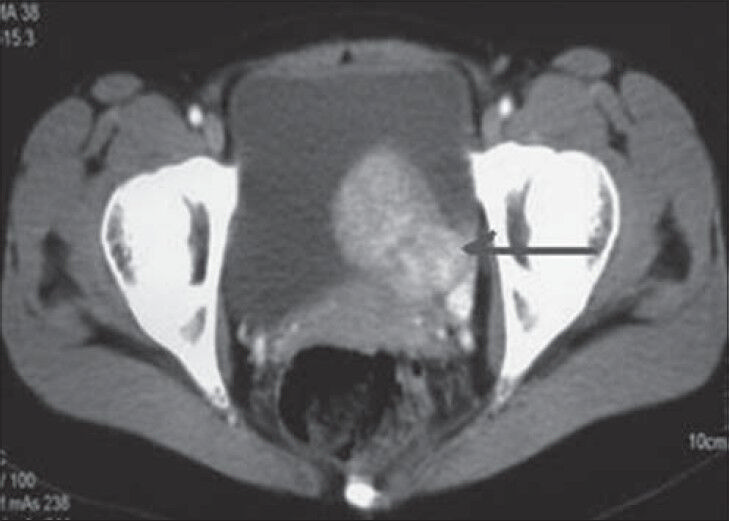
- 26-year-old female with accelerated hypertension and elevated serum metanephrines diagnosed with pelvic paraganglioma. CECT abdomen axial cut shows heterogeneously enhancing intraluminal growth (arrow) from the left anterolateral wall of the urinary bladder with predominant intraluminal component.
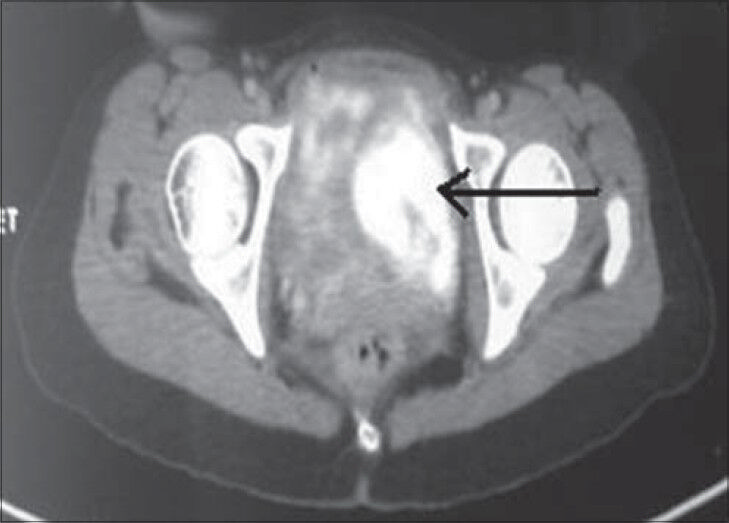
- 26-year-old female with accelerated hypertension and elevated serum metanephrines diagnosed with pelvic paraganglioma. PET/CT image shows intense tracer uptake and somatostatin receptor expressing lesion (arrow) in the left lateral wall of the urinary bladder.
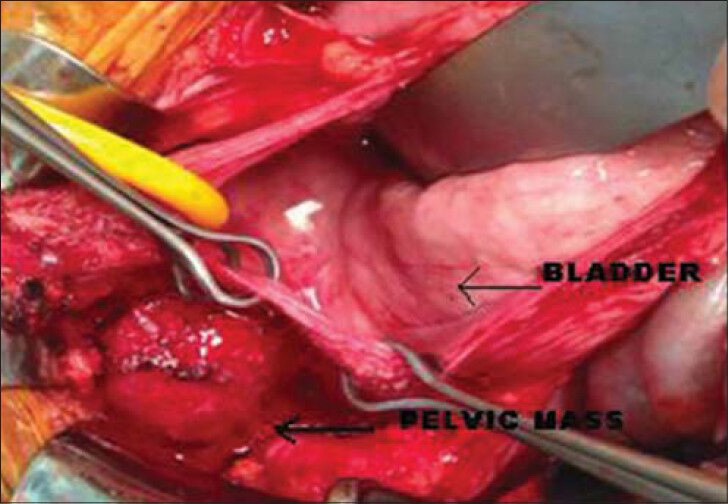
- 26-year-old female with accelerated hypertension and elevated serum metanephrines diagnosed with pelvic paraganglioma. Intraoperative image shows tumor arising from the left lateral pelvic wall (arrow) and the bladder appears normal (thin arrow).
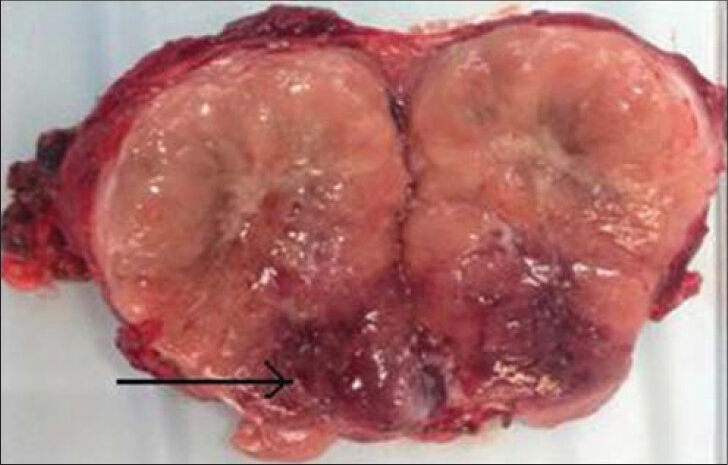
- 26-year-old female with accelerated hypertension and elevated serum metanephrines diagnosed with pelvic paraganglioma. Photograph of the cut specimen of the excised mass shows areas of necrosis in its inferior aspect (arrow).
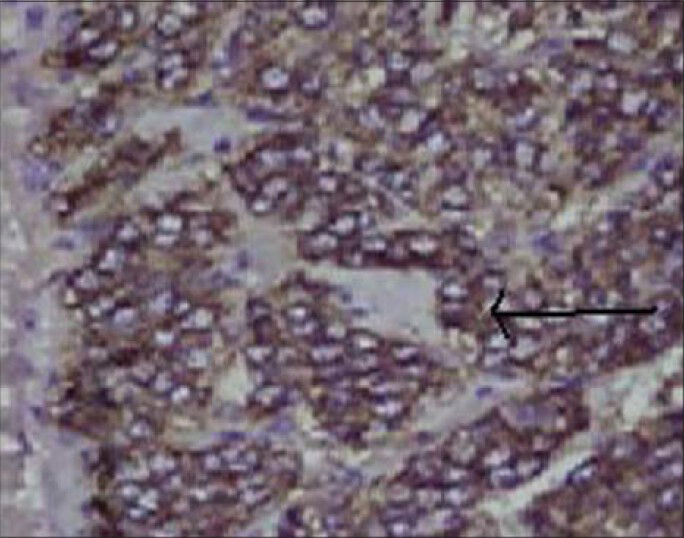
- 26-year-old female with accelerated hypertension and elevated serum metanephrines diagnosed with pelvic paraganglioma. Photomicrograph of the tissue on immunohistochemical staining (×10) shows positivity for chromogranin marker, suggestive of pheochromocytoma (arrow).
DISCUSSION
Paragangliomas are extra-adrenal pheochromocytomas.[1] These tumors are rare (10% of pheochromocytomas are paragangliomas), slow-growing, hypervascular lesions arising from the neural crest cells. Pelvic location is rare (2%)[2] and the most common location is the retroperitoneal space.[3] There is an increased incidence in women and in patients living at high altitudes. Paragangliomas occur mainly in adults[4] (mean age, 37 years; range, 11–70 years) and are usually benign. The signs and symptoms can be related to excess catecholamine secretion and include paroxysmal hypertension accompanied by anxiety, sweating, a throbbing headache, and either facial pallor or flushing during an attack.[1] On the other hand, bladder pheochromocytoma is also a rare tumor, accounting for less than 1% of all pheochromocytomas.[5]
The hypertensive crises result from excessive catecholamine secretion usually accompanying voiding.[6] Our index case was diagnosed to have accelerated hypertension and eclampsia, which were under control after delivery on antihypertensive medications. However, she presented with complaints of uncontrolled hypertension after about 1 year of delivery, with episodes of headache and palpitation on micturition. Catecholamine and vanillylmandelic acid levels in the urine or catecholamine levels in the plasma help in the diagnosis of a symptomatic pheochromocytoma. In our case, patient's urinary and metanephrine levels were not markedly raised on evaluation for uncontrolled hypertension. Imaging is essential in evaluating the location, extent, and mutifocality of the disease. CT can detect larger tumors, but its sensitivity is just 82%. In our index case, CT revealed a large, lobulated, heterogeneously enhancing soft tissue mass arising from the left posteroinferior wall of the urinary bladder, with areas of necrosis. With the suspicion of urinary bladder pheochromocytoma, the patient underwent cystoscopy, which showed normal bladder mucosa with a bulge in the left anterolateral wall near the bladder neck with a non-visualized left ureteric orifice suggesting submucosal growth from the urinary bladder wall. The treatment of pelvic pheochromocytoma is primarily surgical, and patient preparation is an essential step, which includes pre-operative treatment with alpha and beta blocking agents. Surgical resection is the treatment of choice.[7]
The patient was planned for radical cystectomy in view of the large endophytic bladder growth and taken for surgery after optimization of her blood pressure with alpha and beta blockers. Intra-operatively, we found an exophytic growth arising from the left lateral pelvic wall abutting the bladder in the lateral wall. The bladder wall adjacent to the mass was normal. The mass was dissected from the adjacent tissues and excised preserving the bladder. Post-operatively, the patient recovered well and has normal blood pressure, not requiring any antihypertensive medication.
CONCLUSION
Pelvic pheochromocytomas are a common location of paragangliomas and may mimic urinary bladder pheochromocytomas on imaging studies due to their location and restricted space in the pelvic region. Detailed imaging investigations along with pre-operative evaluation and preparation are important prior to planning intervention to prevent inadvertent cystectomy.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/56/143409
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Best cases from the AFIP: Paraganglioma of the organs of Zuckerkandl. Radiographics. 2003;23:1279-86.
- [Google Scholar]
- Laparoscopic resection of a large periadrenal nonmalignant pheochromocytoma. Surg Endosc. 2002;16:362-3.
- [Google Scholar]
- Clinical presentation and penetrance of pheochromocytoma/paraganglioma syndromes. J Clin Endocrinol Metab. 2006;91:827-36.
- [Google Scholar]
- Extraadrenal retroperitoneal paraganlioma: Clinical, pathologic, and CT findings. AJR Am J Roentgenol. 1990;155:1247-50.
- [Google Scholar]
- Pheochromocytoma of urinary bladder: Contemporary methods of diagnosis and treatment options. Urology. 1993;41:435-9.
- [Google Scholar]
- Bladder pheochromocytoma: A 3-year follow-up after transurethral resection (TURB) Urol Int. 2000;65:176-8.
- [Google Scholar]






