Translate this page into:
Patients Radiation Risks from Computed Tomography Lymphography

*Corresponding author: Abdullah Almujally, Departments of Radiology, Fondazione IRCCS Policlinico S. Matteo, School University of Pavia, Pavia, Italy. abdullah.almujally@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Almujally A, Sulieman A, Calliada F. Patients radiation risks from computed tomography lymphography. J Clin Imaging Sci 2020;10:46.
Abstract
Objectives:
This study aims to first measure patient doses during computed tomography (CT) chest, abdomen, and extremities procedures for evaluation lymphedema, and second to estimate the radiation dose-related risks during the procedures.
Material and Methods:
Radiation effective doses from CT lymphography procedures quantified using CT machines from different vendors. After the calibration of CT systems, the data collected for a total of 28 CT lymphography procedures. Effective and organ doses extrapolated using national radiological protection software based on Monte Carlo simulation.
Results:
The mean patient doses for chest and abdomen procedures in term of CTDIvol (mGy) and DLP (mGy.cm) are 10.0 ± 3 and 425 ± 222 and 24 ± 12 and 1118 ± 812 for CT 128 and CT 16 slice, respectively. The mean DLP (mGy.cm) for extremities was 320 ± 140 and 424 ± 212 for CT 128 and CT 16 slice, in that order.
Conclusion:
Patients’ dose showed significant differences due to variation in the scan length and clinical indication. Organs lay in the primary beam received high radiation doses especially in the chest region which increases the probability of radiation-induced cancer. The current patient’s doses are higher compared to the previous studies.
Keywords
Lymphography
Computed tomography dosimetry
Radiation risk
Cancer incidence
INTRODUCTION
The usage of computed tomography (CT) for medical diagnostic imaging is increasing for differential diagnosis of lymphedema. Patients were exposed to a significant-high radiation dose range between 2.5 up and 30 mSv from CT procedures.[1] Rehani et al. recently reported that more than 2.5 million patients received an effective dose above 100 mSv due to repetitive radiation exposure.[2] The incidence of lymphedema is increasing due to an increase in cancer incidence and the survival rate due to advancements in cancer treatment. Radiation-induced cancer due to CT imaging contributes up to 2.0% of current cancer incidence in the United States.[3] The benefit of justified using as low as reasonable achievable radiation doses exceed the projected radiogenic risk. However, still patients exposed to less optimized CT procedures.[4] Recent study by Mettler et al. in the US showed that the efforts of dose reduction and optimization produced in a reduction of patient doses from CT procedures by 6%.[4] This reduction is due to the increasing awareness of staff at radiology departments and improved CT design and improvement in detector technology by producing sensitive detectors and that allows generating high image quality with a least radiation dose.[4] The modern multidetector technology (sensitive detectors) enabled efficient usage of radiation dose to obtain diagnostic findings.[2,5] Patients are frequently exposed to radiation. Therefore, there is a need for evaluation of radiation risk from CT procedures to explore a method for radiation dose optimization. Lymphedema is a common lymphatic system disorder affect more than 250 million individual worldwide.[6] CT procedure is frequently performed for lymph node evaluation. This study aims to measure patient doses during CT chest, abdomen and extremities procedures, and second to evaluate the radiation dose-related risks during the procedures.
MATERIAL AND METHODS
CT machine and patient population
The effective dose for 28 patients had undergone CT examinations for lymphedema as clinical indications. All procedures were performed a tertiary hospital equipped with two CT modalities CT 128, 16 detectors from Siemens (Siemens Healthcare, Germany). The two CT machines were calibrated to assure the accuracy of dose measurements. An accuracy of measured dose up to ±5% was obtained. The patient doses were estimated using measurements of CT dose indexes (CTDI), exposure-related parameters, and the ImPACT spreadsheet based on NRPB conversion factors.[1,7,8] Data were collected using a sheet for all patients to maintain the consistency of the information displayed during CT examinations. All CT machines are equipped with a CT dosimetry unit. A data collection sheet was designed to evaluate the patient doses and the radiation-related factor. The collected data include, sex, age, tube potential, tube current-time product settings, pitch, slice thickness, and total slice number, Moreover, all scanning parameters were recorded, as well as the CT dose index volume (in millisievert) and dose-length product (in millisievert-centimeters).
CT dose measurements
Patients radiation doses reported using two dose indicators volume CTDIvol (mGy) and dose-scan length product (DLP [mGy.cm]). Tissue and organ equivalent dose conversion coefficient was obtained from the national protection board (NRPB) now health protection agency datasets in the UK based on the Monte Carlo simulations.[7] The CTDOSE dose analysis and estimation software developed by the ImPACT scan group was used to extrapolate the effective and organ doses.[7,8] CT scan acquisition and exposure factors such as peak tube potential (kVp), tube current (mA), exposure time (second), pitch, slice thickness (mm), gender, and scan acquisition parameters were used to calculate the dose values.
CT lymphographic technique
CT lymphographic imaging was carried out for 128 patients using two CT modalities (128 and 16 Detectors. The ethics and research committee approved this retrospective study. Before image acquisition, patients were positioned in the supine with head first position. For the two modalities, constant tube potential fixed at 120 kVp, different tube current and scan length were used for all patients [Table 1]. The technique consists of contrast and non-contrast CT image acquisition. Contrast medium injected at the area of the interest after local anesthesia. Image acquisition is usually performed at a certain time interval up to 10 min after the administration of the contrast media [Table 1].
| CT detector | Age (year) | Exposure setting (mAs) | Scan length (cm) |
|---|---|---|---|
| CT 128 | 36.0±10.0 (18.0–75.0) | 190±60 (100.0–280.0) |
53±17 (38.0–77.0) |
| CT 16 | 40.0±7 (30.0-64) | 340±30 (210.0-455.0) |
47.0±5 (42.0.0-55.0) |
RESULTS
Patient’s doses during CT procedure, including chest and lower or upper extremities, are illustrated in Tables 1-3. The mean patient doses in term of CTDIvol (mGy) and DLP (mGy.cm) are 10.0 ± 3 and 425 ± 222 and 24 ± 12 and 1118 ± 812 for CT 128 and CT 16 slice, respectively. The results show that the patient dose from CT 16 slice is double the dose from 128 slices. A considerable variation in patients doses up to 100% between the two imaging modalities in terms of radiation dose per slice CTDIvol (mGy), dose per procedure (DLP [mGy.cm]) and effective dose (mSv). This can be attributed to variation exposure parameters selection and imaging protocol.
| CT modality | CTDIvol(mGy) | DLP (mGy.cm) |
Effective dose(mSv) |
|---|---|---|---|
| CT 128 | 10.0±3 (5.0–14.0) | 475±220 (166.0–950.0) | 6.6±3 (2.3–13.3) |
| CT 16 | 24.0±12 (13.0–36.0) | 1118±812 (545–1695.0) | 15.7±12 (7.6–23.7) |
| CT modality | CTDIvol(mGy) | DLP (mGy.cm) |
Effective dose (mSv) |
|---|---|---|---|
| CT 128 | 4.5±2 (3.5.0–6.0) | 320±140 (120.0–460.0) | 1.0±0.4 (0.4–1.4) |
| CT 16 | 8.0±4 (6.0–12.0) | 424±212 (220–618.0) | 1.3±0.6 (0.7–1.9) |
DISCUSSION
The patient effective dose also showed that the same level of variation since the patient group is within the same age range considerable variation of mean organ doses among hospitals were observed for similar CT examinations. In addition to that, patient’s doses showed 3 time variations between the minimum and maximum values suggesting that imaging protocol should be standardized and optimized. The mean scan length always and tube current-time product (mAs) are in direct proportional relation with patient doses. Thus, precise adjustment of these factors will result in a drastic reduction of patient dose without deterioration of the image findings quality. The mean effective dose (mSv) per procedure is 6.6 ± 3 and 15.7 ± 12 for CT 128 and CT 16 slices, in that order. The effective dose for CT lower extremities is lower compared to CT abdomen and pelvis [Table 3]. This can be attributed to the fact that most of human radiosensitive organs and tissues located in the trunk region. The lower DLP to effective dose conversion factor was used compared to CT chest and abdomen. The prospect of radiogenic risk due to ionizing radiation exposure depends on irradiated organ doses, age at exposure, and patient tissue or organ weighting. The patient radiogenic risk per CT examination is ranged from 35 to 70 × 10-5 per procedure. The current practice showed that patients usually exposed to a high dose exceeding 100 mSv in a year due to their diagnosis and treatment follow-up. Lymphedema patients undergo a series of imaging procedures, including nuclear medicine procedures such as single-photon emission CT (SPECT) or positron emission tomography with sensitivity up to 96%.[9] In literature, to the best of our knowledge, this is the first study provided radiation dose for lymphedema patients undergoing CT procedures. Various organs in the primary beam received a high radiation dose. Breast, lung, and heart received an equivalent dose (mSv) 30, 32, and 35 mSv per single procedure, respectively. This high organ doses increase the risk of radiation-induced cancer for these specific organs, especially for young patients. All previous studies reported the dose value for specific organs (chest, abdomen, brain, or extremities) for different clinical indications. Thus, this study provided new information regarding the radiation risk for lymphedema patients. In comparison with previous studies, comparable patient dose (DLP, mGy.cm) for 128 CT slice while the patient dose from 16 CT slice is higher from all published studies [Figure 1].[10-12] The current study dose is higher compared to conventional CT procedures because, in this study, additional image acquisition is required to provide further details according to the clinical indication.[13,14] However, still, dose can be optimized to assure that patients received a minimum radiation dose.
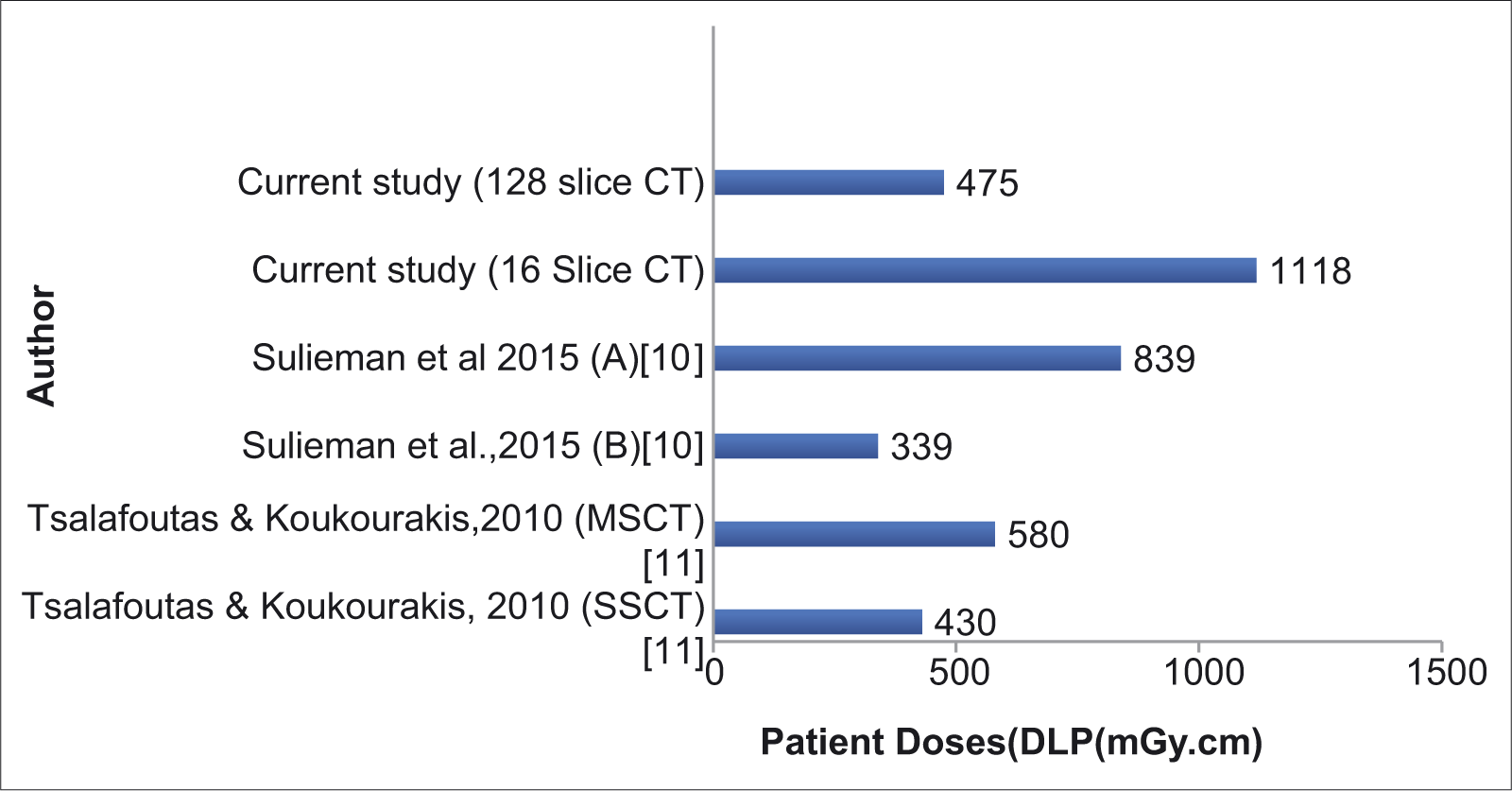
- Comparison of patient dose during chest computed tomography (CT) procedure. MSCT: Multislice CT, SSCT: Single slice CT, A: control group, B: optimization group).
CONCLUSION
Patient radiation dose during CT lymphographic imaging procedure was evaluated. Patients’ dose showed significant differences due to variation in the scan length and clinical indication. Organs lay in the primary beam received high radiation dose, especially in the chest region, which increases the probability of radiation-induced cancer. The current patient’s dose is higher compared to the previous studies. Optimization of radiation dose is recommended to ensure that patients received the minimum possible dose without affecting the quality of the images.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The 2007 recommendations of the international commission on radiological protection. ICRP publication 103. Ann ICRP. 2007;37:1-332.
- [Google Scholar]
- Patients undergoing recurrent CT scans: Assessing the magnitude. Eur Radiol. 2020;30:1828-36.
- [CrossRef] [PubMed] [Google Scholar]
- Computed tomography-an increasing source of radiation exposure. N Engl J Med. 2007;357:2277-84.
- [CrossRef] [PubMed] [Google Scholar]
- Patient exposure from radiologic and nuclear medicine procedures in the United States: Procedure volume and effective dose for the period 2006-2016. Radiology. 2020;295:418-27.
- [CrossRef] [PubMed] [Google Scholar]
- Radiogenic risk assessment for abdominal vascular computed tomography angiography. Radiat Phys Chem. 2020;168:108523.
- [CrossRef] [Google Scholar]
- Filariasis: Diagnosis and treatment. Dermatol Ther. 2009;22:475-90.
- [CrossRef] [PubMed] [Google Scholar]
- Normalised Organ Doses for X-ray Computed Tomography Calculated Using Monte Carlo Techniques United Kingdom: National Radiological Protection Board, Chilton; 2014.
- [Google Scholar]
- 2011. Available from: http://www.impactscan.org/ctdosimetry.htm [Last accessed on 2020 May 13]
- Diagnostic accuracy of lymphoscintigraphy for lymphedema and analysis of false-negative tests. Plast Reconstr Surg Glob Open. 2017;5:e1396.
- [CrossRef] [PubMed] [Google Scholar]
- Dose reduction in chest CT examination. Radiat Protec Dosim. 2015;165:185-9.
- [CrossRef] [PubMed] [Google Scholar]
- Patient dose considerations in computed tomography examinations. World J Radiol. 2010;28:262-8.
- [CrossRef] [PubMed] [Google Scholar]
- Communicating potential radiation-induced cancer risks from medical imaging directly to patients. Am J Roentgenol. 2015;205:962-70.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation doses in chest, abdomen and pelvis CT procedures. Radiat Prot Dosim. 2015;165:194-8.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation dose measurement in gastrointestinal studies. Radiat Prot Dosim. 2011;147:118-21.
- [CrossRef] [PubMed] [Google Scholar]






