Translate this page into:
Patient positioning during the radiographic procedure affects the radiological signs of acetabular retroversion - A systematic review

*Corresponding author: Marie Midtgaard, Department of Radiology, Hospital Lillebaelt, Kolding, Denmark. marie.midtgaard@rsyd.dk
-
Received: ,
Accepted: ,
How to cite this article: Midtgaard M, Vils Pedersen MR, Lyhne Christensen N, McKnight K, Jensen J. Patient positioning during the radiographic procedure affects the radiological signs of acetabular retroversion - A systematic review. J Clin Imaging Sci 2023;13:34.
Abstract
Young adults presenting with non-traumatic hip pain may suffer from acetabular retroversion (AR). The previous studies have suggested that patient positioning during the radiographic procedure, that is, pelvic tilt and/or rotation may alter the appearance of the acetabulum. The purpose of this systematic review was to explore and collate existing literature on the correlation between pelvic positioning in weight-bearing anterior-posterior radiographs and the radiographic signs of AR, namely, the ischial spine sign (ISS) the cross-over sign (COS) and posterior wall sign (PWS). The preferred reporting items for systematic reviews and meta-analysis guidelines were followed. MEDLINE, EMBASE, PubMed, The Cochrane Library, and CINAHL were searched. The search string included the following keywords: Pelvic, tilt, rotation, positioning, inclination, incidence, AR, ISS, COS, PWS, and acetabular version. Two authors independently screened the studies identified in the search, extracted data, and critically assessed included studies for quality using the Quality Assessment of Diagnostic Accuracy Studies 2 tool. In total, 2289 publications were screened. Fifteen articles were found eligible for full-text screening, and four articles met the inclusion criteria. Although the studies varied methodologically, all reported that pelvic positioning impacted radiographic signs of AR investigated. One study suggested that more than 9° of pelvic inclination would result in positive COS. No other benchmark values on the degree of pelvic tilt and rotation that would compromise the diagnosis of AR, that is, the detection of ISS, COS, and PWS were reported. At present, literature reporting on the correlation between patient positioning and AR is sparse. Four studies met the inclusion criteria, and they all reported a link between pelvic positioning and the radiographic appearance of AR.
Keywords
Pelvic positioning
Acetabular retroversion
Radiography
INTRODUCTION
Hip dysplasia is a condition ranging from simple to more complex disorders including a variety of deformities of the femoral-acetabular joint, and can cause early-onset hip osteoarthritis.[1] Patients often present with unspecific non-traumatic hip pain in early adulthood. Pelvic anterior-posterior (AP) radiographs are commonly used as the initial diagnostic tool for the investigation of dysplasia.[2] Acetabular retroversion (AR) is a subtype of hip dysplasia. The radiographic signs indicative of AR are (1) the ischial spine sign (ISS) where the ischial spine protrudes over the pelvic rim and is depicted as a triangular shape, (2) the cross-over sign (COS) is seen when the anterior wall of the acetabulum crosses over the posterior acetabular wall, and (3) the posterior wall sign (PWS) which indicates insufficient coverage of the femoral head and is seen when the center of the femoral head is projected lateral to the posterior border of the acetabulum [Figure 1].[3]
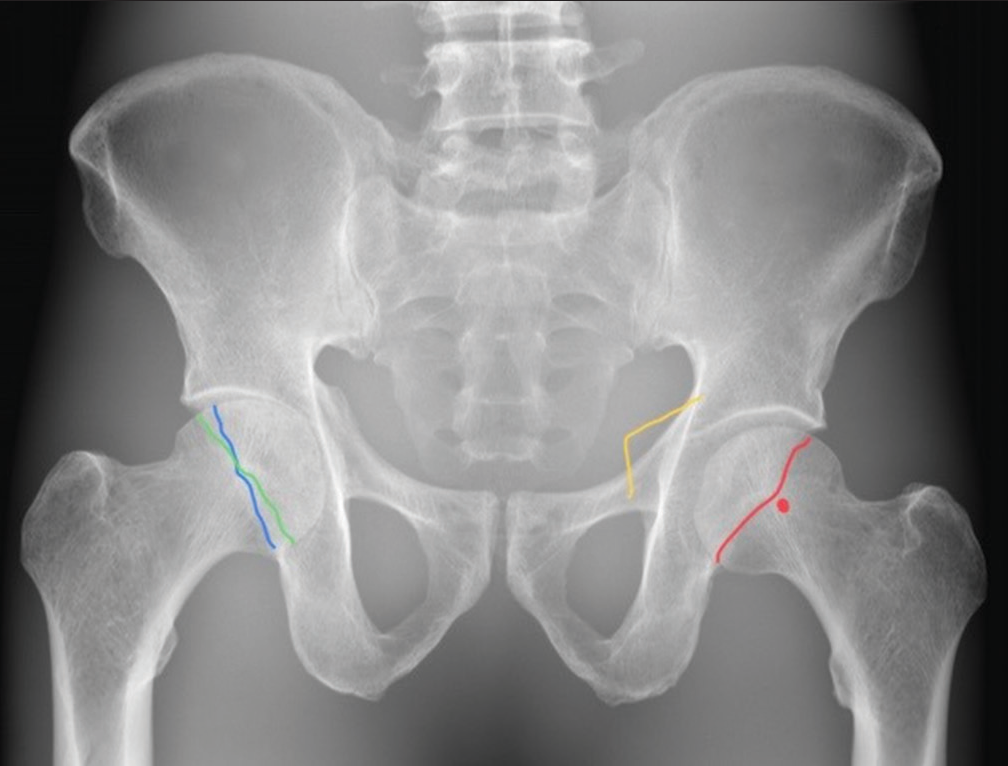
- Depiction of radiographic signs of acetabular retroversion. The ischial spine forms a triangular shape bilaterally in a frontal view of the pelvis. On a normal pelvic radiograph, the ischial spine will be superimposed by the medial aspect of the acetabulum. In case of positive ischial spine sign the ischial spine projects medially to the illiopelvic line of the pelvis and protrude into the pelvic cavity, as depicted by the yellow line. On a true anterior-posterior (AP) radiograph of the pelvis, the anterior rim of the acetabulum will project medial to the posterior rim without intersecting each other in normal hips. The cross-over sign is seen when the anterior and posterior rim of the acetabulum form a “figure of eight” sign by intersecting in the proximal and lateral aspects of the joint socket, as depicted by the blue and green lines. The posterior wall sign indicates a deficient posterior acetabulum, where the outline of the posterior acetabular wall projects (red line) medial to the center of the femoral head (red dot). In a true AP radiograph of the pelvis, normal hips will present with the outline of the posterior acetabular wall overlapping the center of the femoral head.
It has been suggested, that patient positioning during the radiographic procedure, that is, pelvic tilt and/or rotation, may compromise the anatomic appearance of the pelvic bones and potentially impact the diagnostic accuracy when investigating radiographic signs of AR.[4] The diagnostic accuracy of AR on the pelvic radiograph may be correlated to patient positioning during the radiographic procedure. Therefore, the appearance of AR in a mal-positioned radiograph may be positional as opposed to a reliable indicator of anatomical abnormality. Hence, the diagnostic value of a pelvic radiograph may theoretically be dependent on individual radiographer skills, making anatomical knowledge and positioning skills of the performing radiographer highly important.
This systematic review aims to explore and collate the impact of pelvic tilt and/or rotation on the radiographic signs of AR in comparison to the non-tilted and non-rotated (reference standard) in adults. The specific objectives were to outline existing evidence between patient positioning and the radiographic signs of (1) ISS, (2) COS, and (3) PWS.
MATERIAL AND METHODS
The preferred reporting items for systematic reviews and meta-analysis protocols (PRISMA-P) guidelines were followed, and this systematic review was registered at the International Prospective Register of Systematic Reviews (PROSPERO) (ID-number: CRD42022315758).[5]
Search and screening
A search string was developed inspired by the patient, intervention, comparison, and outcome (PICO) format, to understand the research question from various perspectives. The PICO tool helps to provide predefined eligibility criteria for the literature search.[6]
The following words were applied to the search string: Pelvic, tilt, rotation, positioning, inclination, incidence, AR, ISS, COS, PWS, and acetabular version. The search string was modified and adapted to suit the relevant scientific databases. One author (MM) developed the search with input from a science librarian employed by the City University of Birmingham, United Kingdom.
The electronic bibliographic databases CINAHL (EBSCOhost interface), MEDLINE (EBSCOhost interface), EMBASE (OVID interface), PubMed (NIH), and The Cochrane Library (Wiley interface) were searched on September 27, 2021, and repeated on May 4, 2023. The MEDLINE search is presented in Table 1.
| S1 (MH “Pelvic Tilt”) |
| S2 (MH “Tilt”) |
| S3 (MH “Rotation”) |
| S4 (MH “Orientation”) |
| S5 (MH “Patient Positioning”) |
| S6 “Pelvic inclination” |
| S7 “Inclination” |
| S8 “Pelvic incidence” |
| S9 (MH “Incidence”) |
| S10 “Acetabular Retroversion” |
| S11 “Ischial Spine Sign” |
| S12 “Cross Over Sign” |
| S13 “Posterior Wall Sign” |
| S14 “Acetabular Version” |
| S15 “S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9” |
| S16 “S10 OR S11 OR S12 OR S13 OR S14” |
| S17 “S15 AND S16” |
Eligibility criteria
Studies comparing pelvic positioning to the presence of the radiographic signs of ISS, COS, and PWS were eligible for inclusion. Studies assessing the morphology of AR post-surgical or post-traumatic were excluded, since intervention or trauma can alter the anatomic appearance of the pelvis. Studies on patients younger than the age of 18 were excluded to ensure comparable studies with patients of full skeletal maturity. Studies involving acquired or congenital bone deformities other than AR were excluded from the study. No restrictions regarding language, location, study type, or date of publication were applied. Moreover, The International (PROSPERO) was searched for relevant ongoing or recently completed reviews.
All identified records were uploaded to a bibliographic database, where an initial duplicate search was made. The remaining records were uploaded to Covidence®, where a second duplicate search was made. In Covidence, two authors (MM and NLC) individually screened based on title and abstract. Next, the studies potentially eligible for inclusion were full-text-screened by the same two authors. Reasons for exclusion at full-text stage were recorded. The reference lists of included articles were scanned for eligible articles. Moreover, the “find-similar” feature in databases was used on all included articles.
Data extraction and quality assessment
A data extraction form downloaded from the Cochrane Handbook was used to develop a data extraction template.[6] Two authors piloted the data extraction template and extracted data independently. In case of discrepancy, disagreement would be resolved by one of the co-authors (JJ). All included studies were assessed for methodological quality using a modified Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool, where flow and timing were kept out, since all images were taken in the same consecutive setting. The QUADAS-2 tool aids with transparency of bias and applicability when assessing diagnostic accuracy.[7]
Outcome
The primary outcome was to estimate the impact of patient positioning, that is, pelvic tilt and rotation, on the presence or absence of the radiographic signs of AR, that is, ISS, COS, and PWS.
RESULTS
Search and screening
In total 2289 articles were identified and uploaded to EndNote, a reference management tool where an initial duplicate search reduced the number of articles to 2138. A second removal of duplicates was made after uploading to Covidence® which reduced the number of articles eligible for screening to 2090. Initial screening based on title and abstract against inclusion/ exclusion criteria resulted in 20 articles eligible for full-text screening. Following full-text screening, three articles were eligible for inclusion. A fourth article by Siebenrock et al. was found by snowballing the reference list of Kakaty et al.[4,8] Figure 2 shows the inclusion/exclusion flowchart.
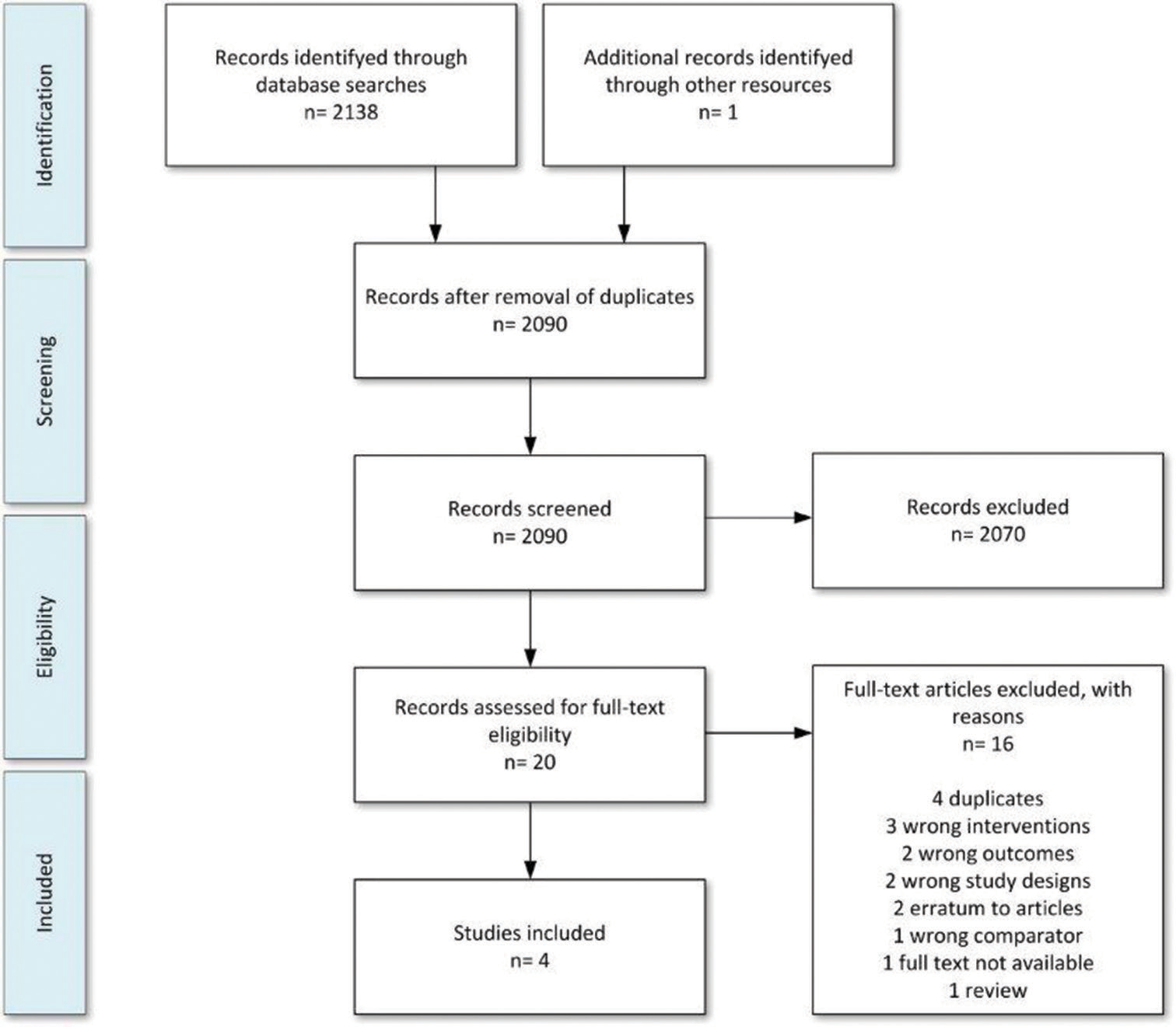
- Preferred reporting items for systematic review and meta-analysis flowchart showing the study selection process.
The four included studies differed methodologically regarding sample size, investigated radiographic signs of AR, whether they investigated tilt and/or rotation of the pelvis as well as their definition of a reference standard. Three studies included cadavers and one study in vivo patients. All these factors contribute to the heterogeneity of methodological approaches and potentially outcomes. Combined with the fact, that only four studies were identified, a narrative approach to data synthesis was applied using the SWiM guidelines.[9] In Table 2, the descriptive information and the results are presented.
| Author and year | Radiographic signs of AR: ISS COS PWS |
Study population Cadaver/in vivo (No.) |
Intervention and range: Rotation Tilt | Evaluated by: Orthopedic surgeon Radiologist Other |
Reference of pelvic neutral positioning | Impact of tilt on radiographic signs of AR? | Impact of rotation on radiographic signs of AR? |
|---|---|---|---|---|---|---|---|
| Tannast et al., 2015 |
COS PWS |
In vivo (101) Cadavers (20) |
Tilt Rotation |
Orthopedic surgeons | Neutral rotation: The midline of the sacrococcygeal joint falling directly over the symphysis pubis | Pelvic tilt affects the appearance of PWS and COS | Pelvic rotation affects the appearance of PWS and COS |
| Kakaty et al., 2010 |
ISS | Cadavers (20) | Tilt Rotation |
Orthopedic surgeons | Neutral tilt: 60° inclination angle Neutral rotation: The midline of the sacrococcygeal joint falling directly over the symphysis pubis |
Pelvic tilt affects the appearance of ISS | Pelvic rotation affects the appearance of ISS |
| Siebenrock et al., 2003 | COS PWS |
Cadavers (4) | Tilt Rotation |
Orthopedic surgeons | Neutral tilt: the distance between the symphysis pubis and the sacrococcygeal joint. Neutral rotation: alignment of the coccyx over the symphysis and symmetric appearance of the pelvic structures |
Pelvic tilt affects the appearance of PWS and COS | Pelvic rotation affects the appearance of PWS and COS |
| Jackson et al., 2016 |
COS ISS |
In vivo (46) | Tilt (standing vs. supine) | Orthopedic surgeons | Not reported – compared standing vs. supine | Pelvic tilt affects the appearance of COS and ISS. | Not relevant |
AR: Acetabular retroversion, ISS: Ischial spine sign, COS: Cross -over sign, PWS: Posterior wall sign
Quality assessment of included studies
Regarding the assessment of the risk of bias and applicability concerns the overall quality of the included studies was high, even though one of the studies lacked a definition of a reference standard, and thereby may have introduced bias.[10] The remaining three of the included studies clearly defined the interpretation and conduct of the index test and the reference standard, and limited applicability concerns were noted regarding these biases.[4,8,11] The QUADAS-2 results from the quality assessment of the four articles are presented in Table 3.
| Study | Risk of bias (a) | Applicability concerns (b) | ||||
|---|---|---|---|---|---|---|
| Patient selection | Index test | Reference standard | Patient selection | Index test | Reference standard | |
| Tannast et al. 2015 | ? |  |
 |
? |  |
 |
| Kakaty et al. 2010 | ? |  |
 |
? |  |
 |
| Siebenrock et al. 2003 | ? |  |
 |
? |  |
 |
| Jackson et al. 2016 |  |
 |
 |
 |
 |
 |
 : Low risk,
: Low risk,  : High risk, ?: Unclear. QUADAS-2: Quality assessment of diagnostic accuracy studies
: High risk, ?: Unclear. QUADAS-2: Quality assessment of diagnostic accuracy studies
OBJECTIVES
Patient positioning and the ISS
Two studies explored the ISS and both studies reported that pelvic tilt affected the radiographic appearance of the ISS although no estimates of the exact degree of tilt/rotation needed to compromise the validity of the radiographic appearance of the ISS was offered.[8,10]
The definition of reference standard varied in the studies. Kakaty et al. defined their reference standard of neutral rotation as the midline of the sacrococcygeal joint falling directly over the symphysis pubis and the reference standard of neutral tilt as a 60° inclination angle.[8]
The study by Jackson et al. compared differences in pelvic tilt between standing and supine radiographs, providing no clear definition of a reference standard, as the positions were individual for each patient. Despite the variation in reference standard, both aforementioned studies found that an increase in pelvic tilt leads to an increase in the detection of ISS.[8,10]
Patient positioning and the COS
The three studies by Tannast et al., Siebenrock et al., and Jackson et al. investigated the radiographic appearance of COS and found that it was affected by either pelvic tilt, pelvic rotation, or both.[4,10,11] Tannast et al. and Jackson et al. provided no evaluations on margins for when tilt and rotation of the pelvis would compromise the detection of COS.[10,11] However, Siebenrock et al. reported that pelvic inclination of more than 9 ° from the neutral positioning resulted in a positive COS.[4] In all three studies, the results showed that a decrease in pelvic tilt caused a decrease of the detection of COS. Tannast et al. and Siebenrock et al. concluded that both pelvic tilt and rotation compromised the validity and detection of COS. Siebenrock et al. showed that pelvic rotation could result in both the absence and presence of COS, depending on the rotation being contralateral or ipsilateral, respectively.[4,11]
Patient positioning and the PWS
Tannast et al. and Siebenrock et al. applied the same definition of a reference standard for neutral tilt and rotation and investigated the effect of pelvic tilt and rotation on the presence of PWS in images made on cadavers. Both studies found that a decrease in pelvic tilt would cause a decrease in the detection of PWS and an-increase/decrease in PWS when pelvis rotation was ipsilateral/contralateral, respectively.[4,11] A benchmark value of 9° was reported as the angle that would affect the presence of PWS.[4]
DISCUSSION
This is, to the best of the authors knowledge, the first systematic review made on the correlation between pelvic positioning and the diagnostic accuracy of the radiographic signs ISS, COS, and PWS. Four studies met the inclusion criteria, and they varied in applied methodology and presentation of findings. However, they all reported that pelvic tilt and rotation affected the detectability of ISS, COS, and PWS.[4,8,10,11] Even though all the included studies reported that pelvic positioning had an impact on the radiographic visualization of ISS, COS, and PWS, only Siebenrock et al. reported a specific degree of mal-positioning which would influence the detectability of COS and PWS.[4] In addition, the study by Jackson et al. lacks comparison with a predefined reference standard, which compromises the validity and the reproducibility of the study.[10]
The cadaveric specimens in three of the studies were all missing femurs and were all free of the normal soft tissues. The lack of soft-tissue decreases the absorption in the radiographs, which affects the image quality.[4,8] Without the soft tissue, the dry cadaver specimens had a more homogeneous absorption of the radiation. With bone as the only absorption in the images, the image contrast was increased making the structures, such as the acetabular rims, easier to define - The clear delineation of anatomical structures was further enhanced by the missing femoral heads. Moreover, the acetabular rims of the cadavers were all marked with a metal wire for increased detectability of the acetabular and COS.[4,8,11] This is not representative of a normal radiographic setting where the detectability of the acetabular rims is not enhanced by physical markings and can result in over or under diagnosis in the included studies. An overdiagnosis was suggested by Jackson et al. who highlighted that 68% of their images showed a positive COS, which was considerably higher than the reported incidence of 5% in the normal population.[10] This may, however, be in line with studies suggesting that hip dysplasia, and other developmental conditions of the hip, may be under-diagnosed radiographically.[10,12]
It should also be taken into consideration that individuals and specimens who do not have AR will not show positive signs of ISS, COS, and/or PWS in their neutral-positioned pelvis radiograph, but could according to the four included studies, produce false-positive signs when the pelvis is tilted and/or rotated.[4,8,10,11]
The subjective evaluation of the presence or absence of ISS, COS, and PWS calls for a clear definition of what exactly to investigate in the radiographs. When assessing PWS, the center of the femoral head needs to be identified. However, none of the studies provide information on how they accounted for the impact of the missing femoral head when evaluating PWS. Without knowing if the specimen has a non-pathological morphology of the acetabulum, it can be challenging to establish the center of the normal hip. Furthermore, missing soft tissue of the specimens resulted in missing structures like cartilage that normally creates a joint space distance from the femoral head to the acetabular socket, adding further insecurity to the assessment of PWS. The findings of the studies on the detectability of PWS, and how it was affected by pelvic tilt and rotation, were therefore compromised in terms of generalizability to the clinical setting.
The European Guidelines on Quality Criteria for Diagnostic Radiographic Images highlight and underpins the importance of neutral rotation in radiographs of the pelvis, defined as a symmetrical reproduction of the pelvis judged by the midline of the sacrum falling directly over the center of the symphysis pubis.[13] This definition is similar to the reference standard employed in three of the included studies.
Findings in the included studies suggested that patient positioning during the acquisition of a pelvis radiograph may compromise the diagnostic value and perhaps even produce both false negative and false positive signs of AR.[4,8,10,11] This highlights the need for detailed and evidence-based radiographic positioning guidelines for the radiographers to consult before obtaining radiographs of the pelvis, particularly when dysplasia may be suspected. The diagnostic value of a well-positioned and well-exposed radiograph of the pelvis must be emphasized and calls for high-quality radiographic work.
The use of cadaveric specimens in three of the included studies does impose a limitation regarding generalizability to the clinical setting. Moreover, the inherent limitation of this review is the limited number of studies that were eligible for inclusion, making the results difficult to generalize. This however highlights the importance of further research on this topic, to underline the need to focus on the diagnostic value of a well-positioned radiograph of the pelvis when clinically suspecting hip dysplasia.
CONCLUSION
All four included studies reported an effect of pelvic tilt and/ or rotation on the detection of the radiographic signs ISS, COS, and PWS on AP radiographs of the pelvis. However, the limited number of included studies combined with heterogeneity of included studies makes it difficult to generalize the impact of patient positioning on diagnostic accuracy. Still, the results do indicate, that patient positioning during the radiographic procedure needs to be in focus to improve diagnostic accuracy benefitting the patient.
IMPLICATIONS FOR PRACTICE
The findings in this systematic review do emphasize the importance of prioritizing patient positioning during radiographic procedures. By adhering to positioning guidelines, radiographers can improve diagnostic accuracy and potentially enhance patient outcomes. Particularly, since patient positioning during the acquisition of pelvic radiographs, in theory, may alter the radiologic diagnosis of AR.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Hip dysplasia in the young adult caused by residual childhood and adolescent-onset dysplasia. Curr Rev Musculoskelet Med. 2016;9:427-34.
- [CrossRef] [PubMed] [Google Scholar]
- Femoroacetabular impingement. Arthritis Rheumatol. 2015;67:17-27.
- [CrossRef] [PubMed] [Google Scholar]
- Acetabular retroversion: Diagnosis and treatment. EFORT Open Rev. 2018;3:595-603.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of pelvic tilt on acetabular retroversion: A study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241-8.
- [CrossRef] [PubMed] [Google Scholar]
- Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
- [CrossRef] [PubMed] [Google Scholar]
- Cochrane handbook for systematic reviews of interventions version 6.2 Cochrane Training. 2021. Available from: https://training.cochrane.org/handbook/current [Last accessed on 2021 Aug 31]
- [Google Scholar]
- QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529-36.
- [CrossRef] [PubMed] [Google Scholar]
- The ischial spine sign: Does pelvic tilt and rotation matter? Clin Orthop Relat Res. 2010;468:769-74.
- [CrossRef] [PubMed] [Google Scholar]
- Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ. 2020;368:l6890.
- [CrossRef] [PubMed] [Google Scholar]
- Supine and standing AP pelvis radiographs in the evaluation of pincer femoroacetabular impingement. Clin Orthop Relat Res. 2016;474:1692-6.
- [CrossRef] [PubMed] [Google Scholar]
- Which radiographic hip parameters do not have to be corrected for pelvic rotation and tilt? Clin Orthop Relat Res. 2015;473:1255-66.
- [CrossRef] [PubMed] [Google Scholar]
- A deep learning algorithm for radiographic measurements of the hip in adults-a reliability and agreement study. Diagnostics (Basel). 2022;12:2597.
- [CrossRef] [PubMed] [Google Scholar]
- European guidelines on quality criteria for diagnostic radiographic images Brussels: European Commission; 1996.
- [Google Scholar]







