Translate this page into:
Paratesticular Liposarcoma: A Radiologic Pathologic Correlation
Address for correspondence: Dr. Ahmet Pergel, Department of Surgery, School of Medicine, Rize University, 53100, Rize, Turkey. E-mail: pergelahmet@hotmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Spermatic cord liposarcoma is an uncommon paratesticular tumor. Patients usually present with a painless scrotal or inguinal mass, mimicking inguinal hernia. Clinical examination suggested an inguinal hernia. Computed tomography demonstrated a fat-containing mass in the right inguinal region. The mass was surgically removed, along with the right testis and spermatic cord. Histopathological examination revealed a well-differentiated liposarcoma. No evidence of recurrence or metastases has been noted during the two-year follow-up with postoperative adjuvant therapy.
Keywords
Cord liposarcoma
inguinal hernia
inguino-scrotal mass
INTRODUCTION

Liposarcoma of the spermatic cord is a rare malignant neoplasm that accounts for 3% to 7% of all sarcomas. Although 20% of liposarcomas originate in the retroperitoneum, only 0.1% manifest as incidental inguinal hernias.[1] The majority of spermatic cord sarcomas begin their development just below the external inguinal ring and therefore grow as a scrotal mass, rather than as an inguinal mass.[2]
We report the radiologic and pathologic features of an 81-year-old male patient with liposarcoma of the spermatic cord that mimicked an incarcerated right scrotal inguinal hernia. Our patient presented with complaints of a progressively increasing swelling in his right inguino-scrotal region for one year that had grown rapidly during the last three months. Physical examination revealed a mass in the right inguino-scrotal region 10 cm in size that was firm, non-tender, irreducible, and painless. Routine laboratory results were within normal limits.
RADIOLOGIC FEATURES
On a CT scan, well-differentiated liposarcoma typically has a characteristic appearance of a predominantly adipose mass containing nonlipomatous components. Generally, fat composition of a well-differentiated liposarcoma is greater than 75% of the tumor. The non-lipomatous component is often seen as a prominent thick septa (>2 mm) that may show nodularity.[3] Benign lipomas and hernias containing omentum are potential mimics. Lipomas are generally smaller and more homogeneous and hernias are elongated masses that can be often traced back to the inguinal canal.[4]
In our case, the ultrasound examination revealed a solid, hyperechoic, and heterogeneous mass lesion in the right inguino-scrotal region. CT demonstrated a fat-containing mass with a nodular enhancement extending below the external inguinal ring into the scrotum. There was no radiographic evidence of any regional lymph node or distant metastatic disease [Figure 1].
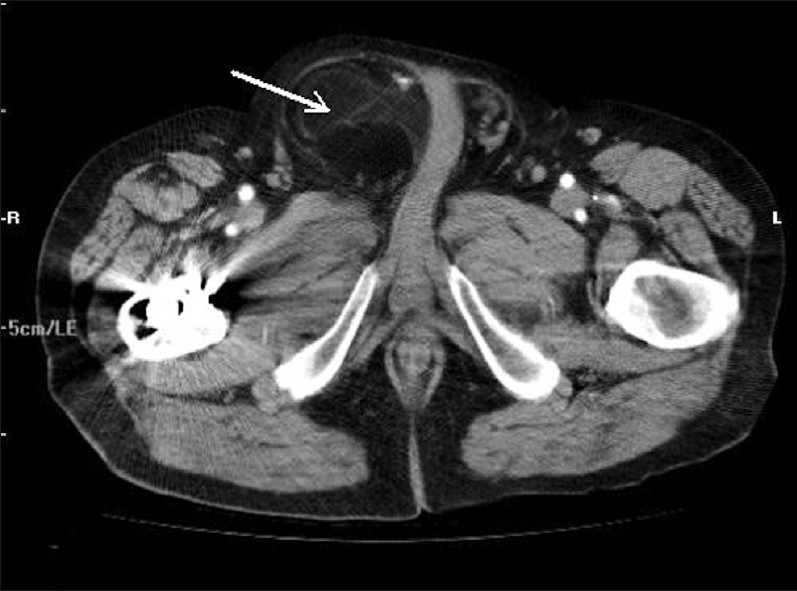
- Computed tomography image demonstrates a lipomatous mass (arrow).
PATHOLOGIC FEATURES
Patient underwent radical right orchiectomy with high ligation of the spermatic cord, together with wide excision and scraping of neoplastic tissue from the inguinal and scrotal region. The gross appearance of the specimen revealed a large, soft, well-circumscribed, multilobulated, fat-containing mass adhering to the spermatic cord and testis. There was no obvious hernial sac [Figure 2]. The histopathologic evaluation revealed a well-differentiated liposarcoma containing lipoblasts and spindle-shaped cells with hyperchromatic nuclei within the fibromyxoid stroma [Figure 3].

- Gross examination of the mass revealed a large, encapsulated, yellow-brown colored fatty tissue measuring 27×18×4.5 cm. The mass weighed 858 gm, with variable consistency on palpation. In addition, atrophic testis was adherent to the mass and measured 3×2.5×1.5 cm in size.
![(a and b) Microscopic examination of the mass revealed an encapsulated proliferation consisting of mature adipocytes accompanied by both spindle shaped cells with hyperchromatic nuclei within the stromal tissue and multivacuolated lipoblasts in between on a partly fibrous and partly myxoid background. In addition to Leydig cell hyperplasia, widespread atrophy and hyalinization were detected within the seminiferous tubules in the cross-sections of the testicular tissue. [Hematoxilyn and Eosin stain, (a) ×100 and (b) ×400].](/content/12/2011/1/1/img/JCIS-1-57-g004.png)
- (a and b) Microscopic examination of the mass revealed an encapsulated proliferation consisting of mature adipocytes accompanied by both spindle shaped cells with hyperchromatic nuclei within the stromal tissue and multivacuolated lipoblasts in between on a partly fibrous and partly myxoid background. In addition to Leydig cell hyperplasia, widespread atrophy and hyalinization were detected within the seminiferous tubules in the cross-sections of the testicular tissue. [Hematoxilyn and Eosin stain, (a) ×100 and (b) ×400].
The patient's postoperative course was uneventful and he was discharged from the hospital on the second postoperative day. The patient received adjuvant radiotherapy and during the follow-up period of 2-years remained free of disease, with no evidence of any local recurrence or distant metastasis.
DISCUSSION
Patients with paratesticular liposarcoma usually present in their fifties or sixties, with an age range of 16 to 87 years. A palpable scrotal or inguinal mass is the most common finding; the differential diagnosis includes inguinal hernia, hydrocele, and chronic epididymitis.[5] Liposarcomas are more often located in the lower extremities (41%), the retroperitoneum (19%), and the inguinal region (12%).[6]
The typical clinical characteristics of a well-differentiated liposarcoma are a painless, slow-growing (months to years) soft-tissue mass. However, pain and tenderness have been reported in 10–15% of the cases.[3] Rapid growth, large size, and symptomatic presentation are features suggestive of malignancy. Tumors range from 3 to 30 cm in diameter and are gray-white to yellow-tan in color. Most tumors are lobulated or nodular, and necrosis and hemorrhage may be present. Fibrous septa dividing the tumor into smaller lobules may be present. Liposarcomas involve the spermatic cord more commonly than the testicular tunics.[5]
The patient in our case was 81 years old. Although he had noticed the swelling in his right inguinal region one year earlier, he did not seek any medical advice. He became troubled about his condition only after the progressive increase in the size of the inguinal mass accelerated during the last three months. He was operated on with the diagnosis of an incarcerated inguinoscrotal hernia. After exposing the field, we found that it was extremely difficult to distinguish with the naked eye the right testis from the mass macroscopically. The mass was yellow-tan in color and was organized in lobular units. Appearance of the right testis was atrophic due to probable tumor pressure.
The World Health Organization (WHO) Committee for the Classification of Soft Tissue Tumors in 2002 categorized soft-tissue liposarcomas into five types: Well-differentiated, dedifferentiated, myxoid, pleomorphic, and mixed.[78] A well-differentiated liposarcoma is a low-grade neoplasm with five histologic variants: Lipoma-like, sclerosing, inflammatory, spindle cell, and liposarcoma with meningothelial whorls (which may indicate early dedifferentiation).[7] The present case was a well-differentiated liposarcoma.
A well-differentiated liposarcoma has no metastatic potential unless dedifferentiation occurs, but lesions may recur locally. The prognosis and treatment of well-differentiated liposarcomas are therefore closely related to the anatomical locations of the lesions.[9]
Subcutaneous liposarcomas are treated adequately with wide surgical excision, including a cuff of surrounding normal tissue. With adequate initial resection, local recurrence of subcutaneous lesions is rare to nonexistent, as reported by Azumi and colleagues.[10]
The rate of local recurrence is 70% for groin lesions and 91% for retroperitoneal lesions.[7911] In these cases, radiation therapy may be employed as an adjunct to surgical resection in an attempt to avoid local recurrence.[2] Although radiotherapy is considered to be an effective adjunct to surgery for soft tissue sarcomas at other sites, little data are available regarding the radiation dosage required for adjuvant radiotherapy for para-testicular sarcomas.[1]
In our case, in addition to radical orchiectomy, postoperative radiotherapy was employed and there has been no signs of any local recurrence during our two-year follow-up period.
The rarity of an inguinal liposarcoma makes it very difficult to differentiate it from an incarcerated inguinal hernia. Radiologists should be aware of this entity. Paratesticular liposarcoma should be considered as a possibility during the differential diagnosis of fat containing inguino-scrotal mass.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/57/90952
REFERENCES
- Incidental liposarcomas identified during hernia operations. J Surg Oncol. 1999;71:50-3.
- [Google Scholar]
- From the archives of the AFIP: imaging of musculoskeletal liposarcoma with radiologic-pathologic correlation. Radiographics. 2005;25:1371-95.
- [Google Scholar]
- Malignant fatty tumors: Classification, clinical course, imaging appearance and treatment. Skeletal Radiol. 2003;32:493-503.
- [Google Scholar]
- Miscellaneous primary tumors of the testis, adnexa, and spermatic cord. In: Rosai J, Sobin LH, eds. Atlas of tumor pathology, fasc 25, ser 3. Washington, DC: Armed Forces Institute of Pathology; 1999. p. :235-366.
- [Google Scholar]
- Adipocytic tumors. In: WHO classification of tumors. Pathology and genetics: Tumors of soft tissue and bone. Lyon, France: IARC; 2002. p. :19-46.
- [Google Scholar]
- Malignant lipomatous tumors. In: Atlas of tumor pathology: Tumor of the soft tissue. Washington DC: Armed Forces Institute of Pathology; 2001. p. :217-38.
- [Google Scholar]
- Surgical management of malignant soft-tissue tumors. In: Simon MA, Springfield DS, eds. Surgery for bone and soft-tissue tumors. Philadelphia Pa: Lippincott-Raven; 1998. p. :555-65.
- [Google Scholar]
- Atypical and malignant neoplasms showing lipomatous differentiation.A study of 111 cases. Am J Surg Pathol. 1987;11:161-83.
- [Google Scholar]
- Chemotherapy, irradiation, and surgery for function- preserving therapy of primary extremity soft tissue sarcomas: İnitial treatment with ifosfamide, mitomycin, doxorubicin, and cisplatin plus granulocyte macrophage-colony-stimulating factor. Cancer. 2002;94:786-92.
- [Google Scholar]






