Translate this page into:
Obstructive Uropathy Secondary to Uretero-inguinal Hernia
Address for correspondence: Dr. Lih En Hong, Department of General Medicine, Flinders Medical Centre, Flinders Drive, Bedford Park - 5042, South Australia, Australia. E-mail: LihEn.Hong@health.sa.gov.au
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Uretero-inguinal hernia in patients with native kidneys is rare. We report a case of an 84-year-old man who was diagnosed with obstructive uropathy secondary to uretero-inguinal hernia, with no past history of herniorrhaphy or congenital genitourinary malformation. Uretero-inguinal hernias are predominantly indirect inguinal hernias and may be paraperitoneal or extraperitoneal. Computed tomography (CT) is a non-invasive diagnostic tool for uretero-inguinal hernia. Herniorrhaphy is indicated in all cases of uretero-inguinal hernia to prevent obstructive uropathy.
Keywords
Hernia
inguinal hernia
obstructive uropathy
uretero-inguinal

INTRODUCTION
Inguinal hernia is a common presentation in male patients. However, inguino-scrotal herniation of the ureter, also described as uretero-inguinal hernia, is a rare presentation. This presentation can potentially cause obstructive uropathy or serious surgical complications to the ureter during surgery if unrecognized. Uretero-inguinal hernia in patients with native kidneys is rare, with some cases identified as a cause of renal failure.[1] We report a case of obstructive uropathy secondary to uretero-inguinal hernia.
CASE REPORT
An 84-year-old male presented with a 2-week history of increased exertional dyspnea and worsening peripheral edema. His significant past medical history included chronic kidney disease with baseline serum creatinine of 235 μmol/l (reference range: 80–120 μmol/l), which is likely secondary to renovascular cause, ischemic heart disease, congestive heart failure, paroxysmal atrial fibrillation, prostate cancer, and hypertension. On examination, there were clinical signs consistent with pulmonary edema. A large, 15 cm × 10 cm × 10 cm left partial reducible inguinoscrotal hernia was found on abdominal examination. The patient reported the hernia had been present for over 5 years but had not caused any problems. He was diagnosed with decompensated congestive heart failure, acute deterioration of renal function in setting of known chronic renal failure with serum creatinine peaking at 408 μmol/l, and acute urinary retention for which a urinary catheter was inserted.
Investigations to ascertain the patient's deterioration in renal function included ultrasound of the renal tract which showed significant hydronephrosis of the left kidney and left proximal hydroureter. The left distal ureter was not identified. A mass measuring 7 cm was also noted on the right kidney. Ultrasound of the left inguinal region for possible wall defect was not performed as there was no plan for surgical repair. The renal findings were further assessed with a computerized tomography (CT) scan of the abdomen, which confirmed severe left hydronephrosis with a dilated left ureter tracking into a large left indirect inguinal hernia which also contained a non-dilated loop of sigmoid colon [Figures 1a and 2]. Ureteric collapse beyond this point was consistent with ureteric obstruction. The CT scan also identified a heterogeneous calcified right renal mass, favored to reflect a renal cell carcinoma [Figures 1b and 2]. A radionuclide renal scan with technetium-labeled mercaptoacetyltriglycine (Tc99m-MAG3) showed poor perfusion and function of the left kidney, which accounted for approximately 21% of the total renal function. The right renal mass was biopsied with pathology confirming a papillary renal cell carcinoma. In view of his significant comorbidities, he was treated conservatively. He passed away 3 months later due to progressive congestive heart failure.
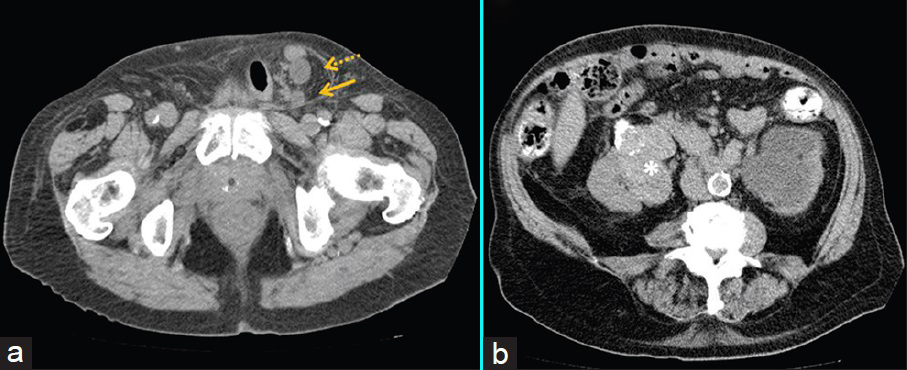
- 84-year-old man with acute deterioration of renal function in setting of known chronic renal failure diagnosed with obstructive uropathy secondary to uretero-inguinal hernia. (a) Axial image of a non-contrast computed tomography (CT) scan of the abdomen demonstrates the left ureter entering (dashed arrow) and exiting (solid arrow) a left indirect inguinal hernia with a hydronephrotic left kidney. (b) Axial image of a non-contrast CT scan of the abdomen shows a heterogeneous, calcified solid right renal mass (asterisk), diagnosed as a papillary renal cell carcinoma.
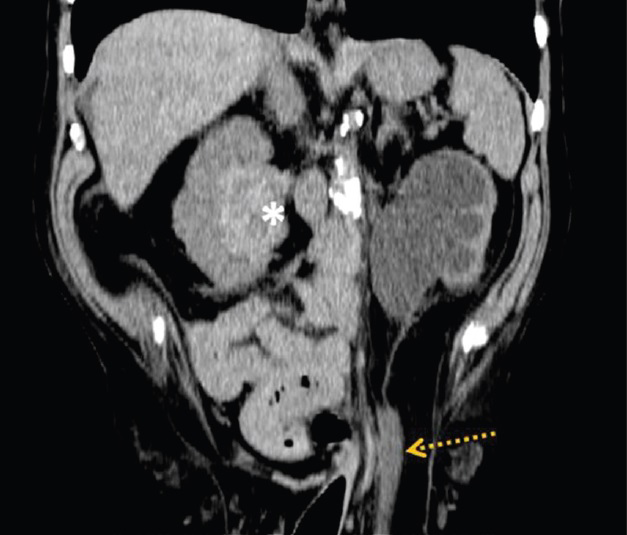
- 84-year-old man with acute deterioration of renal function in setting of known chronic renal failure diagnosed with obstructive uropathy secondary to uretero-inguinal hernia. Coronal image of a non-contrast CT scan of the abdomen demonstrates the left ureter entering a left indirect inguinal hernia (dashed arrow) and a calcified solid renal mass on the contralateral kidney (asterisk).
DISCUSSION
Uretero-inguinal hernias are predominantly indirect inguinal hernias and may be paraperitoneal or extraperitoneal.[1] Paraperitoneal hernia is the more common variant, accounting for approximately 80% of all cases.[1] It occurs when the ureter is adherent to the posterior peritoneum and is herniated alongside the peritoneal sac into the inguinal canal. It is often accompanied by herniation of other organs such as the colon.[2] In extraperitoneal herniation, the ureter herniates without the peritoneal sac. This was initially thought to be related to a congenital embryonic defect resulting in fusion of the ureter and genitoinguinal ligaments.[1] Previous case reports have demonstrated occurrence of uretero-inguinal hernias in the absence of congenital anomalies or prior hernia repair.[23] Other risk factors of uretero-inguinal hernia include obesity and deficiency in collagen synthesis.[4]
Early diagnosis of uretero-inguinal hernia is important because it can cause chronic renal impairment due to obstructive uropathy as in this case. Furthermore, it increases the risk of iatrogenic ureteral injury during hernia repair if undiagnosed.[4] While several cases of uretero-inguinal hernia reported in literature were identified preoperatively during radiological investigation for urinary symptoms,[134] a number of cases have also been diagnosed during hernia repair.[34] Previous reports have emphasized the importance for pre-operative diagnosis to reduce the risk of ureteral injury during surgery,[345] although this can be challenging if the patient is not acutely symptomatic. A degree of clinical suspicion is, therefore, required in patients presenting with renal function deterioration on a background of known hernia.
Ultrasound examination is an ideal first-line imaging modality for renal tract assessment and can reliably identify hydronephrosis and proximal hydroureter.[6] Confirmation of the site of obstruction and diagnosis of rare etiologies such as uretero-inguinal hernia requires a degree of prior clinical suspicion. The tracking of the ureter can be challenging due to its retroperitoneal location, and ultrasound imaging of the renal tract does not routinely include assessment of the inguinal orifices. Identification of the site and etiology of renal tract obstruction is more reliably assessed on cross-sectional imaging, which also allows anatomical classification of any hernias identified. Magnetic resonance imaging (MRI) can provide satisfactory assessment of the renal tract and has been shown to reliably identify uretero-inguinal hernias,[67] but may not be a viable alternative for patients in remote locations or with previous surgical stents and implants. Non-contrast CT remains the most easily accessible cross-sectional imaging modality for assessment of renal obstruction. The ultra-low-dose scanning protocol now enables assessment for renal tract pathology at radiation doses nearly equivalent to a plain abdominal X-ray.[89] The corresponding ionizing radiation risk is significantly lowered, but not completely eliminated. Scanning should remain limited to patients in whom there is clinical suspicion of pathology and whose management will be altered based on results.
Herniorrhaphy is indicated in all cases of uretero-inguinal hernia to prevent obstructive uropathy.[3] If present, management of obstructive uropathy includes insertion of a nephrostomy tube or nephroureteral stent.[10] Stent insertion enables identification and protection of the ureter during herniorrhaphy,[5] but endourologic insertion of the stent can be technically difficult due to the length and tortuosity of the ureter.[2] During herniorrhaphy, the ureter is carefully dissected from the hernia sac and returned to the retroperitoneal compartment.[5] In our case, clinical management of the hernia and associated left-sided obstructive uropathy was further complicated by the presence of a renal cell carcinoma on the right kidney.
CONCLUSION
Uretero-inguinal hernia is a rare condition, but can be a potential cause of obstructive uropathy. Low-dose non-contrast CT is currently the modality of choice for diagnosis of uretero-inguinal hernias, allowing identification and anatomical classification of the hernia as well as demonstrating any associated complications. Clinicians should be vigilant for this condition as early recognition of uretero-inguinal hernia is important given the medical and surgical complication it poses.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/33/159448
Financial support and sponsorship: Nil
Conflict of interest: There are no conflict of interest.
REFERENCES
- Chronic obstructive uropathy due to uretero-inguinal hernia: A case report. Int J Surg Case Rep. 2012;3:379-81.
- [Google Scholar]
- Obstructive uropathy secondary to ureteroinguinal herniation. Rev Urol. 2001;3:207-8.
- [Google Scholar]
- Obstructive uropathy due to uretero-inguinal hernia: An uncommon occurrence. Indian J Urol. 2013;29:355-6.
- [Google Scholar]
- Sonographic diagnosis of a ureteral inguinal hernia in a renal transplant. J Ultrasound Med. 2008;27:1759-65.
- [Google Scholar]
- Obstructive uropathy secondary to ureteral herniation in a pediatric en bloc renal graft. Am J Transplant. 2005;5:2074-7.
- [Google Scholar]
- Low-dose versus standard-dose CT protocol in patients with clinically suspected renal colic. AJR Am J Roentgenol. 2007;188:927-33.
- [Google Scholar]
- Does ultra-low-dose CT with a radiation dose equivalent to that of KUB suffice to detect renal and ureteral calculi? J Comput Assist Tomogr. 2006;30:44-50.
- [Google Scholar]






