Translate this page into:
Obliterating Airway Bronchus Sign of Occult Malignancy in Sarcoid Conglomerate Fibrotic Masses

*Corresponding author: Jonathan D. Dodd, Department of Radiology, St Vincent’s University Hospital, Dublin, Ireland. jdodd@svhg.ie
-
Received: ,
Accepted: ,
How to cite this article: McVeigh N, Murphy DJ, McKone E, Dodd JD. Obliterating airway bronchus sign of occult malignancy in sarcoid conglomerate fibrotic masses. J Clin Imaging Sci 2021;11:12.
Abstract
Sarcoidosis is a multiorgan disease which presents in up to 95% of cases with lung involvement, a proportion of which develops conglomerate fibrotic masses (CFMs). CFMs typically progressively increase in size overtime. The development of a lung malignancy within a CFM is rare and difficult to diagnose within the underlying lung fibrosis. Here, we describe the obstructing airway bronchus sign in CFMs as an important part of assessing CFMs overtime on computed tomography, which when it occurs should raise suspicion of an occult underlying carcinoma.
Keywords
Malignancy
Computed tomography thorax
Computed tomography chest
Sarcoidosis
INTRODUCTION
A 62-year-old male presented to the emergency department with increasing fatigue and breathlessness over a week. He suffered from chronic fibrotic pulmonary sarcoid and emphysema for 11 years. He was an exsmoker having stopped when diagnosed with sarcoidosis. Examination revealed extensive wheeze with reduced air entry bilaterally. His spirometry yielded a FEV1 of 1.21 L (32% predicted), FVC 4.85 L (99% predicted), and a diffusing capacity of the lungs for carbon monoxide of 3.24 mmol/(min*kPa) (30% predicted).
Serial chest computed tomography (CT) scans over 10 years showed an interval increase in fibrotic changes in the upper and middle lung zones and perihilar conglomerate fibrotic masses (CFMs) in a typical distribution and appearance for Stage IV chronic fibrotic sarcoid [Figures 1a and b]. Clinically, he reported no change in his baseline dyspnea between 2014 and 2016. Imaging appearances remained stable until 2019 when a repeat chest CT showed an increase in size of the CFMs [Figure 1c]. A PET-CT scan was acquired to assess lung and nodal disease activity because of his worsening dyspnea. It showed no nodal uptake but increased uptake in the right perihilar CFM [Figure 1d]. Subsequent percutaneous CT-guided biopsy revealed squamous cell carcinoma of the lung. Retrospective review of his serial chest CT scans showed obliteration of the airway bronchi within the conglomerate fibrotic mass, caused by the underlying lung carcinoma. He was surgically inoperable due to his severe underlying lung disease and was treated with chemotherapy.
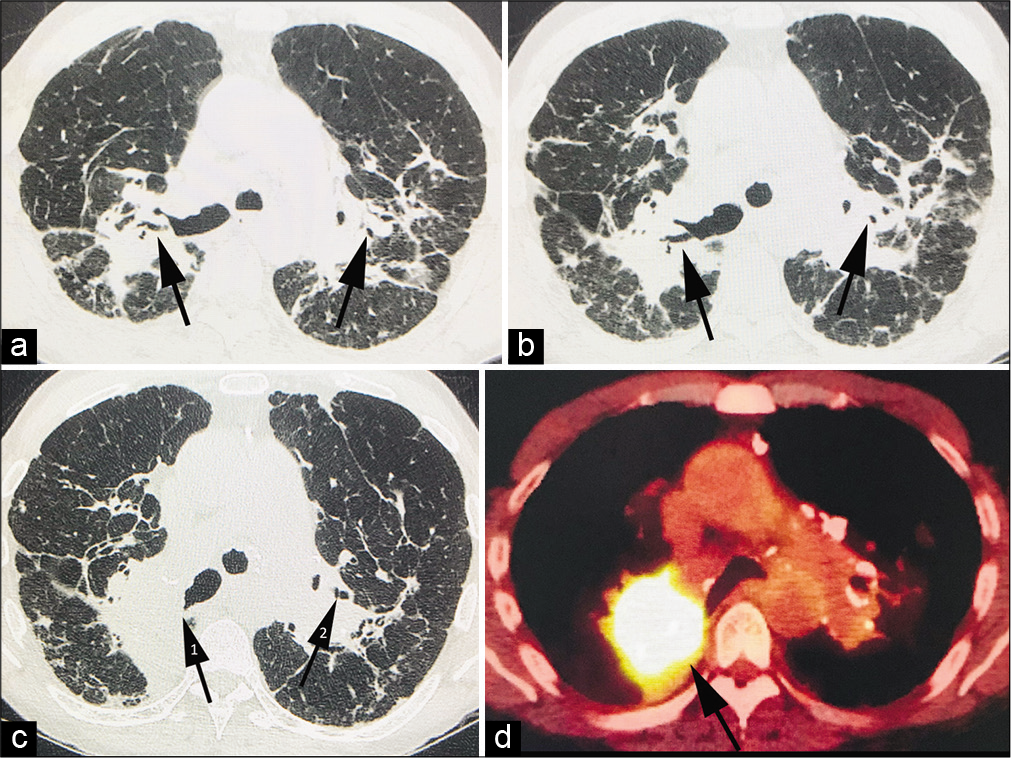
- A 62-year-old male who presented with increasing fatigue and breathlessness on a background history of chronic fibrotic pulmonary sarcoid and emphysema. (a) Non-contrast computed tomography (CT) thorax in 2014 showing bilateral conglomerate fibrotic masses (CFMs) on a background of chronic fibrotic sarcoid. Note the patent airways (arrows) within the masses bilaterally. (b) Non-contrast CT thorax in 2016 showing an interval increase in size of the bilateral CFMs. Again, note patent airways (arrows) with the masses. (c) Non-contrast CT thorax in 2019 shows a marked increase in the size of the right conglomerate fibrotic mass. Note obliteration of the airways (arrow 1) within the right conglomerate mass but patent airways in the left conglomerate fibrotic mass (arrow 2). (d) PET-CT thorax with FDG shows intense FDG uptake within the right conglomerate fibrotic mass (arrow) suspicious for an occult malignancy. Subsequent biopsy revealed squamous cell carcinoma.
DISCUSSION
CFMs are common in fibrotic sarcoid, occurring in 17–20% of cases.[1] They typically show progression in size overtime, making it challenging for radiologists to detect occult malignancy within CFMs. Patients with sarcoid have a slightly higher incidence of solid organ malignancy and immune-related malignancy,[2] with an increased risk of lung malignancy typically presenting during the first 5 years of disease. This is followed by a progressive decrease in risk to 10 years when lung malignancy risk is significantly lower than expected in the general population.[3] As the incidence of concurrent lung malignancy in sarcoidosis is a rare entity, it is often subject to misdiagnosis resulting in a delay in appropriate patient treatment.[4,5]
Many potential causes for obliterating airways can be seen in the lungs, including mucus plugs, aspiration, and pneumonia. Typically, the airways within CFMs are stretched apart by the traction from the surrounding fibrotic process and become dilated, making them easier to detect. Conversely, in malignancy, there is often occlusion or partial occlusion of the airways. The progressively increasing size of benign CFMs on serial CT imaging makes differentiating benign from malignant disease particularly difficult. A further issue is that serial surveillance high-resolution chest CT imaging in sarcoid is typically performed without intravenous contrast, making occult malignancy even harder to detect. We propose that evaluation of CFMs should include an assessment of the airways within these lesions, and an obliterating bronchus should raise the suspicion of an occult malignancy.
CONCLUSION
Imaging interpretation of CFMs should include an assessment of the airways within the masses. The obliterating bronchus sign in CFMs on chest CT should alert the radiologist to the possible diagnosis of an occult lung malignancy.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Long-term follow-up CT scan evaluation in patients with pulmonary sarcoidosis. Chest. 2005;127:185-91.
- [CrossRef] [PubMed] [Google Scholar]
- Sarcoidosis and subsequent cancer risk: A Danish nationwide cohort study. Eur Respir J. 2015;45:269-72.
- [CrossRef] [PubMed] [Google Scholar]
- Sarcoidosis and cancer risk: Systematic review and meta-analysis of observational studies. Chest. 2015;147:778-91.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed diagnosis of lung cancer due to misdiagnosis as worsening of sarcoidosis: A case report. BMC Pulm Med. 2020;20:71.
- [CrossRef] [PubMed] [Google Scholar]
- Concurrence of sarcoidosis and lung cancer. A report of four cases. Respiration. 2000;67:90-3.
- [CrossRef] [PubMed] [Google Scholar]






