Translate this page into:
Non-resolving Findings in a Long-term Radiographic Follow-up of an Infant with Acute Paraffin Oil Aspiration
Address for correspondence: Dr. George Stathis, Department of Radiology, School of Medicine, National and Kapodistrian University of Athens, General University Hospital “ATTIKON”, Rimini 1 Str., Chaidari, GR 124 62, Athens, Greece. E-mail: stathisgrg@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Acute lipoid pneumonia (LP) in children is a rare disorder caused by the aspiration of oil-based substances and is difficult to diagnose due to non-specific clinical symptoms and radiological findings. We report the case of a 5-month-old male infant with acute LP caused by accidental aspiration of a large amount of mineral oil. We present the imaging findings in the computed tomography scans performed during his hospitalization and focus on the residual abnormalities seen on a scan performed 7-years after the incident. This, to the best of our knowledge, is the longest follow-up report of an acute exogenous LP patient and the only case that demonstrates non-resolving abnormalities in a pediatric patient after a single acute episode of mineral oil aspiration.
Keywords
Aspiration
children
lipoid pneumonia
mineral oil
INTRODUCTION

Lipoid pneumonia (LP) is a rare inflammatory disease of the lung parenchyma caused by accumulation of fatty oily material in the alveoli. Exogenous lipoid results from aspiration or inhalation of mineral, vegetable, or animal oil into the peripheral lung.[12] Children can aspirate large amounts of different oily materials, mineral oil being the most frequently encountered substance, and this happens especially when certain risk factors are present.[3456] The aspiration of fatty material elicits a pulmonary inflammatory reaction that produces non-specific clinical and radiologic findings, often similar to those of bacterial pneumonia and tuberculosis, complicating or delaying the diagnosis. Thus, it is imperative to identify correctly this entity when there is a high degree of suspicion, through a thorough and focused noting of patient's medical history and an accurate recognition of its radiologic manifestations. We present a case of acute LP in a 5-month-old infant due to accidental mineral oil aspiration, confirmed by analysis of bronchoalveolar lavage (BAL) and focus on the radiologic findings showing evolution of parenchymal lesions over a follow-up period of 7 years.
CASE REPORT
This was a case report of a 5-month-old male infant who was admitted as an emergency case to a secondary care hospital with acute onset of high-grade fever and respiratory distress. The chest X-ray showed bilateral extensive consolidation involving mainly the lower lobes of the lungs. He was placed on broad spectrum antibiotics and bronchodilatory inhalers, in response to which he showed no clinical improvement over a period of 2 days. Therefore, and in view of his deteriorating clinical status, he was urgently transferred to our hospital for further management.
Upon arrival, the infant was in respiratory distress requiring 4 L/min of oxygen to keep his oxygen saturation above 90%. Further examination of the infant revealed dysmorphic features such as low set ears, generalized muscular hypotony, and delayed psychomotor development. Additional questions on patient history identified that at the age of 5-months the child had accidentally ingested paraffin oil administered by his 3-year-old brother. This prompted consideration of a probable diagnosis of acute exogenous LP. Computed tomography (CT) scan [Figure 1a] revealed extensive bilateral consolidations in the lower lobes. Bronchoscopy was performed which did not reveal any significant anatomical abnormalities or foreign bodies. The BAL aspirate was opalescent with a supernatant halo of fat and showed an increased number of macrophages. BAL was sent for microbiological studies including Gram staining, Ziehl-Neelsen staining, and bacterial and fungal cultures. The microbiological results were all negative. The cytologic study showed numerous foamy macrophages with intracytoplasmic and extracellular droplets of fat with a positive histochemical confirmation of acute LP with Oil Red O stain. (Oil Red O is a fat-soluble dye used for staining of lipids and triglycerides.) Total lavage was not performed as it was considered too risky in view of the critical status of the patient and the signs of hypoxia he demonstrated during the procedure.
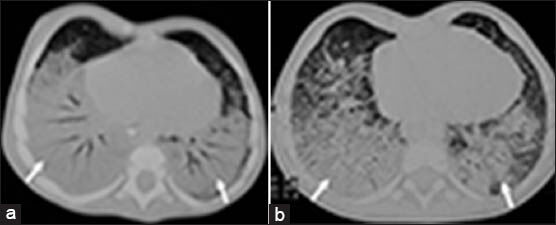
- 5-month-old male infant aspirated large amounts of paraffin oil causing respiratory distress diagnosed later as due to lipoid pneumonia (a) Chest computed tomography (CT) performed 1.5 month post-paraffin oil aspiration shows diffuse extensive airspace consolidations (arrows) in both lower lobes. (b) High-resolution chest CT taken 7 months after the incident shows persistent imaging findings (arrows) with minimal improvement.
A corticosteroid therapy regimen was introduced which led to an improvement of his general condition. The infant remained in our hospital for a total of 5 months showing gradual clinical improvement. Before discharge an additional bronchoscopy and BAL was performed that showed a clear aspirate with no supernatant fat and fewer lipid-laden macrophages. Further, an additional CT scan was performed which showed persistent findings with minimal improvement [Figure 1b]. 7-years after the incident, the patient was admitted for a complete workup. He underwent spirometry, which revealed a forced vital capacity (FVC) equal to 85% of predicted value, a forced expiratory volume in 1 s (FEV1) of 79% of predicted value. FVC and FEVI values over 80% of predicted value are considered normal. FEV1/FVC ratio was 81%, which was within the normal range (approximate range: 75-80%) for healthy adults. The reversibility test was negative. The patient could not undergo further pulmonary function testing (lung volume, diffusing capacity of lung for carbon monoxide). BAL revealed far fewer lipid-laden macrophages, while the CT scan showed resolution of the consolidations, but evidence of residual interstitial findings [Figure 2].

- 8-year-old male with history of acute lipoid pneumonia. Follow-up high-resolution chest computed tomography taken 7-years after the episode of aspiration, shows bilateral thickening of the interlobular septa (open arrow), streaky peripheral infiltrates (arrows) and areas of hyperinflation.
DISCUSSION
LP is an uncommon pulmonary disorder that results from the accumulation of lipids in the alveoli.[12] On the basis of the source of the lipid, it is further classified as exogenous or endogenous. The exogenous type is due to aspiration of animal fat, vegetable or mineral oil and can be acute or chronic in presentation.
Acute exogenous LP is a type of pneumonitis associated with an incident of aspiration of a large amount of an oil-based product.[1] Most cases of exogenous LP result from aspiration of mineral oil, which is usually used for the treatment of refractory constipation.[1] In early childhood, the factors that increase the risk of aspiration, in both the acute and chronic form, are commonly associated with underlying conditions, such as disruption of the normal physiologic function of the airway and the upper gastrointestinal tract, congenital disorders of the structure and function of the foregut, and impairment of neurologic or neuromuscular control of the process of breathing and/or swallowing. Additional predisposing factors to LP in children are gastroesophageal reflux and forced ingestion of oily medication as practiced in a number of geographic areas.[35] Our patient showed features of developmental delay along with generalized muscular hypotony, which was hypothesized to have contributed to the aspiration of a large amount of material.
Acute exogenous LP in children, typically manifests clinically as an acute aspiration condition, which evolves into respiratory failure and, occasionally, death.[7] In the report published by Zanetti et al., 17 children with LP having non-specific clinical presentation, showed air space consolidation on chest radiographs, which suggested bacterial pneumonia.[4] The children showed no improvement with antibiotic therapy and were later investigated with high-resolution CT and BAL. Only at this stage did the parents mention the history of mineral oil ingestion. The time period between the initial radiographs and diagnosis varied from 30 days to 45 days. Such a delay was also observed in our case, partially attributed to the initial reluctance of the parents to mention the incident of accidental aspiration, afraid of being accused of lack of proper care of the baby.
Acute exogenous LP manifests radiologically within 30 min of the episode of aspiration or inhalation. Pulmonary opacities can be seen in most patients within 24 h.[2] Chest X-ray shows parenchymal abnormalities that include areas of ground-glass opacity or consolidation, bilateral and segmental or lobar in distribution and predominantly involving the middle and lower lobes, similar to those seen in general aspiration pneumonia. High-resolution computed tomography is the imaging technique of choice for investigating LP and, in children, it must be performed with the lowest possible radiation. The principal CT imaging findings include alveolar consolidations, ground-glass opacities, nodular lesions, interlobular septal thickening, and intralobular interstitial thickening.[34] The crazy-paving pattern, consistent with well-defined areas of ground-glass attenuation with superimposed septal thickening, has also been described as a characteristic feature of LP. In addition, exogenous LP may be diagnosed promptly when areas of fat attenuation are identified within a pulmonary air-space consolidation. Pure mineral oil has a CT attenuation value of -132 HU and negative density values (between -30 and -150 HU) within the consolidation area. These findings, although non-specific, can suggest the diagnosis of LP.[12] However, in some patients with LP, as in the present case, fat attenuation is not evident on CT images because the fat attenuation values are averaged with the surrounding inflammatory exudates so that the fat component becomes less conspicuous or obscure.[1]
According to most studies on pediatric patients, the radiologic manifestations of acute exogenous LP typically improve or resolve over time. Sias et al.,[5] evaluated 28 children with LP for 24 months and demonstrated normalization of CT scans in 18 of them right after treatment. In two patients scanned 12 months after treatment, a cystic lesion in the right lung and a discrete area of segmented atelectasia were observed. Treatment abandonment occurred in 6 cases and no further CT follow-up was reported for the remaining children. Sias et al., also demonstrated the potential role of multiple BALs in the treatment of LP, in a prospective study of 10 children with LP. In these cases, LP was secondary to mineral oil aspiration, and the delay between aspiration and treatment was 1-60 days.[8] Over a follow-up period of 6 months, complete radiologic resolution was demonstrated in 3 out of 6 patients who had a short interval between intake of mineral oil (1-4 days) and treatment. In the remaining three cases, partial resolution with patchy residual ground glass opacities were seen on CT. All four children with a longer time interval between aspiration of mineral oil and treatment had residual areas of consolidations on CT scans taken at 6-months, but no further follow-up was reported.
In our case, the follow-up CT scan that was performed 7 years after the aspiration demonstrated architectural distortion associated with thickening of the interlobular septa. Mineral oil (a mixture of inert, long-chain, saturated hydrocarbons obtained from petroleum) is emulsified and phagocytosed by alveolar macrophages, which, filled with oil, reach the interlobular septum through the lymphatic channels. Subsequently, with the permanence of the oil, there is development of chronic interstitial inflammation, which can evolve into pulmonary fibrosis and decreased lung volume. In our case, there was no evidence of end-stage lung lesions and functional respiratory tests were normal. The imaging findings can be attributed to the large amount of aspirated oil, the delay in the correct diagnosis and the fact that the patient did not undergo any therapeutic BAL, which has been shown to facilitate the removal of lipid-laden macrophages implicated in development of alveolar and interstitial fibrosis. To the best of our knowledge, this is the longest follow-up study of a pediatric patient with acute LP showing imaging features on CT and the only case reported where a single episode of fat aspiration that is associated with residual interstitial changes in the follow-up CT scan.
CONCLUSION
We have described a case of acute exogenous LP induced by accidental aspiration of mineral oil for which the early imaging findings were consistent with published reports. Long-term follow-up, however, revealed partial resolution with persistent interstitial lesions seen on CT scan. A finding that has not been reported in the pediatric population and merits consideration when interpreting imaging examinations of patients with a history of acute LP.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/2/126028
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Radiological and clinical findings in acute and chronic exogenous lipoid pneumonia. J Thorac Imaging. 2003;18:217-24.
- [Google Scholar]
- Lipoid pneumonia: Spectrum of clinical and radiologic manifestations. AJR Am J Roentgenol. 2010;194:103-9.
- [Google Scholar]
- Lipoid pneumonia in children: Clinical and imagenological manifestations. Arch Med Res. 2000;31:42-7.
- [Google Scholar]
- Lipoid pneumonia in children following aspiration of mineral oil used in the treatment of constipation: High-resolution CT findings in 17 patients. Pediatr Radiol. 2007;37:1135-9.
- [Google Scholar]
- Evolution of exogenous lipoid pneumonia in children: Clinical aspects, radiological aspects and the role of bronchoalveolar lavage. J Bras Pneumol. 2009;35:839-45.
- [Google Scholar]
- Lipoid pneumonia in 53 patients after aspiration of mineral oil: Comparison of high-resolution computed tomography findings in adults and children. J Comput Assist Tomogr. 2010;34:9-12.
- [Google Scholar]
- Radiographic plain film and CT findings in lipoid pneumonia in infants following aspiration of mineral oil used in the treatment of partial small bowel obstruction by Ascaris lumbricoides. Pediatr Radiol. 1985;15:157-60.
- [Google Scholar]
- Clinic and radiological improvement of lipoid pneumonia with multiple bronchoalveolar lavages. Pediatr Pulmonol. 2009;44:309-15.
- [Google Scholar]






