Mandibular Metastasis of a Recurrent Poorly Differentiated Urothelial Bladder Carcinoma

*Corresponding author: Georges Aoun, Department of Oral Medicine and Maxillofacial Radiology, Faculty of Dental Medicine, Lebanese University, Beirut, Lebanon. aoungeorges@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Aoun G, Hayek E, Nasseh I. Mandibular Metastasis of a Recurrent Poorly Differentiated Urothelial Bladder Carcinoma. J Clin Imaging Sci 2020;10:27.
Abstract
Metastatic lesions to the oral cavity are uncommon; they represent between 1 and 3% of all malignant oral neoplasms. In this article, we report a rare case of metastatic urothelial bladder carcinoma in the mandible detected on oral radiographic images and confirmed with multiple imaging modalities. A 67-year-old woman presented to our clinic suffering from pain in the right side of the mandible with a mild swelling. Panoramic radiograph revealed an ill-defined relatively radiolucent lesion in the right mandibular premolar-canine region presenting with permeative changes. Cone-beam computed tomography showed a relatively hypodense lesion with demineralization, interruption of the buccal cortices, and slight thickening and sclerosis of the buccal cortical bone. The patient was referred for further evaluation including additional advanced imaging radiographic techniques (MRI and PET scan) and clinical and histopathological examinations that lead to a final diagnosis of metastatic lesion from an underlying urothelial bladder carcinoma.
Keywords
Bladder
Carcinoma
Mandible
Metastasis
Urothelial
INTRODUCTION
Metastatic tumors to the oral cavity are uncommon and are generally detected at a late stage of the disease.[1,2] They are usually found in the jaws and less frequently in the surrounding soft tissues and salivary glands.[1-3]
Tumors metastasizing to the oral cavity mostly come from the breast, the lung, the adrenal glands, the kidneys, the bone, the colon, and the prostate.[3]
Clinically, metastatic tumors of the oral cavity may be asymptomatic or present different non- pathognomonic symptoms mimicking odontogenic infections such as numbness or paresthesia of the lower lip and chin, pain, swelling, altered sensation, halitosis, gum irritation, teeth loosening and mobility, soft-tissues exophytic masses, trismus, and rarely pathologic fractures.[3-8]
Radiographically, these malignant lesions do not present a specific radiographic appearance; radiolucent with ill-defined margins, radiopaque, or mixed radiopaque-radiolucent lesions may be seen.[4,9] This variety of imaging features makes their diagnosis challenging, especially in the initial stages of the disease.
The majority of patients presenting oral metastatic tumors have invasive disease with a poor prognosis.[10,11]
In the literature, few cases of bladder cancer metastatic to the oral cavity have been reported. This report describes a case of a mandibular metastasis of a poorly differentiated urothelial carcinoma.
CASE REPORT
A 67-year-old female presented to our clinic with subtle vague pain in the right premolar region of the mandible, severely mobile adjacent teeth and paresthesia of the right lower lip and chin. The symptoms were perceived about 3–4 weeks previously.
The patient smoked not less than 20 cigarettes/day and her medical history revealed a surgery 12 years previously for a low-grade papillary urothelial carcinoma with complete recovery; no other specific health conditions or any systemic medications taken regularly were reported.
Extraoral examination did not show any abnormality while intraorally a slight swelling of the right lower buccal premolar region was noticed. The overlying mucosa was normal in color but softly tender on palpation.
The adjacent teeth were abnormally loose with the presence of deep pockets and calculus deposits reflecting a severe chronic periodontitis. No regional lymphadenopathy was detected.
A periapical radiograph of the concerned region revealed an ill-defined and non-corticated relatively low-density area with permeative changes, the adjacent teeth were removed, but the symptoms persisted after 2 weeks even though the bone healing was normal. The periapical radiograph taken after extraction exhibited an increased radiolucency in the area [Figure 1].

- Periapical radiographs (before and after extraction) of a 67-year-old woman with subtle vague pain in the right premolar region of the mandible and a paresthesia of the right lower lip and chin revealing an ill-defined radiolucency and alveolar bone demineralization (arrows).
The orthopantomograph showed a 2 cm diameter ill-defined and non-corticated slightly radiolucent osteolytic lesion with permeative changes of the right premolar region extending from the canine area to approximately the mesial aspect of the molar area, the lesion also appeared to be extending from the apical area within the alveolar crest to the superior aspect of the basal cortex [Figure 2].
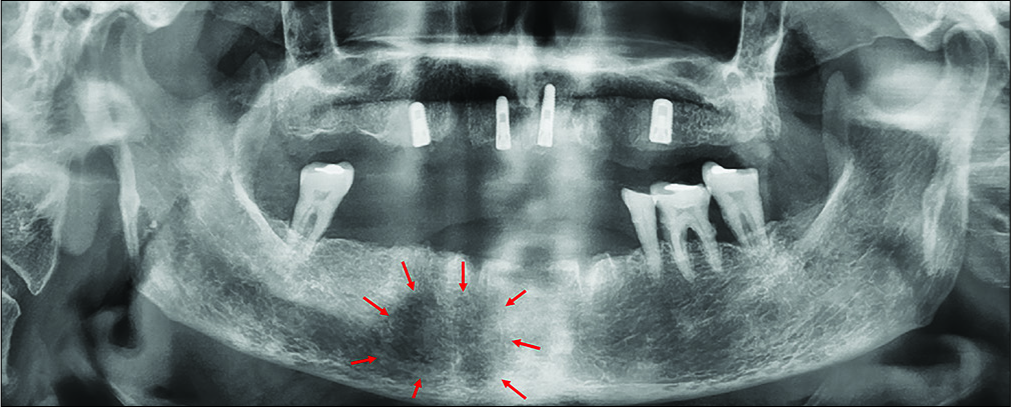
- Panoramic radiograph (after extraction) of a 67-year-old woman with subtle vague pain in the right premolar region of the mandible and a paresthesia of the right lower lip and chin showing the ill-defined radiolucent spongeous osteolytic lesion of the right premolar region in the mental foramen area (arrows).
Cone-beam computed tomography (CBCT) serial cross- sectional of 1 mm thick showed small ill-defined hypodense areas in proximity to the right lower premolar with multiple perforations of the buccal and lingual plates and slight thickening and sclerosis of the buccal cortex [Figure 3].
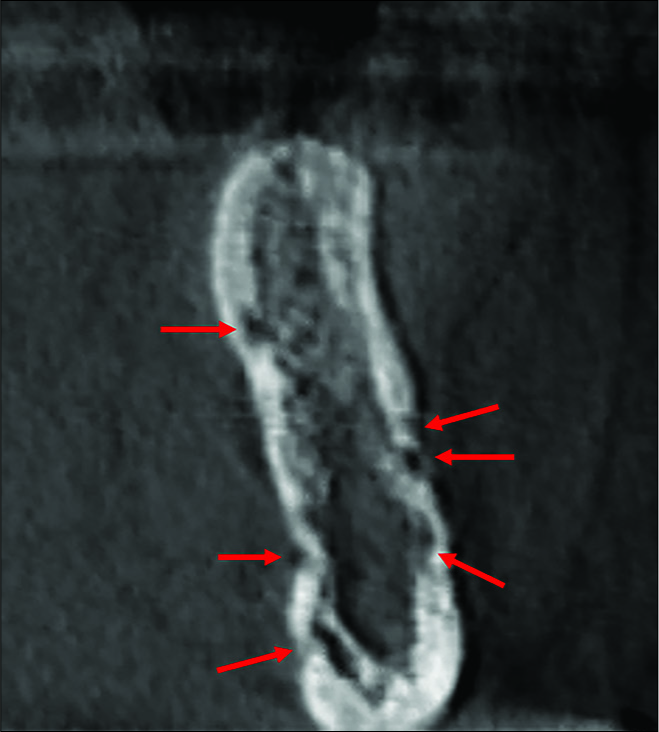
- Cone-beam computed tomography cross-sectional 1 mm thick of a 67-year-old woman with subtle vague pain in the right premolar region of the mandible and a paresthesia of the right lower lip and chin showing multiple perforation of the buccal and lingual plate area near the right lower premolar (arrows).
The same radiographic features are seen in the axial, sagittal, and frontal views [Figure 4].
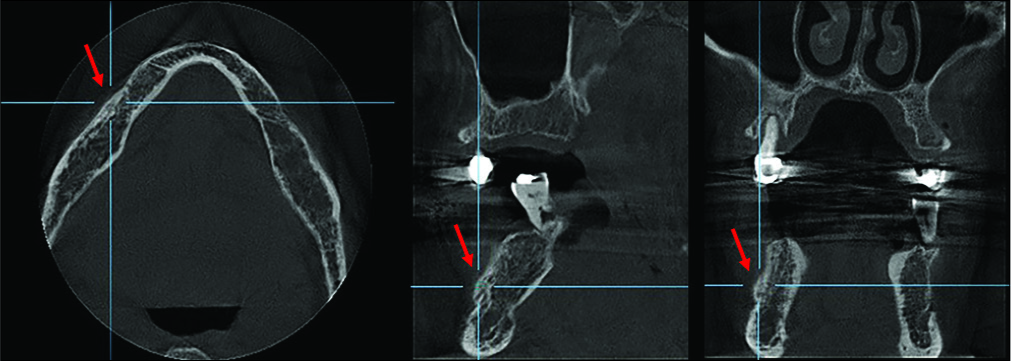
- Axial, sagittal, and frontal cuts at the level of the right lower premolar area of a 67-year-old woman with subtle vague pain in the right premolar region of the mandible and a paresthesia of the right lower lip and chin showing a slight expansion of the buccal cortex (arrows).
Radiographic features and changes as well as the clinical findings were highly suggestive of an aggressive/malignant process.
The patient was referred for maxillofacial surgery evaluation. An incisional biopsy was performed under local anesthesia and sent for histological assessment.
The anatomopathological examination showed bone and fibrous tissues infiltrated by poorly differentiated carcinomatous proliferation. In immunohistochemistry, tumor cells expressed high-molecular-weight cytokeratin; CK7 expressions were intense and diffuse, while GATA3 presented a moderate to low intensity and was distributed heterogeneously.
These findings support the diagnosis of a poorly differentiated metastatic carcinoma.
The patient was referred to an oncologist and a whole body assessment was performed by means of positron emission tomography (PET) scans after intravenous injection of 11 mCi of 18F-FDG and high-resolution CT scan using dedicated PET scanner [Figure 5]; a large hyperactive area involving the right mandible was detected.
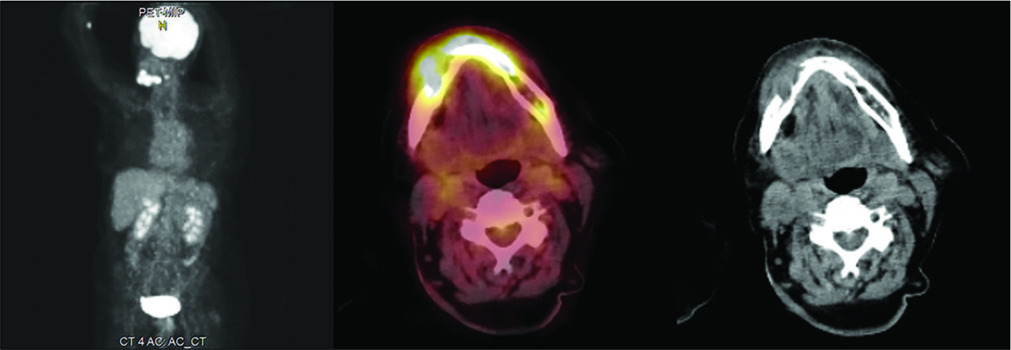
- A 67-year-old woman whole body PET scan and high- resolution PET-CT after intravenous injection of 11 mCi of 18F-FDG showing large hyperactive area involving the right mandible.
Head-and-neck MRI-3T examination showed lytic lesion of the right anterior mandibular body measuring 3 cm and abnormal signal involving also the left mandibular side, suspicious for tumoral infiltration [Figure 6].
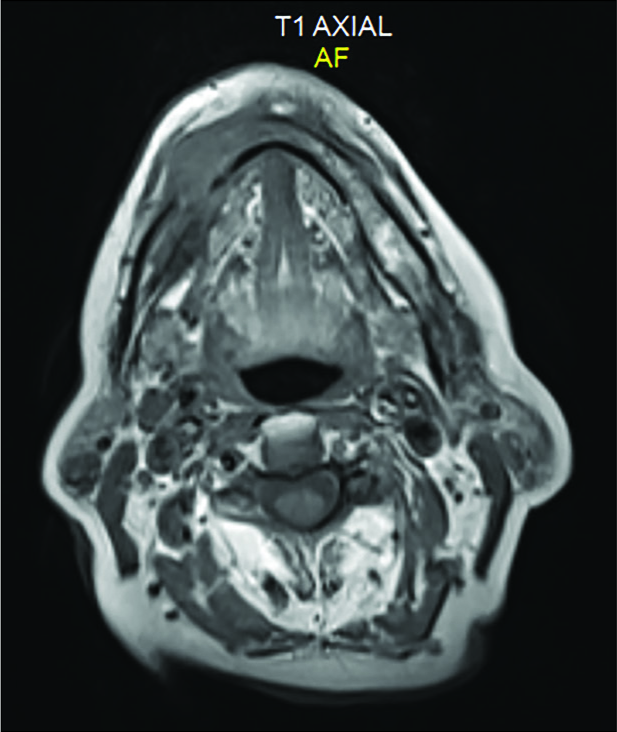
- A 67-year-old woman MRI-3T showing lytic lesion of the right anterior mandibular body measuring 3 cm and abnormal signal involving also the left mandibular side, suspicious for tumoral infiltration.
Other diagnostic procedures were requested such as a pelvic ultrasound and a bladder biopsy.
These investigations confirmed a papillary urothelial carcinoma (Grade 2, Jewett Stage B) infiltrating the muscle wall of the bladder.
The histopathological aspects as well as the immunohistochemical profile are more or less compatible with what was found at the level of the mandibular tumor, which argues in favor of the mandibular metastasis of the urothelial carcinoma.
Extraction of the involved teeth before treatment was decided and the patient was referred for chemo- and radiotherapy. Radiation with a cumulative dose over 2 weeks resulted to a complete relief of her symptoms; every 2 weeks follow- up examinations were performed for the first 2 months and twice per month for the 2 next years.
DISCUSSION
Metastatic tumors to the oral cavity are rare;[12,13] they represent between 1 and 3% of all malignant oral neoplasms and are more frequently found in the jaws.[1-3] Among the jawbones, the mandible is more affected by metastases than the maxilla, with the areas distal to the canine (including the ramus and the body of the mandible) being the most commonly involved.[3,4]
The pathogenesis of mandibular metastasis is not completely understood; however, it is supposed to be hematogenous connected with Batson venous plexus and the presence of abrupt vessel angulation, especially in the molar and premolar regions, leading to bloodstream slowing and favoring the deposit of malignant cells.[14]
Urothelial carcinoma is the most frequent malignant tumor occurring in the bladder; with a slight male predilection, it attacks generally the patients in their 6th and 7th decades.[13]
Mandibular metastasis of bladder urothelial carcinoma is exceptional. In their study conducted on 107 patients, Barbaian et al. found that metastasis from this tumor concerns mostly the regional lymph nodes, the liver, the lungs, the bones, and the adrenal glands.[15]
Because of the infrequency of metastatic bladder tumors to the mandible and the lack of typical clinical signs and radiological features linked to them, their diagnosis is challenging; establishing a precise diagnosis the soonest is essential because these lesions represent a poor prognosis sign of the disease and their early detection is of extreme importance.[12,13]
Finally, metastatic lesions should always be considered in the differential diagnosis of ill-defined jawbones radiolucencies, particularly in patients with a history of malignancy.
CONCLUSION
In the presence of atypical clinical signs and uncharacteristic radiological features in the oral cavity, dentists should take into consideration the probable existence of oral metastases of undiscovered distant primary lesions, especially in patients with a history of previous malignant disease even with complete recovery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Distant metastases and malignant cellular neoplasms encountered in the oral and maxillofacial region: Analysis of 92 patients treated at a single institution. Anticancer Res. 2010;30:1843-8.
- [Google Scholar]
- Metastatic tumours to the oral region. An overview. Eur J Cancer B Oral Oncol. 1995;31:355-60.
- [CrossRef] [Google Scholar]
- Metastases to the oral mucosa: Analysis of 157 cases. J Oral Pathol Med. 1993;22:385-90.
- [CrossRef] [PubMed] [Google Scholar]
- Metastatic tumors in the jaws: A retrospective study of 114 cases. J Am Dent Assoc. 2006;137:1667-72.
- [CrossRef] [PubMed] [Google Scholar]
- Numb chin syndrome: An ominous clinical sign. Br Dent J. 2010;208:283-5.
- [CrossRef] [PubMed] [Google Scholar]
- Mandibular pain as the leading clinical symptom for metastatic disease: Nine cases and review of the literature. Ann Oncol. 1998;9:559-64.
- [CrossRef] [PubMed] [Google Scholar]
- Numb chin syndrome secondary to metastatic breast disease. J Colo Dent Assoc. 1999;78:11-4.
- [Google Scholar]
- Metastatic tumors to the jawbones: Analysis of 390 cases. J Oral Pathol Med. 1994;23:337-41.
- [CrossRef] [PubMed] [Google Scholar]
- Neoplasms metastatic to the mouth, jaws and surrounding tissues. J Craniomaxillofac Surg. 1989;17:283-90.
- [CrossRef] [Google Scholar]
- Transitional cell carcinoma of the urinary bladder metastatic to the oral mucosa. Oncol Lett. 2012;3:343-5.
- [CrossRef] [PubMed] [Google Scholar]
- Carcinoma of the urinary bladder metastatic to the oral cavity. Indian J Cancer. 1994;31:8-11.
- [Google Scholar]
- Maxillary metastasis of transitional cell carcinoma: Report of a case. Oral Surg Oral Med Oral Pathol. 1989;67:185-9.
- [CrossRef] [Google Scholar]
- Mandibular metastasis in a patient with pulmonary adenocarcinoma. Dentomaxillofac Radiol. 2006;35:383-5.
- [CrossRef] [PubMed] [Google Scholar]
- Metastases from transitional cell carcinoma of urinary bladder. Urology. 1980;16:142-4.
- [CrossRef] [Google Scholar]






