Translate this page into:
Malpositioned Lines and Tubes on Chest Radiograph – A Concise Pictorial Review

*Corresponding author: Muthu Kumar Sakthivel, Department of Radiology, Division of Cardiothoracic Imaging, University of North Carolina, North Carolina, United States. drmuthukumar1985@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sakthivel MK, Bosemani T, Bacchus L, Pamuklar E. Malpositioned Lines and Tubes on Chest Radiograph – A Concise Pictorial Review. J Clin Imaging Sci 2020;10:66.
Abstract
A wide variety of cardiothoracic support devices are used in intensive care units and few of these devices are increasingly being utilized in outpatient settings as well. A meticulous assessment of these lines and tubes by the interpreting radiologist is cardinal since malpositioned lines and tubes can significantly impact the functioning of these devices and may result in potential complications affecting the clinical outcomes. The purpose of this article is to illustrate the normal positioning and malpositioning of the routinely used support lines and tubes identified on chest radiographs.
Keywords
Endotracheal tube
Enteric tube
Central venous catheters
Chest radiograph
INTRODUCTION
Chest radiograph is the most performed radiographic examination because of the simplicity in the technique and its clinical utility in both inpatient and outpatient settings. Due to the complexity of the critically ill patients in intensive care units, the performance of daily routine radiographs has been in practice for decades. According to a recent American College of Radiology appropriateness criteria, there is no specific necessity to obtain daily routine chest radiographs.[1,2] However, radiographs are recommended whenever there is a significant change in clinical status, placement and repositioning of support devices, and after any bedside procedures.
ENDOTRACHEAL TUBE
A diverse variety of endotracheal tubes is in clinical practice. The parts of the ET tube include an inflatable cuff that will safely secure the trachea to avert air leak and decrease the risk of aspiration.
Positioning of endotracheal tube: Always start with ensuring the ET tube is within the tracheal air column. The normal positioning of the endotracheal tube is always referred to as the distance of the ET tube tip from the carina. The normal position of the carina is at the level of T4-T5 which is used as the landmark for ET tube positioning. Preferably, the ET tube is positioned in the mid-thoracic trachea terminating 3–5 cm from above the carina. Accounting for flexion and extension of neck, a 2 cm ascend or descend from the aforementioned measurements is commonly encountered.
Malpositioned ET tube
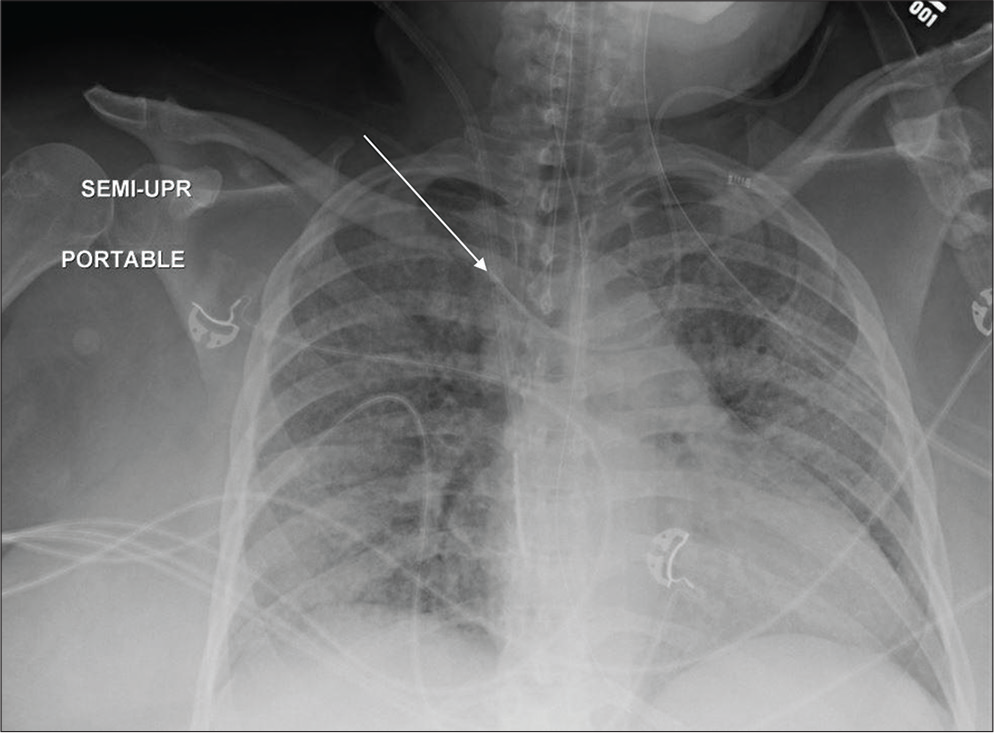
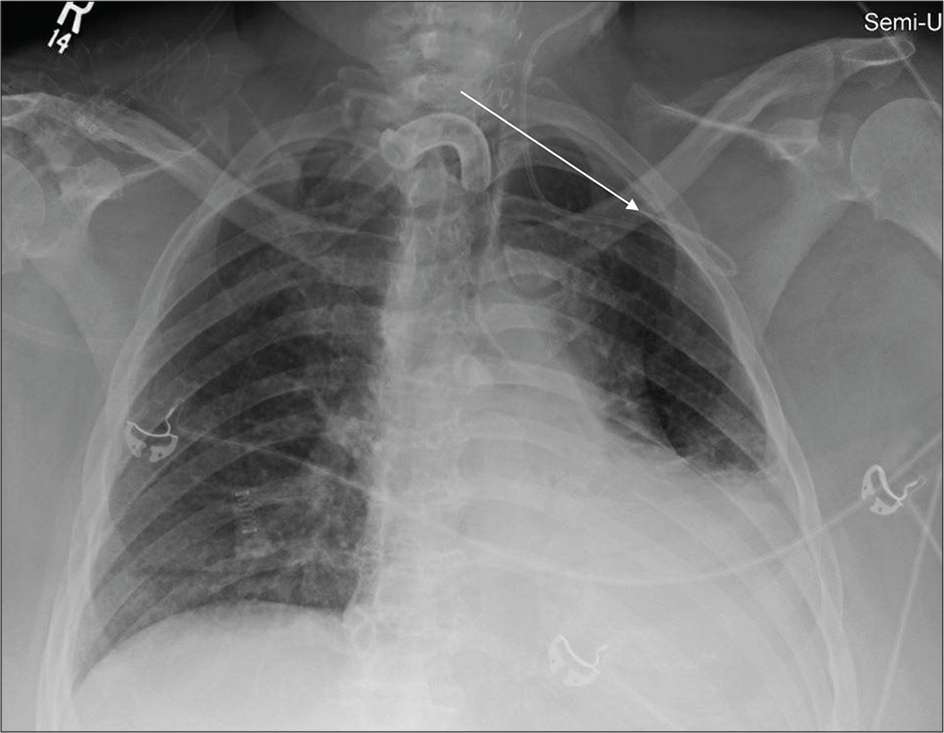
Advancement of ET tube inferiorly into the bronchus may result in hyperinflation of the intubated lung and collapse of the contralateral lung. When the ET tube is advanced too far into the right main stem bronchus, the tube will descend into bronchus intermedius and result in the right upper lobe collapse [Figures 1a and b, Figures 2 a and b]. In the case of esophageal intubation, the ET tube lies left lateral to the tracheal walls within a distended esophagus. A lateral or oblique radiograph will be helpful in precisely delineating this malposition.
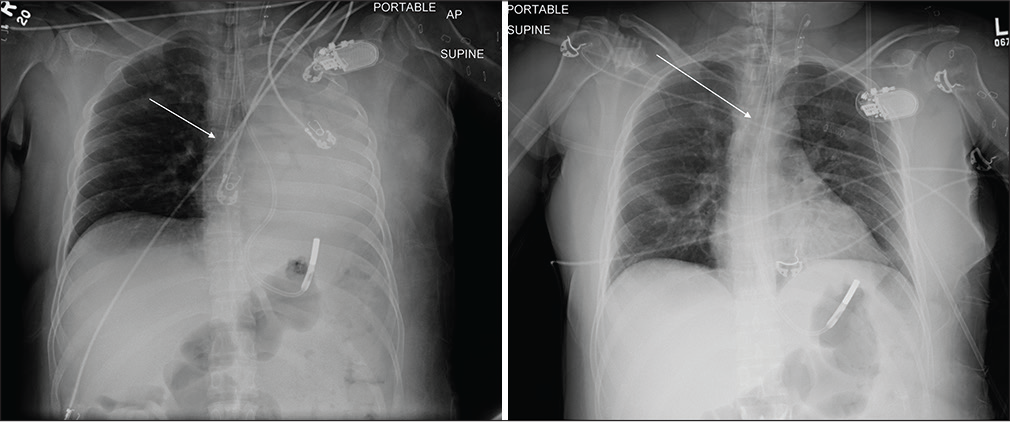
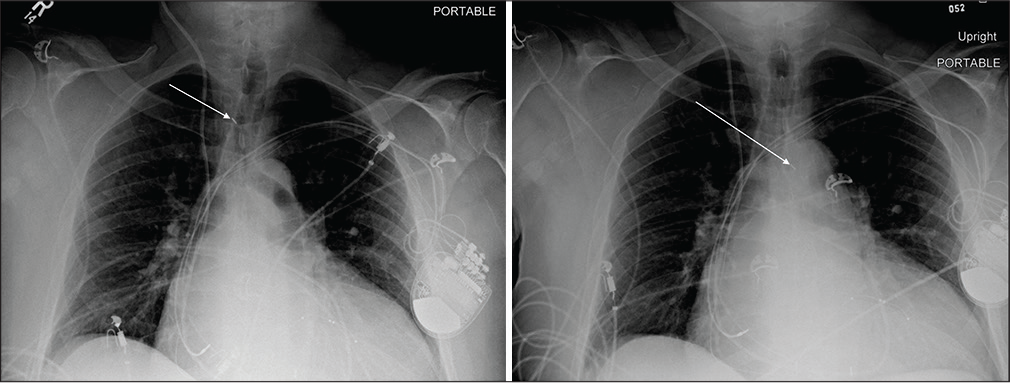
- A 55-year-old male with nephrotic syndrome developed dyspnea. (a) Portable chest radiograph reveals right main stem bronchus intubation (white arrow) with associated complete collapse of the left lung. (b) Repeat portable chest radiograph after repositioning the endotracheal tube with its tip now terminating 3 cm above the carina (white arrow) and resultant reexpansion of the left lung.
- A 54-year-old male admitted in the ICU following a fire accident. (a) Portable chest radiograph reveals left main stem bronchus intubation (white arrow) with bilateral perihilar opacities suggestive of inhalational pneumonitis. (b) Repeat portable chest radiograph after repositioning the endotracheal tip now terminating 2.7 cm above the carina (white arrow).
Key point
Tip of ET tube should be positioned 3–5 cm from the carina. Always check the position of head of the patient as it can alter the position of ET tube, with the ET tube moving inward toward the carinal on flexion and moving away from the carina on extension.
TRACHEOSTOMY TUBE
There is a wide range of tracheostomy tubes available with different materials, size, and styles. Most tubes have a main shaft (cannula) attached to a neck plate (flange), and cuffed tubes have a pilot balloon, which shows whether the cuff is inflated.
Position of tracheostomy tube: Always look for tracheostomy cannula projecting within the tracheal air column.
Malpositioned tracheostomy tube
It is relatively rare to malposition a tracheostomy tube as compared to the endotracheal tube since they are fixed in position by sutures. When there is suspicion for a malpositioned tracheostomy tube,always check the patient’s position since patient rotation can lead to apparent appearance of tracheostomy tube being malpositioned outside the tracheal air column.
Key point
The tracheostomy cannula should project over the tracheal column.
ENTERIC TUBE
In clinical practice, both weighted and non-weighted enteric tubes are routinely used for feeding and decompression of the stomach respectively. Weighted tubes can be identified by its radiodense tip on a radiograph.
Positioning of enteric tubes
The side port of an enteric tube should be ideally positioned below the gastroesophageal junction for proper functioning and to avoid the potential risk of aspiration.
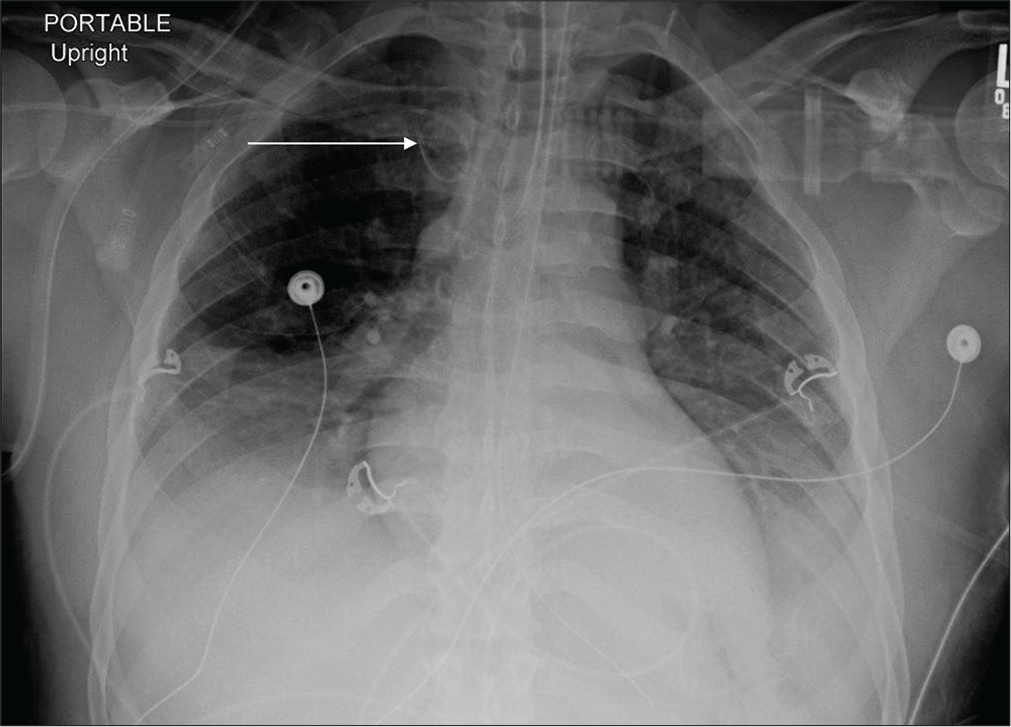
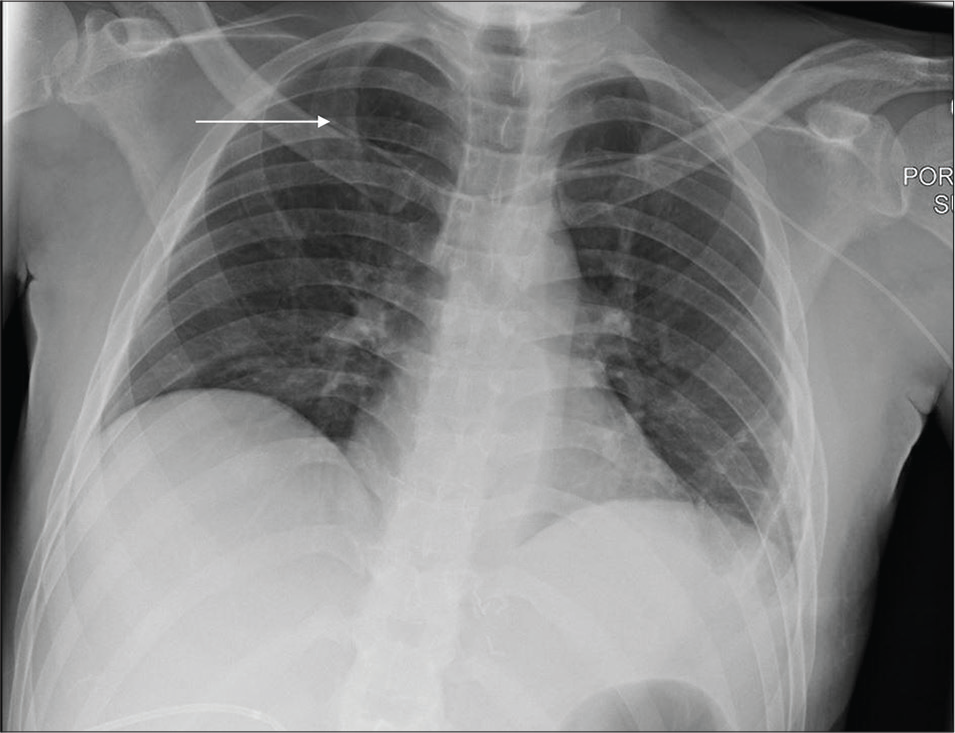
Malpositioning of enteric tubes
An enteric tube terminating above the diaphragm should be meticulously evaluated for malpositioning, which includes tracheal placement, inadequate positioning, and coiling of enteric tubes within the esophagus [Figures 3-5].
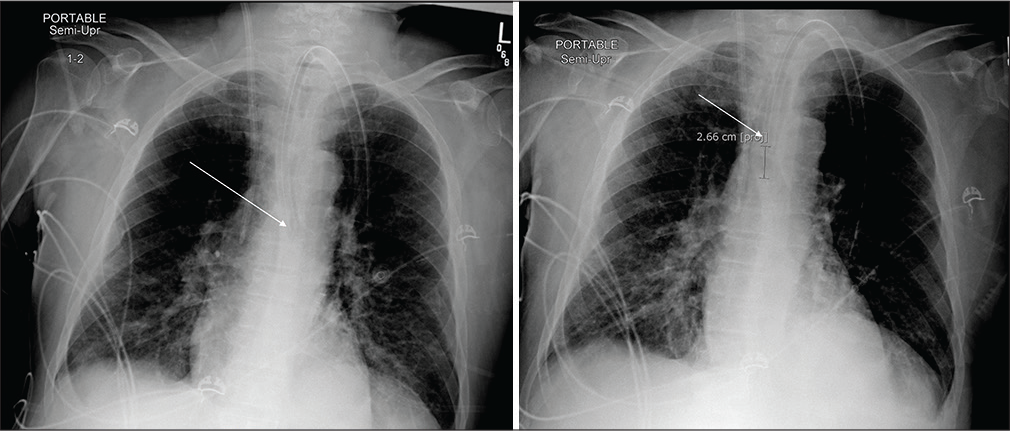
- A 45-year-old female admitted in ICU post-cholecystectomy. (a) Portable chest radiograph reveals coiling of non-weighted enteric tube in neck (white arrow). (b) Repeat portable chest radiograph after repositioning the enteric tube which now courses through the diaphragm with tip beyond the field of view (white arrow) and mid background pulmonary edema.
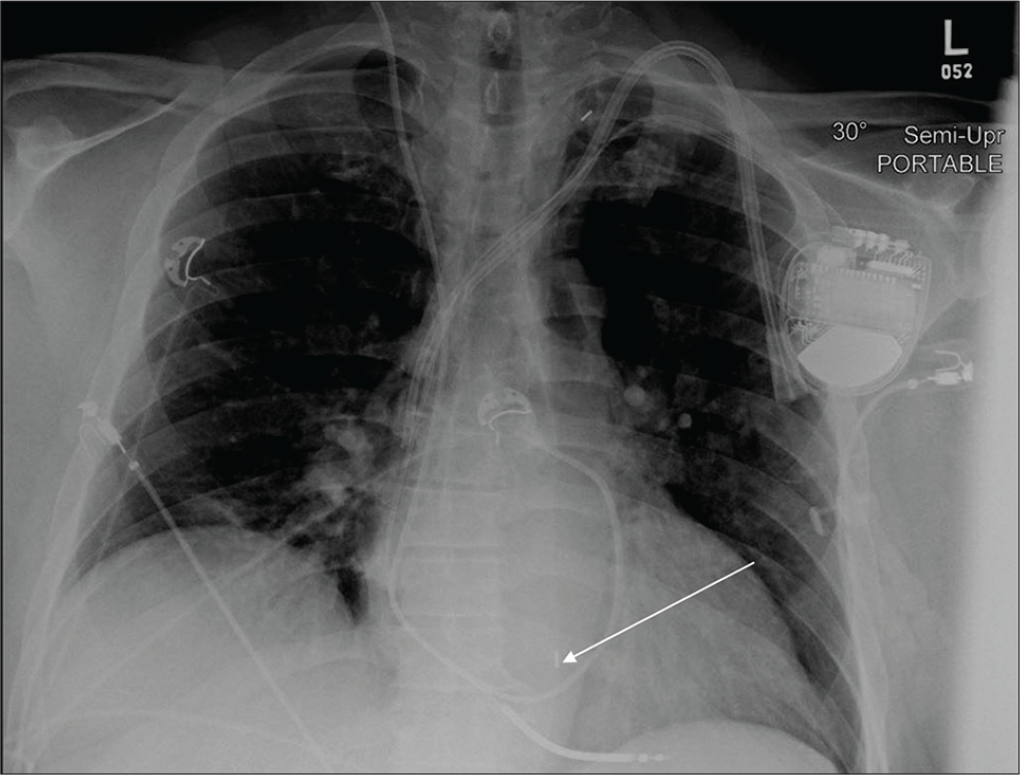
- A 43-year-old male post-thymic resection admitted in the ICU. Portable chest radiograph reveals moderate right pleural effusion with adjacent atelectasis, tracheostomy, and appropriately positioned bilateral central venous catheters. The weighted enteric tube coursing into the left main stem bronchus (white arrow).
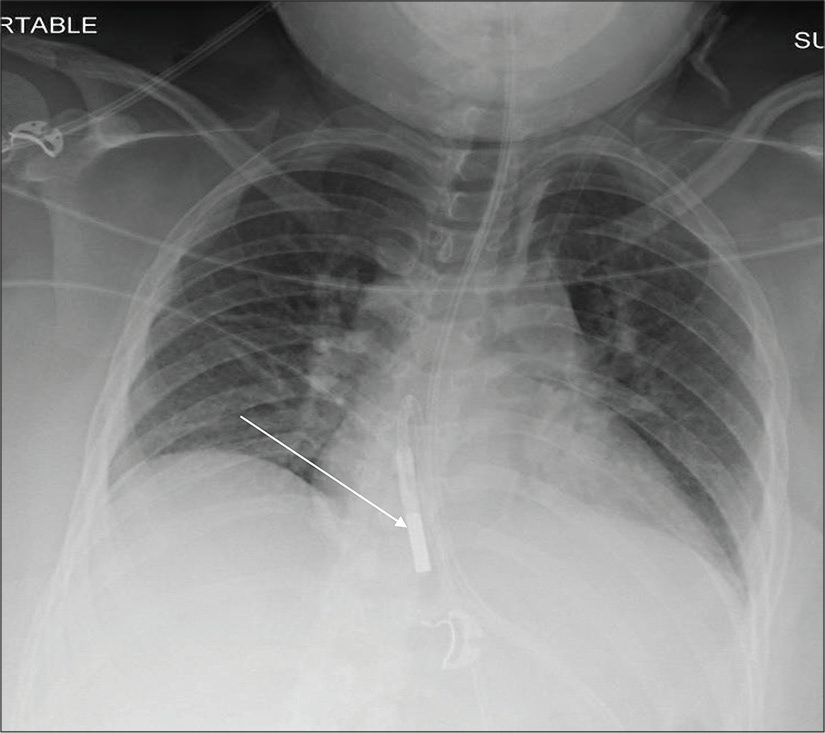
- A 28-year-old male post-appendectomy admitted in ICU. Portable chest radiograph demonstrates hypoinflated lungs with bibasilar atelectasis and coiling of weighted enteric tube within the mid-thoracic esophagus (white arrow).
Key point
The side port of an enteric tube should be ideally positioned below the gastroesophageal junction.
ESOPHAGEAL TEMPERATURE PROBE
Esophageal temperature probes are routinely used for the monitoring of core body temperature in critically ill patients.
Positioning of temperature probes: Ideal placement at the level T8-T9 intervertebral space has long been considered essential for accurate measurement. Chest radiographs are done to ensure correct positioning.
Malpositioned temperature probes
The most commonly encountered malposition is the temperature probe tip at the neck or proximal thoracic esophagus [Figure 6].
- A 45-year-old female post-kidney transplant admitted in ICU. Portable chest radiograph reveals left retrocardiac atelectasis and coiling of esophageal temperature probe with its tip in the proximal thoracic esophagus (white arrow). Other support devices are appropriately positioned.
Key point
The esophageal temperature probe tip should project over level of T8-9.
CENTRAL VENOUS CATHETERS
There have been dramatic advancements in the image-guided placement of central venous catheters which enable appropriate and precise positioning. Central venous catheters can be categorized into four different groups; the peripherally inserted central catheter is non-tunneled central venous catheters, tunneled central venous catheters, peripherally inserted catheters, and implantable port catheters.[3]
Positioning of central venous catheters
Ideally, cavoatrial junction is at commonly acceptable landmark signifying appropriate positioning. Radiographically, this landmark is defined by the right tracheobronchial angle and carina. Cavoatrial junction typically resides 3–4 cm below the structures, however, there is a great variability in apparent positioning taking into account of lung inflation, patient positioning, and projection of the radiographs.
Malpositioning and other complications of central venous catheters
The interpreting radiologist should perform a meticulous assessment of the course of the central venous catheter and also assess for abnormal course, coiling, kinking, fragmentation, and catheter pinch-off. Central venous catheters placed with tip terminating higher from the cavoatrial junction are prone to have low flow rates, malfunction, and thrombosis. There is also a higher risk of SVC erosion, especially with the left-sided catheter insertion. However, with the lower tip, there is a higher risk for arrhythmia. Central venous catheters that taking a vertical course and terminating toward the left of the spine indicate the presence of left-sided SVC, double SVC, coursing into the internal mammary vein, arterial placement, or maybe extravascular [Figures 8-13].
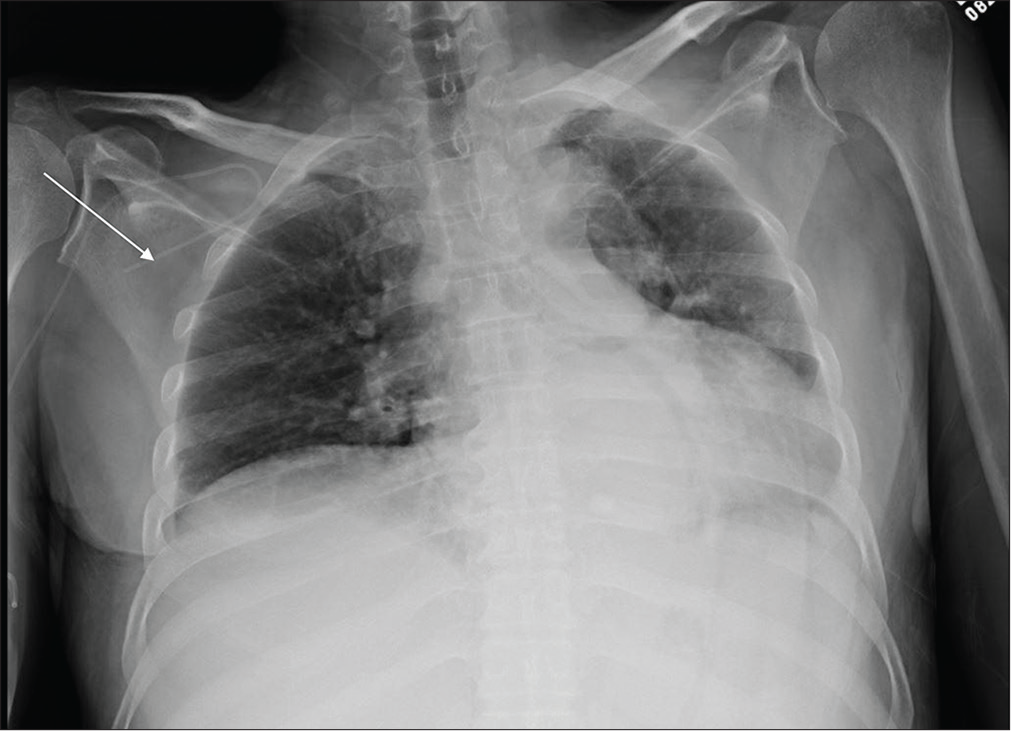
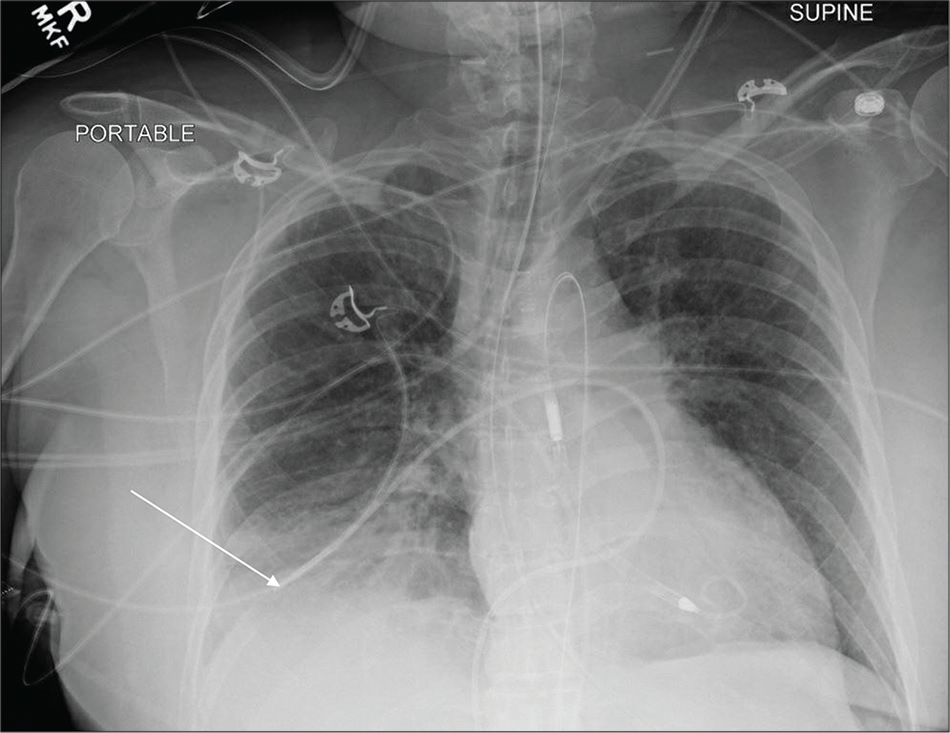
- A 44-year-old male with renal failure admitted in ICU. Portable chest radiograph reveals hypoinflated lungs left retrocardiac atelectasis and coiling of the right subclavian approach central venous catheter and terminating in the right axillary artery (white arrow).
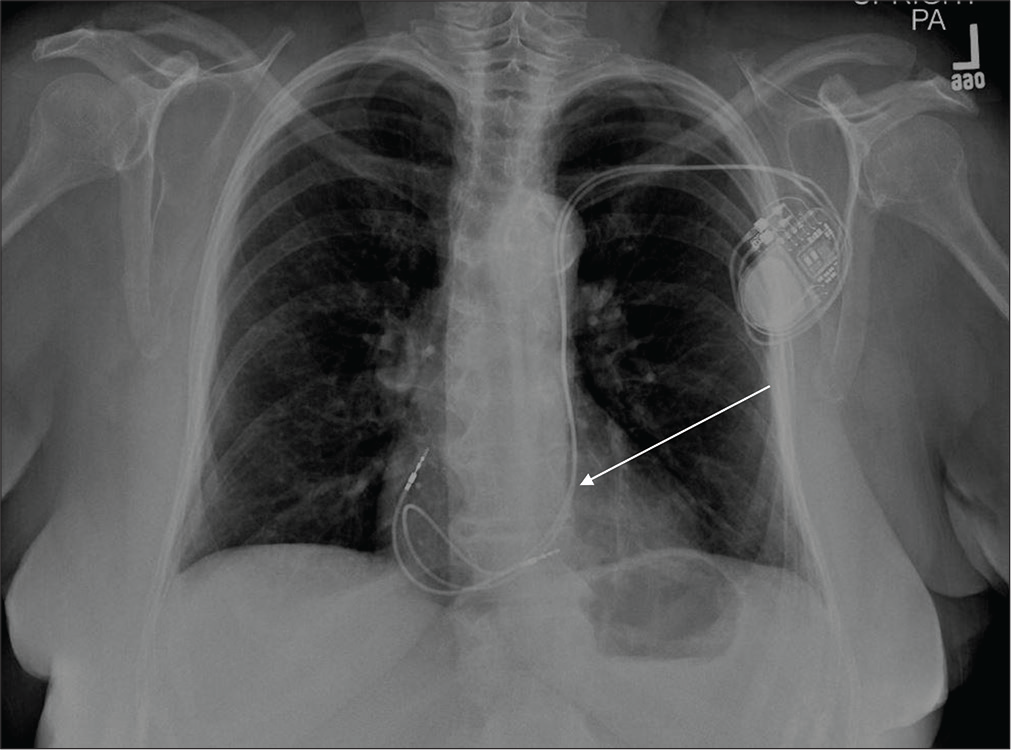
- A 54-year-old female with ruptured splenic abscess admitted in the ICU. Portable chest radiograph reveals small left pleural effusion with the left basilar atelectasis and anomalous course of the left subclavian approach central venous catheter into right ventricle (white arrow). This patient had a left-sided SVC (normal variant).
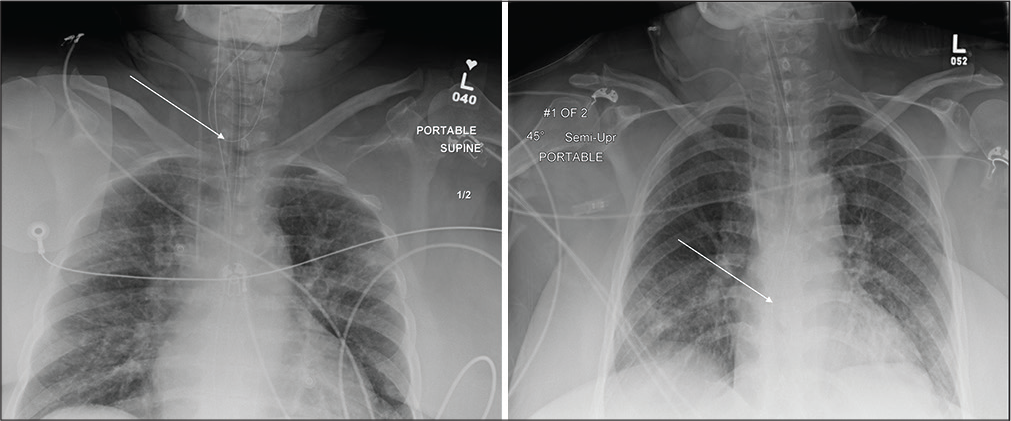
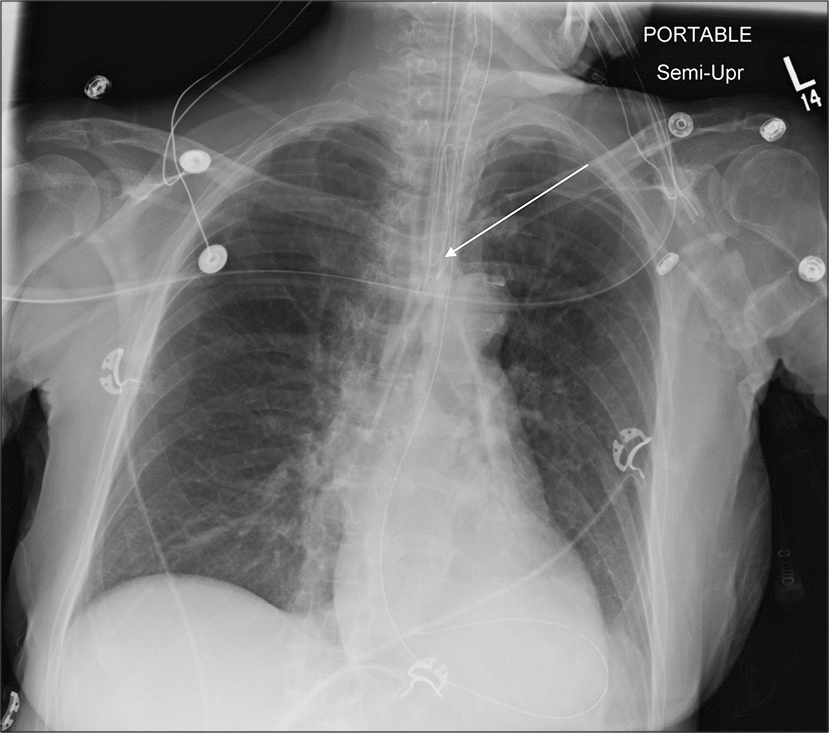
- A 54-year-old male with congestive heart failure admitted in ICU. Portable chest radiograph reveals pulmonary edema and malpositioned left IJV approach central venous catheter with its tip terminating in the distal right brachiocephalic vein (white arrow). Other support devices are appropriately positioned.
- A 56-year-old male with laryngeal carcinoma admitted in ICU. Portable chest radiograph reveals tracheostomy tube within the tracheal air column, malpositioned left IJV approach central venous catheter coursing through and coiled within the left subclavian vein (white arrow), left pleural effusion, and adjacent atelectasis.
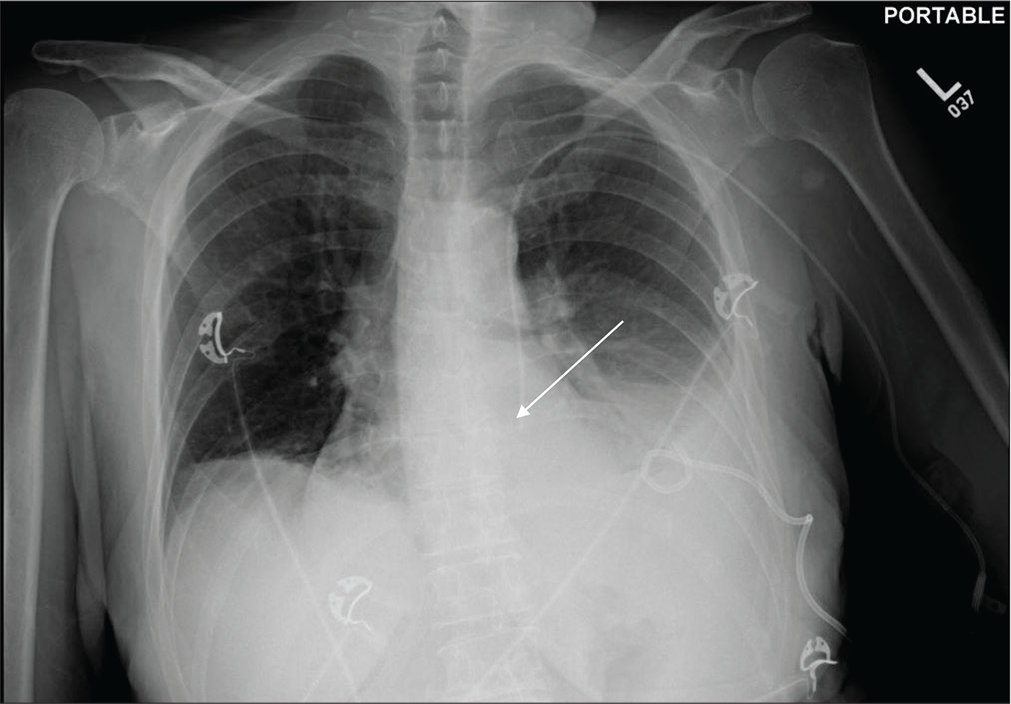
- A 66-year-old male with pancreatic adenocarcinoma post Whipple’s procedure admitted in ICU. Portable chest radiograph reveals small bilateral pleural effusions and bibasilar and left retrocardiac atelectasis and coiling of the right subclavian approach central venous catheter in the proximal right brachiocephalic vein (white arrow). Other support devices are appropriately positioned.
- A 36-year-old male with the right renal malignancy post-surgical resection admitted in ICU. Portable chest radiograph reveals malpositioned left subclavian approach central venous catheter with the tip in the right subclavian vein (white arrow).
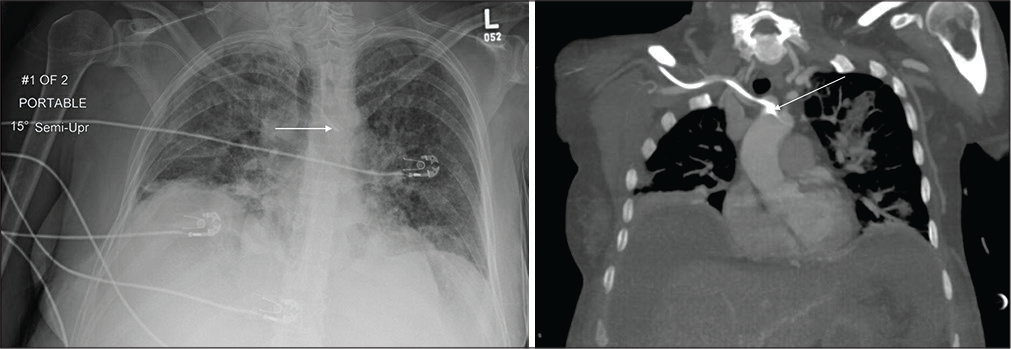
- A 46-year-old male with acute septic shock admitted in ICU. (a) Portable chest radiograph demonstrates malpositioned right subclavian approach central venous catheter crossing the midline and terminating at the expected location of aortic arch (white arrow). A central venous catheter crossing the midline should raise the suspicion of arterial placement. There are diffuse heterogeneous airspace opacities bilaterally suggestive of multifocal pneumonia. (b) Coronal chest CT MIP images of the same patient confirm arterial placement of the right central venous catheter (white arrow) and scattered multifocal opacities suggestive of multifocal pneumonia.
Key point
Tip of central venous catheter should terminate at the cavoatrial junction.
PULMONARY ARTERIAL CATHETER
Swan-Ganz catheters are typically inserted for monitoring pulmonary arterial branch pressures but also used for delivery of medications such as thrombolytic infusions.
Positioning of the Swan-Ganz catheter
Preferentially, the Swan-Ganz catheter tip should terminate centrally within the right or left main pulmonary artery, ideally proximal to the interlobar pulmonary artery.
Malpositioning and complications of Swan-Ganz catheter
If the catheter tip is too distal, it may result in pulmonary infarction or pulmonary hemorrhage, which may be seen as peripheral wedge-shaped peripheral consolidation distal to the catheter. Catheter looping in the right heart made resulting in valvular damage or arrhythmia.
Key point
Swan-Ganz catheter should never cross the hilum [Figures 14-16].
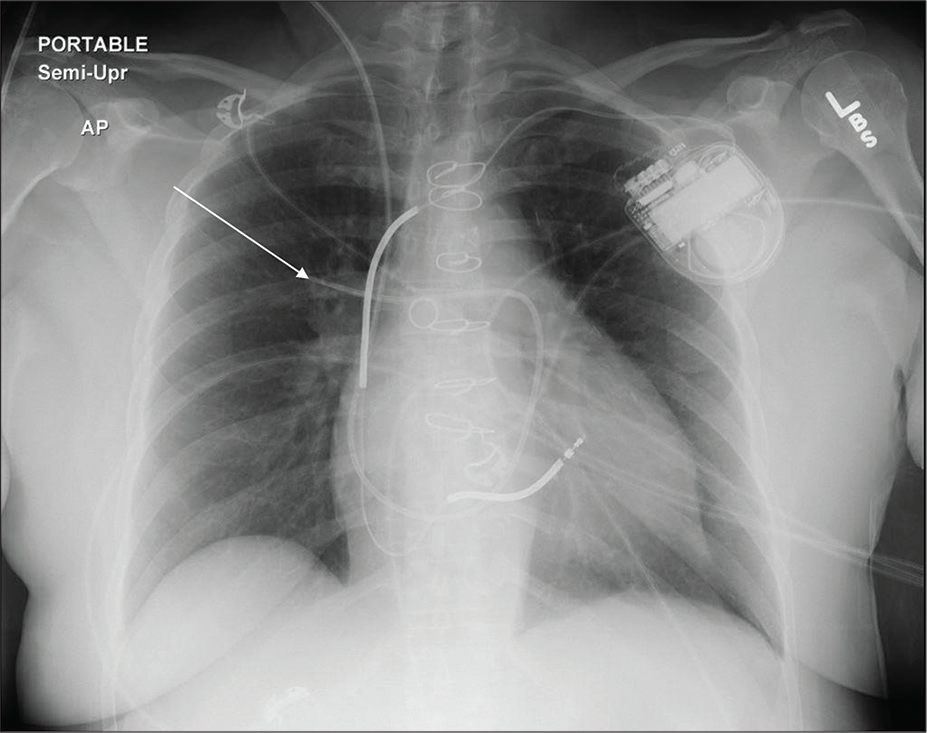
- A 46-year-old female post-CABG admitted in cardiac ICU. Portable chest radiograph demonstrates right IJV approach catheter terminating in the right lower lobe segmental branch pulmonary artery (white arrow). Other support devices are appropriately positioned.
- A 59-year-old female with ventricular tachyarrhythmia and cardiac arrest admitted in cardiac ICU. Portable chest radiograph demonstrates right femoral (inferior) approach Swan-Ganz catheter terminating in the right lower lobe segmental branch pulmonary artery (white arrow). Other support devices are appropriately positioned.
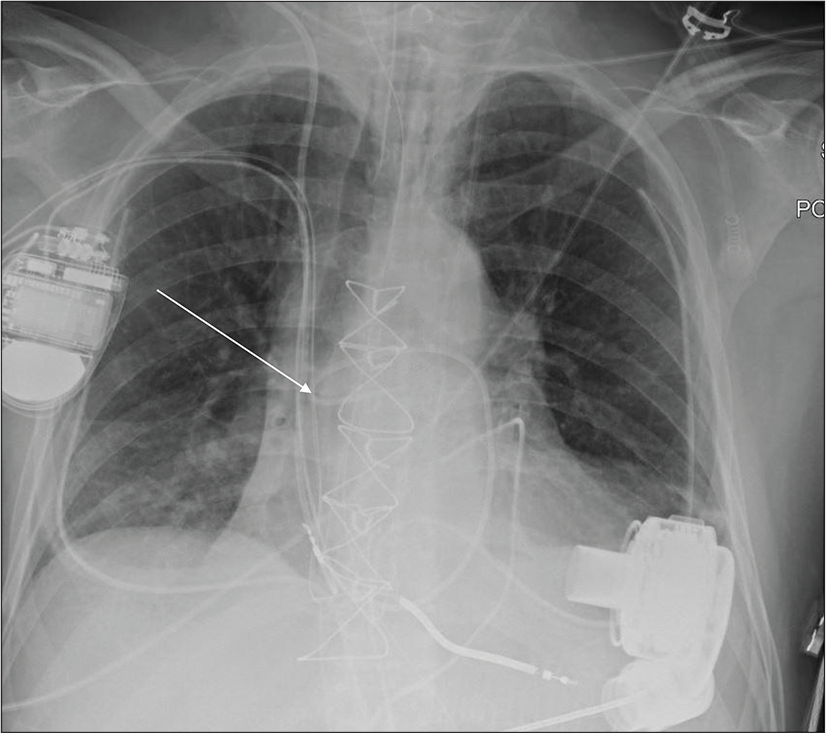
- A 61-year-old male with cardiac failure and post-LVAD placement admitted in cardiac ICU. Portable chest radiograph demonstrates right IJV approach Swan-Ganz catheter coiled within the mid-right pulmonary artery (white arrow). Other support devices are appropriately positioned.
INTRA-AORTIC BALLOON PUMP
IABP catheter is used to improve coronary blood flow during diastole in patients with myocardial ischemia. The interpreting radiologist should be aware of the way IABP is introduced whether it is through the femoral or subclavian arterial approach. This is important to assess for malpositioning and to guide further the tip should be repositioned proximally or distally.
Positioning of IABP
The IABP tip is identified by a radiopaque marker. The tip should be positioned in the proximal descending thoracic aorta, just below (i.e., 2.0 cm) the left subclavian artery take-off and superior contour of the transverse aorta.
Malpositioning of IABP
IABP catheters with their tips placed too proximally can impede the cerebral blood flow and cause stroke [Figure 17]. IABP catheters with their tips placed too distally can result in suboptimal myocardial profusion and potential renal ischemia [Figure 18].
- A 52-year-old male with ischemic cardiomyopathy admitted in cardiac ICU. Portable chest radiograph demonstrates right axillary approach IABP with its proximal tip at the expected location of the right innominate artery (white arrow). The distal tip of IABP is not in the field of view. In this scenario, the radiologist should recommend advancement of the IABP catheter. Other support devices are appropriately positioned. (b) Repeat chest radiograph of the same patient demonstrates interval advancement of the right axillary approach IABP with proximal tip projecting over the proximal aortic arch (white arrow) and distal tip projecting over the descending thoracic aorta.
- A 62-year-old male with thyroid malignancy and coronary atherosclerosis admitted in cardiac ICU post-myocardial infarction. Portable chest radiograph demonstrates femoral approach IABP with its distal tip lying very low 9 cm from the superior aspect of aortic arch (white arrow). The proximal tip is not visualized in the field of view. In this scenario, the radiologist should recommend advancement of the femoral approach IABP catheter.
Key point
IABP tip should lie 2 cm inferior to the aortic arch. Always check for femoral versus axillary/subclavian artery approach insertion of IABP [Figure 17 and 18].
CARDIAC CONDUCTION DEVICES
Cardiac conduction devices are used in clinical practice for more than 6 decades. The most commonly used cardiac conduction devices are pacemaker and implantable cardioverter-defibrillator. These devices have three main parts; pulse generator, electrodes, and lead wires. The radiologist should check all of these parts and look for abnormalities in the course, coiling, and fracture.
Positioning of the cardiac conduction devices
The most commonly utilized insertion approach is by the percutaneous transvenous technique where the leads are inserted via the left subclavian vein for the right atrial access. The generator is placed in the subcutaneous pocket.
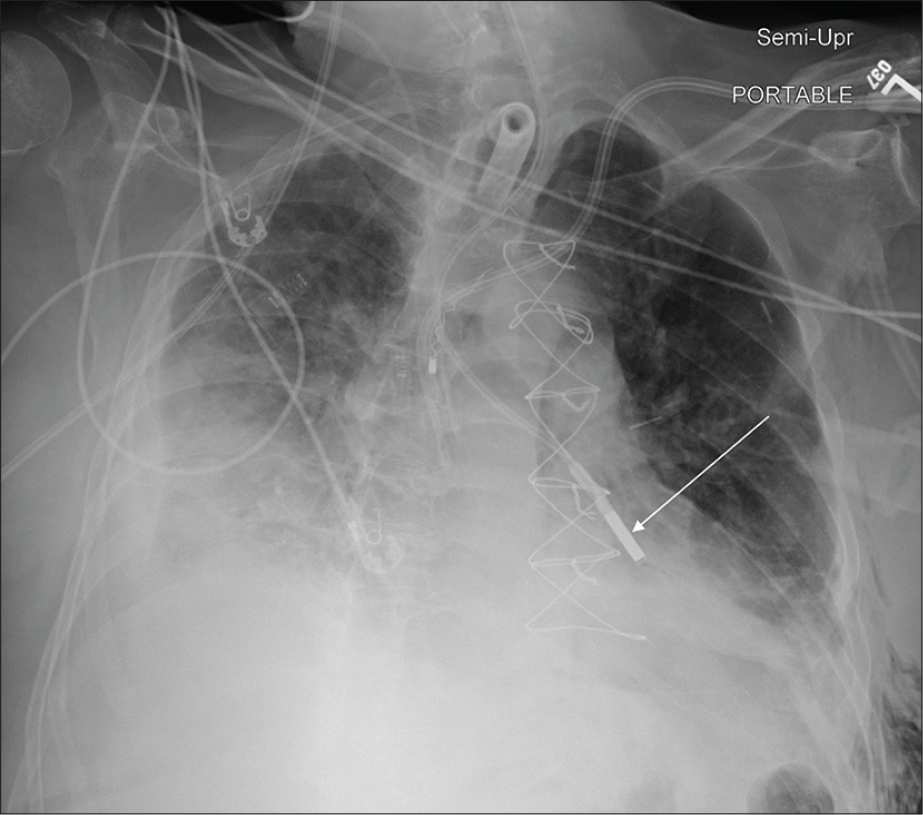
Malfunctioning/malpositioning of the cardiac conduction devices: The interpreting radiologist should look for kinking, pinching, and fracturing of the leads [Figure 19]. An extremely rare condition pacemaker-twiddler’s syndrome refers to permanent malfunction of a pacemaker which occurs when the patient manipulates the subcutaneous chest device resulting in retraction of the previously well-positioned AICD/pacer leads. The interpreting radiologist should also be watchful for the course of the pacemaker/AICD leads since rarely there may be presence of left-sided SVC which makes the implantation of cardiac pacing lead into the right ventricle particularly difficult. This occurs due to the ostium of coronary sinus not being in alignment with the tricuspid orifice and hence a loop must be made before the lead can pass through the tricuspid valve [Figure 20].[4] In routine clinical practice, the radiologist will come across abandoned AICD/pacer leads which were intentionally left. These abandoned catheters rarely cause complications.
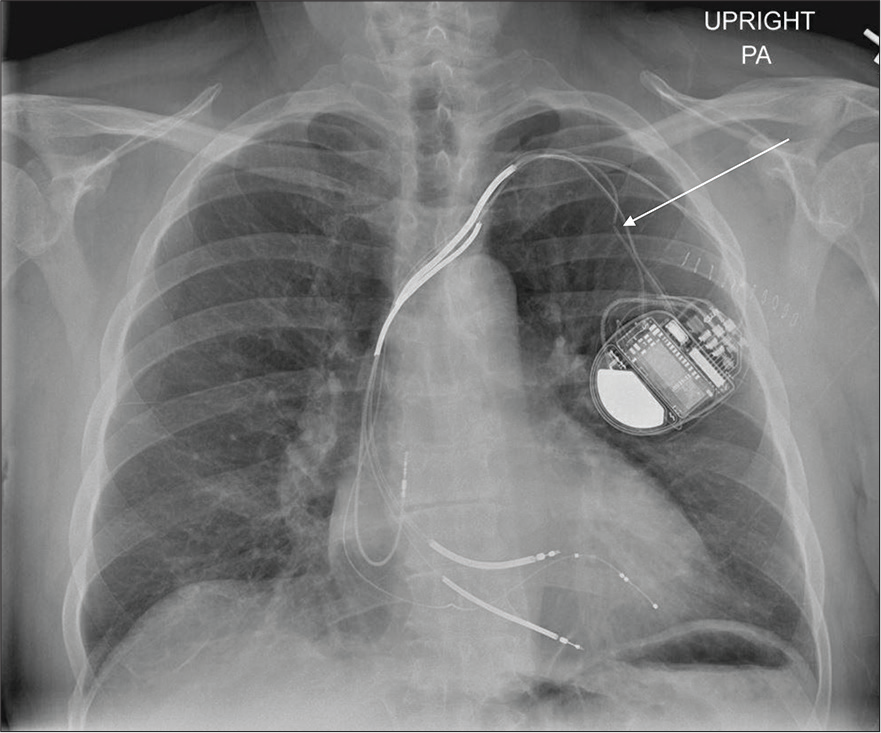
- A 55-year-old male with a medical history of arrhythmia and treated with biventricular defibrillator presented to the cardiology outpatient clinic with worsening palpitations for the past 1 week. PA chest radiograph demonstrates fracture of one of the pacemakers/AICD leads (white arrow).
- A 59-year-old female with new-onset arrhythmia underwent chest radiograph post-pacemaker placement. PA chest radiograph demonstrates left chest wall AICD with anomalous course of pacemaker lead through left-sided SVC with the leads in the right atrium and right ventricle (white arrow).
Key point
A pneumothorax should be excluded on the immediate post-insertion chest radiograph.
CONCLUSION
Chest radiograph is routinely used to assess the appropriate positioning of support devices. An increased awareness of normal and incorrect positions of support devices on chest radiographs can prevent the development of adverse events.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Identification of malpositioned tubes and lines in ICU patients: An automated solution utilizing the electronic medical record. J Am Coll Radiol. 2013;10:146-8.
- [CrossRef] [PubMed] [Google Scholar]
- Chest radiography in the ICU: Part 2, evaluation of cardiovascular lines and other devices. AJR Am J Roentgenol. 2012;198:572-81.
- [CrossRef] [Google Scholar]
- Detection of a left superior vena cava during a pacemaker implantation in Cotonou. Case Rep Cardiol. 2017;2017:7634082.
- [CrossRef] [PubMed] [Google Scholar]






