Translate this page into:
Magnetic resonance permeability for the evaluation of head and neck tumors: Parotid and beyond

*Corresponding author: Stephanie Yuka Matwijszyn Nagano, Department of Imaging, A. C. Camargo Cancer Center, São Paulo, Brazil. ste.matw@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nagano SYM, Chojniak R, Porto GC. Magnetic resonance permeability for the evaluation of head and neck tumors: Parotid and beyond. J Clin Imaging Sci. 2025;15:12. doi: 10.25259/JCIS_173_2024
Abstract
Head and neck cancer is the seventh most common cancer globally, with over 300 thousand deaths annually. Magnetic resonance imaging (MRI) of head and neck tumors is a well-known method for its evaluation, although malignant and benign imaging tumors often overlap. Permeability is an advanced method performed by MRI that assist in the diagnosis and evaluation of the neoplasm treatments, having a well-established role in some cases, such as salivary gland tumors, and promising in others, such as squamous cell carcinoma and lymph node evaluation. This pictorial review aims to demonstrate the diverse applications of magnetic resonance permeability imaging in head and neck tumors, highlighting its role in differentiating benign from malignant lesions, such as parotid gland tumors, assessing head and neck squamous cell carcinoma, and evaluating lymph node involvement. By correlating these advanced imaging findings with conventional magnetic resonance techniques, this review aims to enhance radiologists’ understanding of the method and its clinical utility in improving diagnostic and treatment planning.
Keywords
Carcinomas
magnetic resonance imaging
oncology
permeability
head and neck
INTRODUCTION
Head and neck cancer is the seventh most common cancer globally, accounting for over 325,000 deaths annually. The incidence rates are rising, driven by the factors such as human papillomavirus infection and betel nut use.[1] Magnetic resonance imaging (MRI) is a well-known method of imaging used for the evaluation of head and neck tumors being well-known the conventional sequences T1, T2, diffusion, and Gadolinium T1 postcontrast. Although this assessment is widely recognized, there is considerable signal overlap between different head and neck tumors when only conventional techniques are used, making it impossible to distinguish between tumoral types, especially malignant and benign tumors when only the basic signal characteristics are studied.[2] Dynamic contrast enhanced (DCE), on the other hand, is an advanced technique in MRI used to evaluate microcirculation at the capillary level, when contrast passes from the vessels into the interstitial space. This process alters the relaxation time of water molecules and varies depending on the type of tissue involved.[2] Today DCE, also known as permeability, has a well-known role in the evaluation of parotid tumors, mainly because it can effectively differentiate Warthin’s tumor from other types, reducing the need for invasive procedures for this diagnosis.[3] It is also being studied in other areas, such as the evaluation of head and neck squamous cell carcinomas (HNSCC) diagnosis, recurrence and lymph node assessment.[4]
Since permeability is an advanced and relatively unknown technique, most radiologists can only interpret its use in parotid tumors; however, its applications are much broader. The aim of this study is to educate radiologists and other physicians about the additional applications of permeability in the study of the head and neck, such as in the evaluation of the most common head and neck tumor, squamous cell carcinoma, both for staging and posttreatment assessment.
MATERIAL AND METHODS
This retrospective and educational study used anonymized imaging data from a digital archive. As the study involved only anonymized retrospective data, submission to the ethics committee was not required. Data were analyzed to explore permeability’s broader applications in tumor evaluation.
DISCUSSION
Permeability is an advanced technique in MRI used for the evaluation of the microcirculation at the capillary level in a dynamic assessment especially on how the contrast agents pass from the vessel to the extravascular compartment (tissue) and vice versa. These patterns can be measured and correlated to the conventional MRI for the better evaluation of tumors. The principle is based on the fact that malignant tissues have disorganized vessels and promote greater and faster contrast extravasation from the vessel to the tissue and a slower outflow. Some softwares can quantify the rate at which contrast agent moves from the blood plasma into the extravascular extracellular space (Ktrans) and the rate of contrast agent returning to the plasma (Kep)[4] [Figure 1a]. Even when the machine does not have the software available, permeability sequences can be evaluated using qualitative methods. Among these is the graph known as the permeability curve, where the x-axis represents the time since gadolinium injection and the y-axis indicates the signal intensity of the contrast. The curve formed over time displays wash-in and washout values that vary between benign and malignant tumors, with benign tumors generally showing a curve with slow wash-in and progressive washout, while malignant tumors exhibit a curve with rapid wash-in and slower washout, creating a descending pattern[4] [Figure 1b]. In addition to the curves, the machine also generates a parametric color map where areas with higher Ktrans values are represented by warm colors, such as red and orange, and areas with lower values are displayed with cool colors, like blue[4] [Figure 1c].
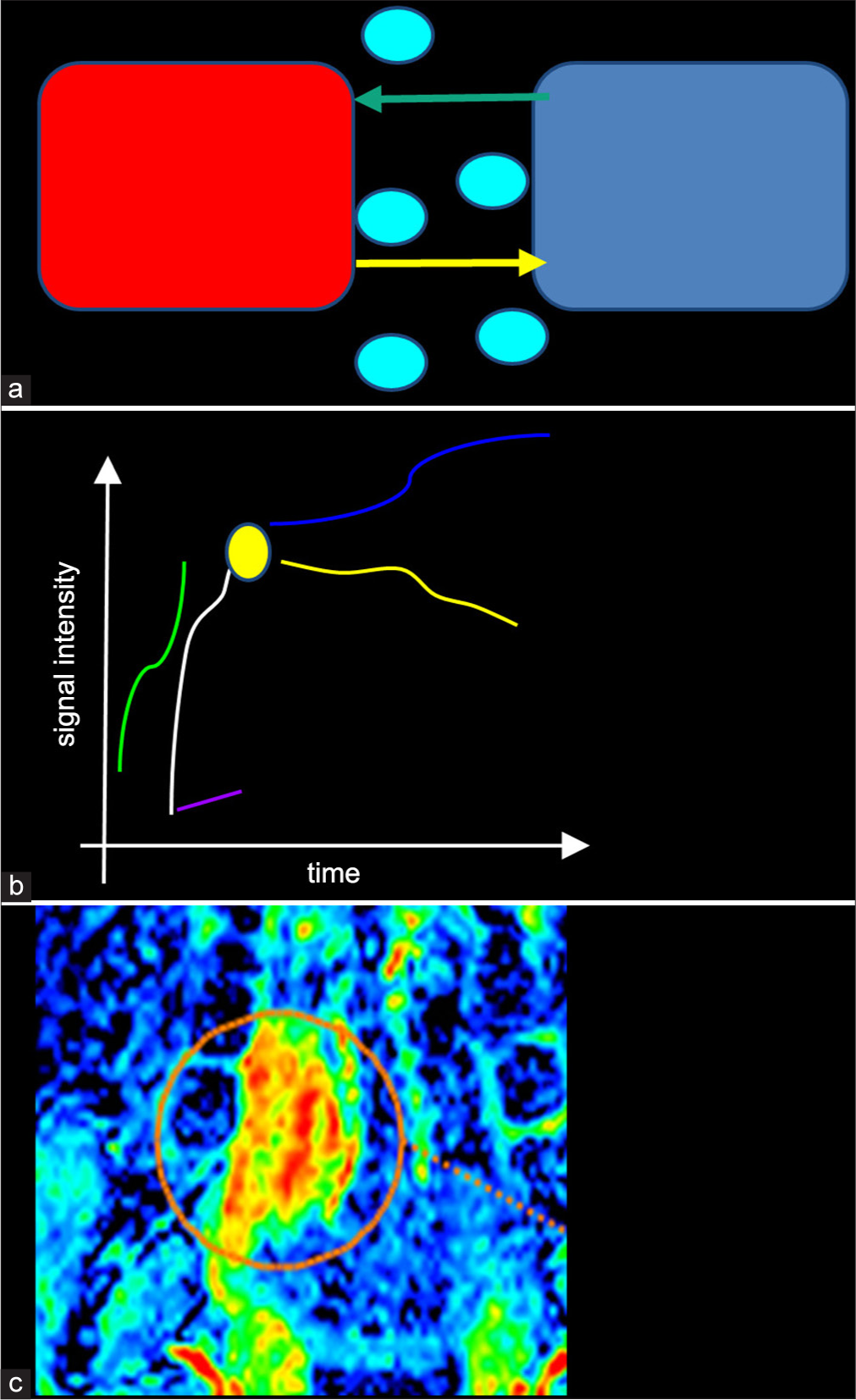
- Physics behind permeability in Dynamic contrast-enhanced magnetic resonance imaging. (a) The diagram demonstrates the interaction between the intravascular (red) and extravascular compartment (blue). Ktrans (yellow arrow) is the transfer constant that quantifies the transfer of contrast (blue circle) from the vascular to the extravascular space and Kep (green arrow) is the rate of contrast that returns to the vessel. (b) The graph illustrates the permeability dynamics based on DCE imaging. The evaluation is a semiquantitative method, demonstrating the initial enhancement curve (wash-in -white line) that represents the rise in signal intensity as the contrast agent transfers to the extravascular compartment; the time to peak (purple line) that is the time to reach the maximum signal intensity (yellow circle) and the washout that indicates how the contrast is returning to the vessel. The washout of malignant tumors usually follows a descending pattern (yellow line), whereas benign lesions follow an ascending pattern (blue line). (c) A parametric image visually represents voxel-by voxel data from the quantitative DCE, indicate varying intensities of the parameters. Warmer colors highlight regions of higher permeability. This patient had an oral tongue neoplasm, demonstrated inside the orange circle.
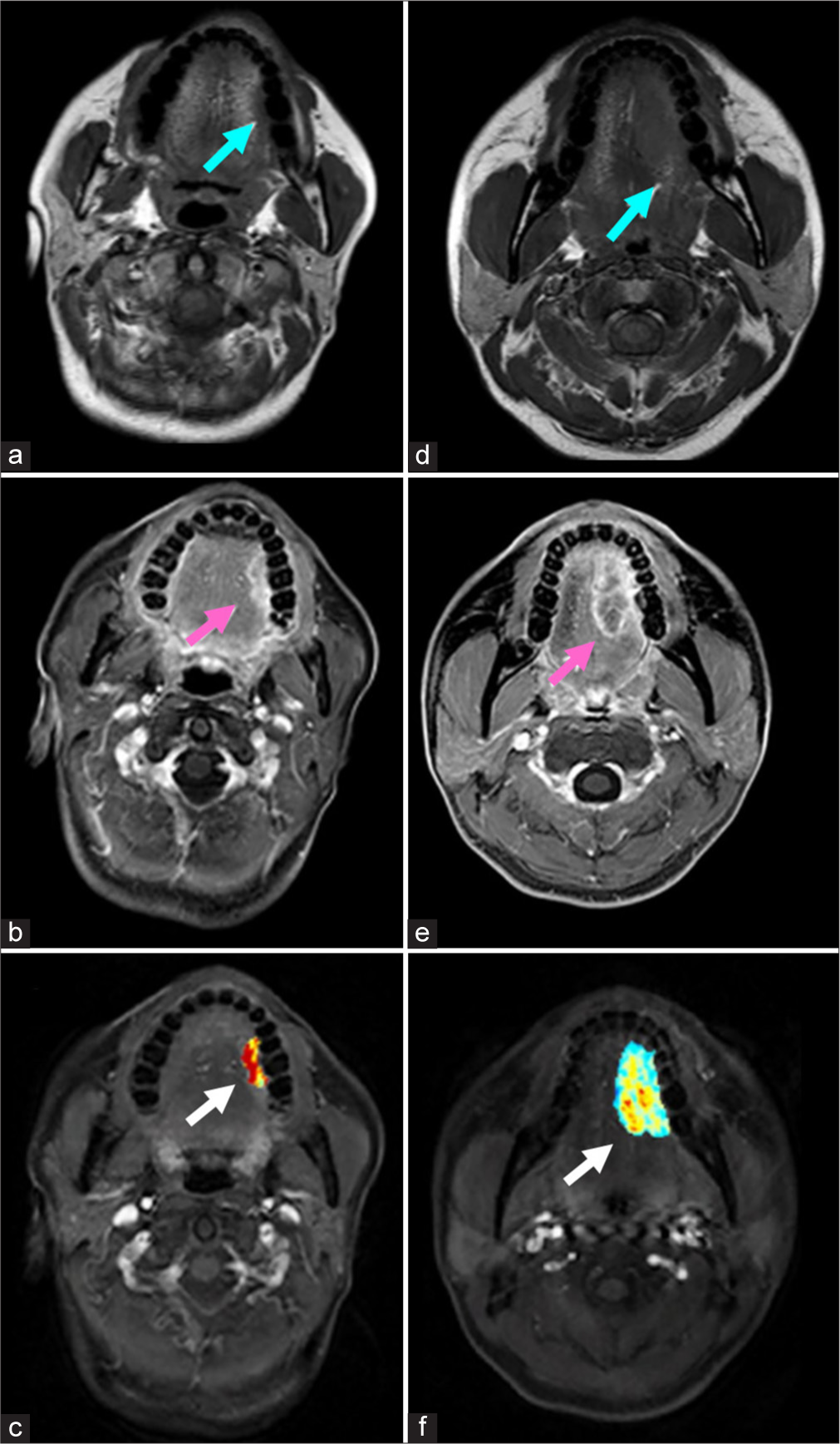
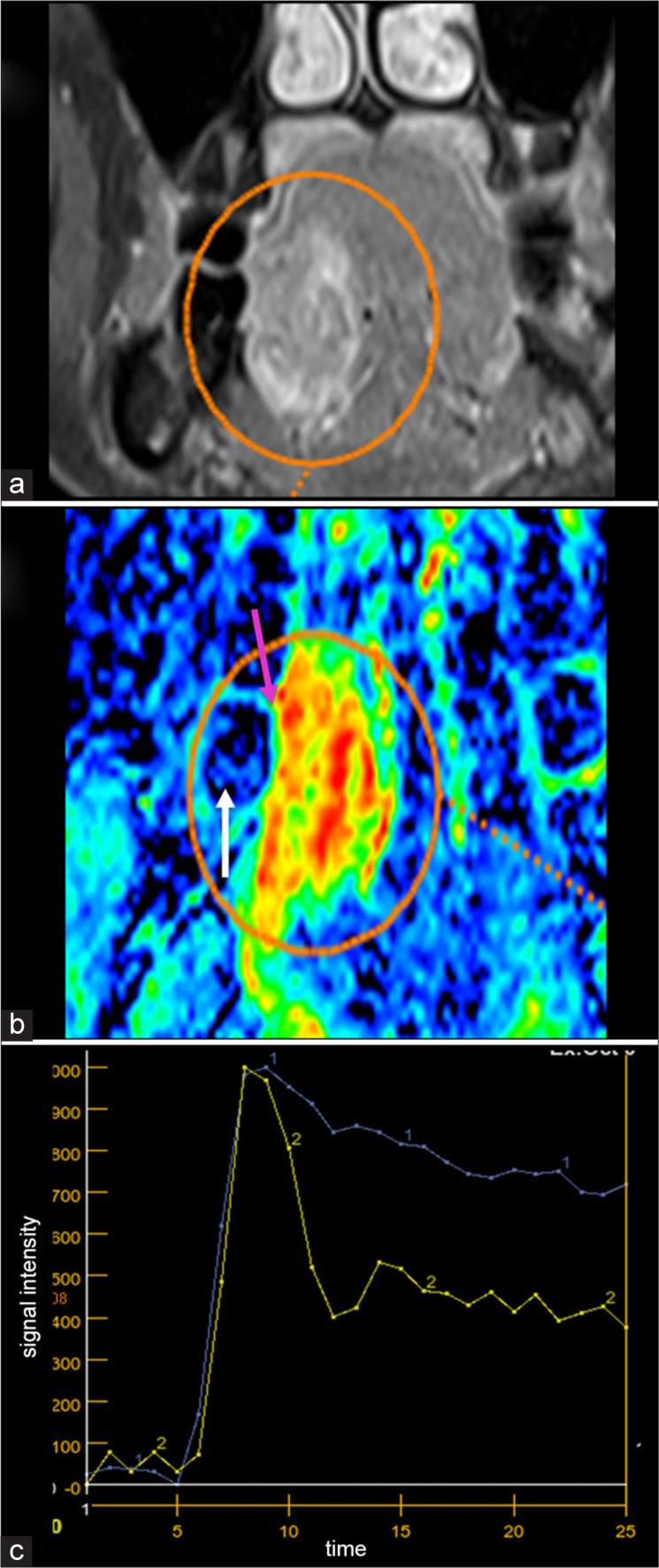
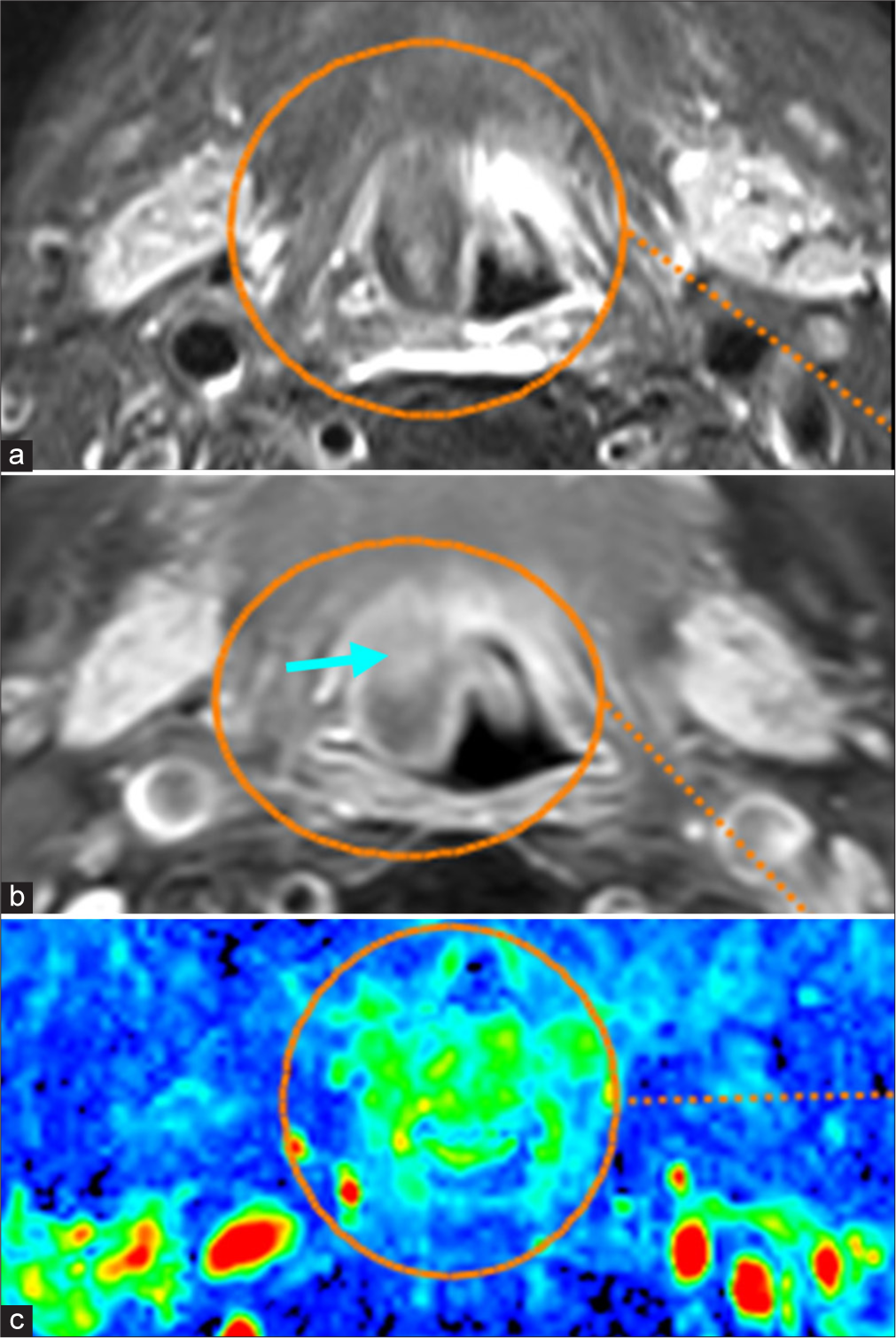
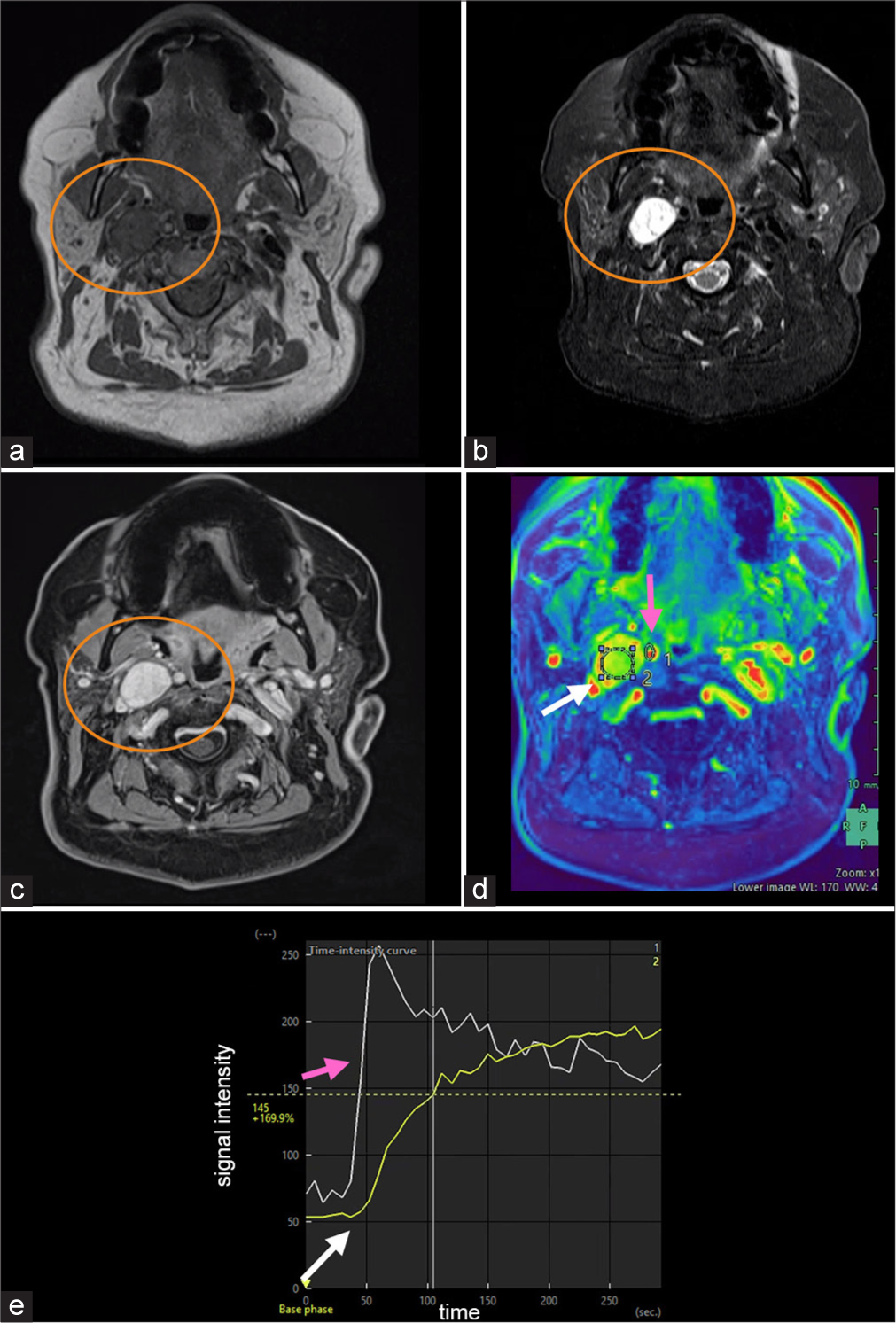
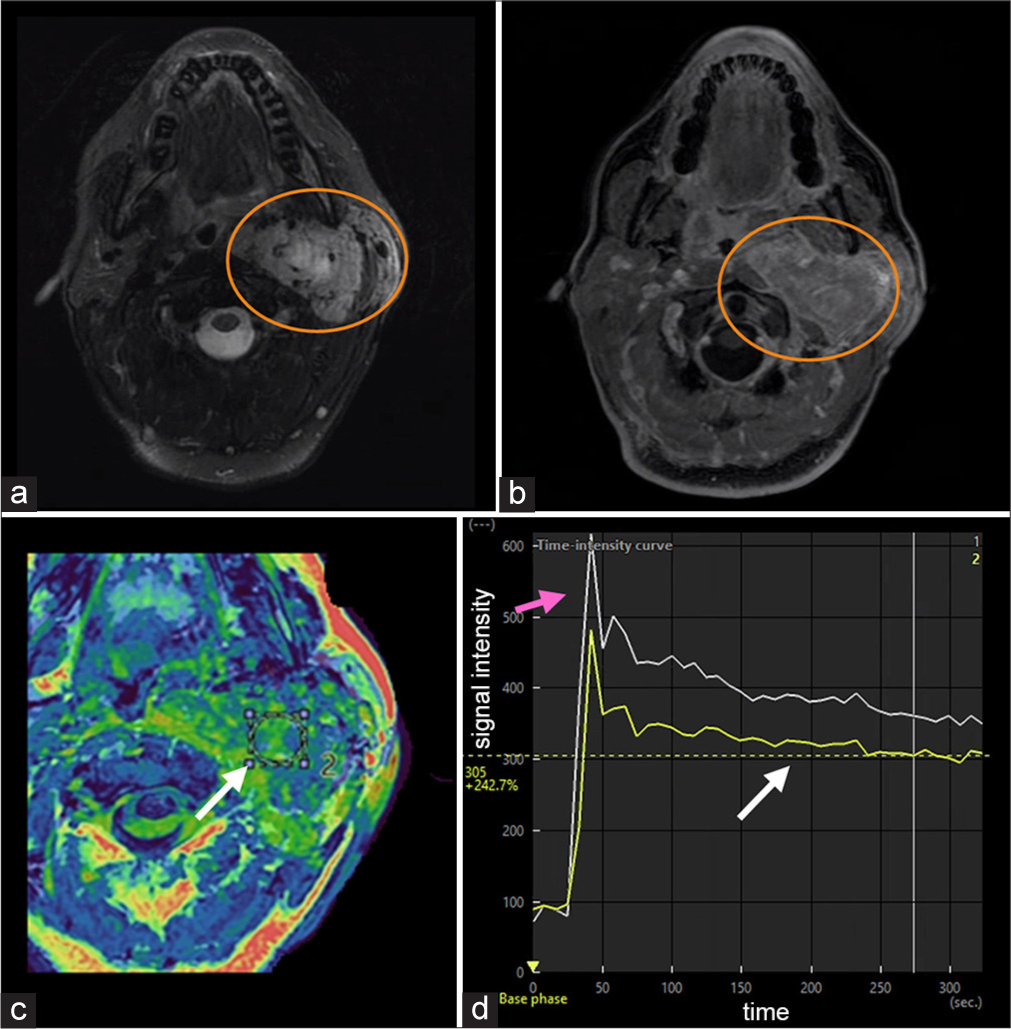
The initial studies of MRI DCE were conducted to evaluate parotid tumors, and today, it is a validated complementary method that can even exclude the need for fine-needle biopsy in certain cases, such as when conventional imaging and permeability findings are consistent with a Warthin tumor.[4] Tumors have distinct signal characteristics in conventional and permeability imaging, which can assist in the diagnosis. Pleomorphic adenoma typically shows high signal on T2 [Figure 2a], no diffusion restriction, high-permeability voxels represented by warm colors [Figure 2b], and an ascending permeability curve[3] [Figure 2c]. Warthin tumor’s usually exhibit isointense or low T2 signal [Figure 3a], high-permeability voxels represented by warm colors [Figure 3b] and permeability with a washout >30% [Figure 3c and d], while malignant tumors, such as adenoid cystic carcinoma, tend to present with variable T2 signal [Figure 4a], diffusion restriction [Figure 4b], color map [Figure 4c], a rapid ascending curve, and a descending plateau washout [Figure 4d].[3]
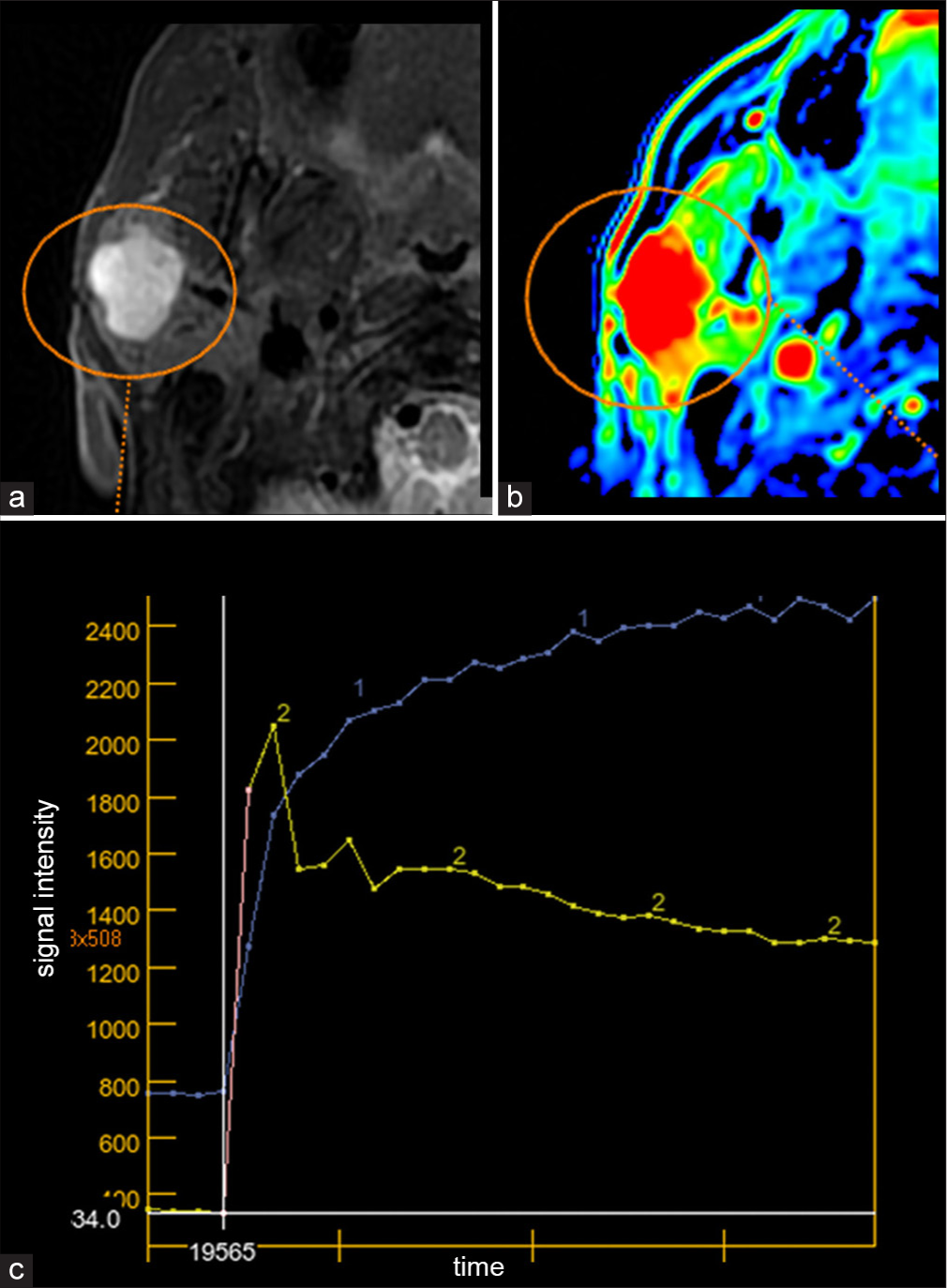
- A 26-year-old patient presents with a palpable nodule on the right side of the face. Magnetic resonance and permeability of the face was performed and a nodule was found at the right parotid gland (orange circle indicates the lesion on figures a and b). Further evaluation by pathology confirmed the pleomorphic adenoma diagnosis. (a) Nodule in the right parotid gland with hyperintensity on T2-weighted images, well-demarcated. (b) Colorcoded permeability map (voxel-byvoxel) showing warm colors due to increased blood volume at the site. (c) Permeability graph illustrating permeability of the lesion (curve 1) in the right parotid gland compared to the carotid artery (curve 2). The lesion has a slightly slower wash-in and slow and ascending washout.
- A 40-year-old patient presented to a routine examination and found an incidental finding in the left parotid gland. Biopsy was performed and the diagnosis of Warthin’s tumor was confirmed. (a) Nodule in the left parotid gland with isointensity on T2-weighted images, well-demarcated (orange circle). (b) Color-coded permeability map (voxel-by-voxel) showing increased permeability (“warm colors”) at the site (orange circle). (c) Permeability graph showing rapid wash-in (blue arrow). (d) Permeability graph depicts more than 30% washout (pink arrow).
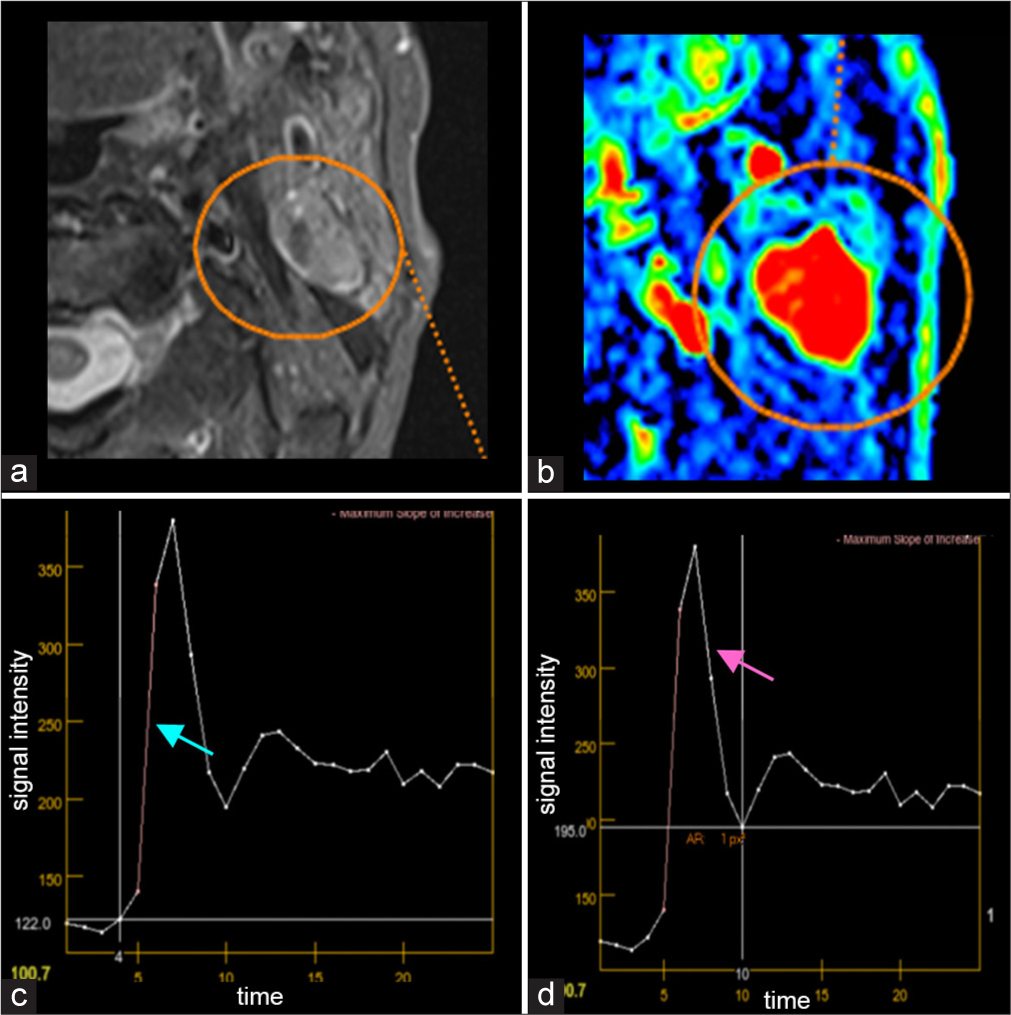
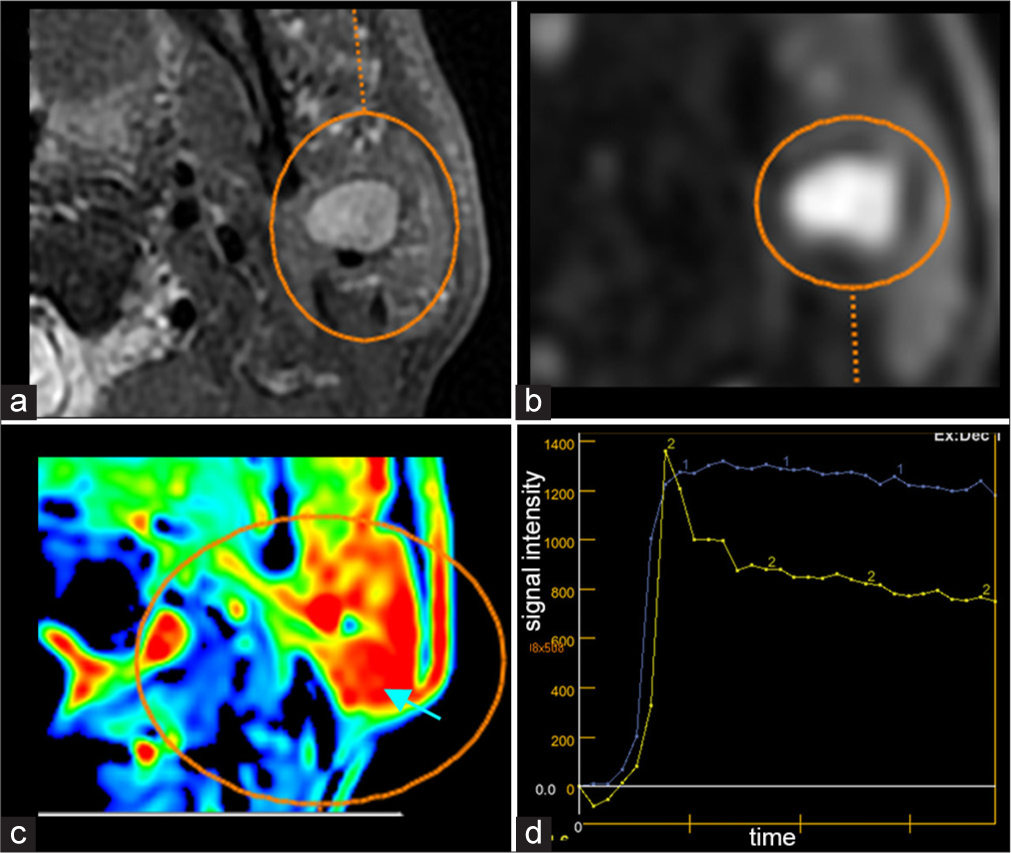
Other applications are being studied for head and neck tumors, many of them focusing on the assessment of HNSCC. Some studies focus on the staging process, aimed at the evaluation of tumor extent. For example, for laryngeal neoplasms, edema or reactive thickening of the laryngeal cartilage may occur [Figure 5a and b], and permeability studies can be useful in differentiating between stages T3 and T4, especially concerning possible lateral margin extension with thyroid cartilage involvement[5] [Figure 5c]. In addition to the evaluation of tumor extent, some quantitative methods of permeability used in staging assessment can also provide information on the stages of squamous cell carcinoma. This has been described in oral cavity tumors, particularly in tongue neoplasms, where the constant Kep, which, as previously mentioned, represents the rate of contrast returning to the plasma, has been characterized as an independent predictor of higher stages of squamous cell carcinoma (stages III and IV). Usually, in advanced stages, Kep is reduced because of tumor hypoxia and reduction in functional microvascularization [Figure 6] - adapted from Guo et al. (2020).[6] In the staging evaluation process, the qualitative and quantitative characteristics of the permeability graph in HNSCC follows the same pattern as malignant parotid tumors, with a high Ktrans, and a rapid wash-in and slow washout. Remember that, in addition to the graph, the parametric map also provides information on areas with higher permeability (indicated by warmer colors) and can assist in the evaluation of head and neck squamous cancer,[4] for example, in the oral tongue [Figure 7] and oropharynx [Figure 8]. An additional aspect of permeability is in the evaluation of HNSCC after treatment. As previously exemplified, malignant tumors typically have a poorly organized capillary network, and permeability studies help in the early detection of recurrence, assessing tumor extent, and facilitating staging. Posttreatment changes (radiotherapy and chemotherapy) include fibrosis, edema, and soft-tissue thickening, sometimes even necrosis, and distinguishing between posttreatment changes and tumor recurrence can be challenging. Studies have shown that when permeability is included in the evaluation of posttreatment squamous cell carcinoma, it can cause a reduction in false positive and negative rates compared to when evaluating MRI alone and also improve specificity[7] [Figures 9 and 10]. Quantitative permeability parameters in HNSCC assessment have also been correlated with immunohistochemical tumor findings. Especially Ktrans has the potential to indicate angiogenesis and proliferative activity which are often linked to higher grade tumors and worse prognosis.[8]
- A 43-year-old patient underwent a complementary examination following the detection of a nodule on computed tomography. The nodule was subsequently removed, and the diagnosis confirmed adenoid cystic carcinoma. (a) Nodule in the left parotid gland with hyperintensity on T2-weighted images, well-demarcated (orange circle). (b) The nodule exhibits intense diffusion restriction (orange circle). (c) Color-coded permeability map (voxel-by-voxel) showing increased permeability (“warmer colors”) at the site (orange circle). Note the central areas appeared warmer (blue arrow). (d) Permeability graph showing that the lesion (curve 1) has a rapid wash-in compared to the carotid artery (curve 2) and a washout with a descending plateau tendency.

- A 65-year-old patient with hoarseness presents for an initial evaluation. Magnetic resonance imaging reveals a lesion in the anterior commissure, suspicious for laryngeal neoplasia. (a) Lesion in the anterior commissure of the larynx with hypointensity on T1-weighted images (orange circle). Movement artifacts in T1-weighted sequences hindered assessment of thyroid cartilage invasion ipsilaterally. (b) The lesion shows hyperintensity on T2-weighted images, with associated edema (orange ellipse). There is no evidence of thyroid cartilage involvement (pink arrows). (c) Color-coded permeability map demonstrates increased permeability (“warmer spot” - orange circle) in the anterior commissure.
- (a) Axial pré-contrast T1-weighted image showing the tumor (blue arrow) in a patient with an early-stage lesion. (b) Axial postcontrast T1-weighted image demonstrating tumor enhancement (pink arrow) in the early-stage lesion. (c) Color-coded Kep map (voxel-by-voxel) of the early-stage lesion, with warm colors indicating higher permeability. The Kep value in the early-stage lesion (white arrow) is 0.995 min-1. (d) Axial pré-contrast T1-weighted image showing the tumor (blue arrow) in a patient with an advanced-stage lesion. (e) Axial postcontrast T1-weighted image demonstrating tumor enhancement (pink arrow) in the advanced-stage lesion. (f) Color-coded Kep map (voxel-byvoxel) of the advanced-stage lesion, with warm colors indicating higher permeability. The Kep value in the advanced-stage lesion (white arrow) is 0.503 min-1.
- A 53-year-old patient was referred by a general practitioner due to an ulcerated lesion on the oral tongue. Magnetic resonance imaging revealed a lesion on the lateral border of the tongue. The patient subsequently underwent surgery, with histopathological analysis confirming squamous cell carcinoma. (a) Lesion at the oral thong with high signal intensity on T2 (orange circle). (b) The lesion has increased blood flow on permeability study (warmer spot - orange circle). This image also helps evaluate the lesion margins because there is a separation (pink arrow) between the warmer spot and the adjacent teeth (white arrow). (c) The lesion (curve 1) has a rapid wash-in, similar to that of the carotid artery (curve 2), with a descending washout, which is also a common finding in malignant tumors.
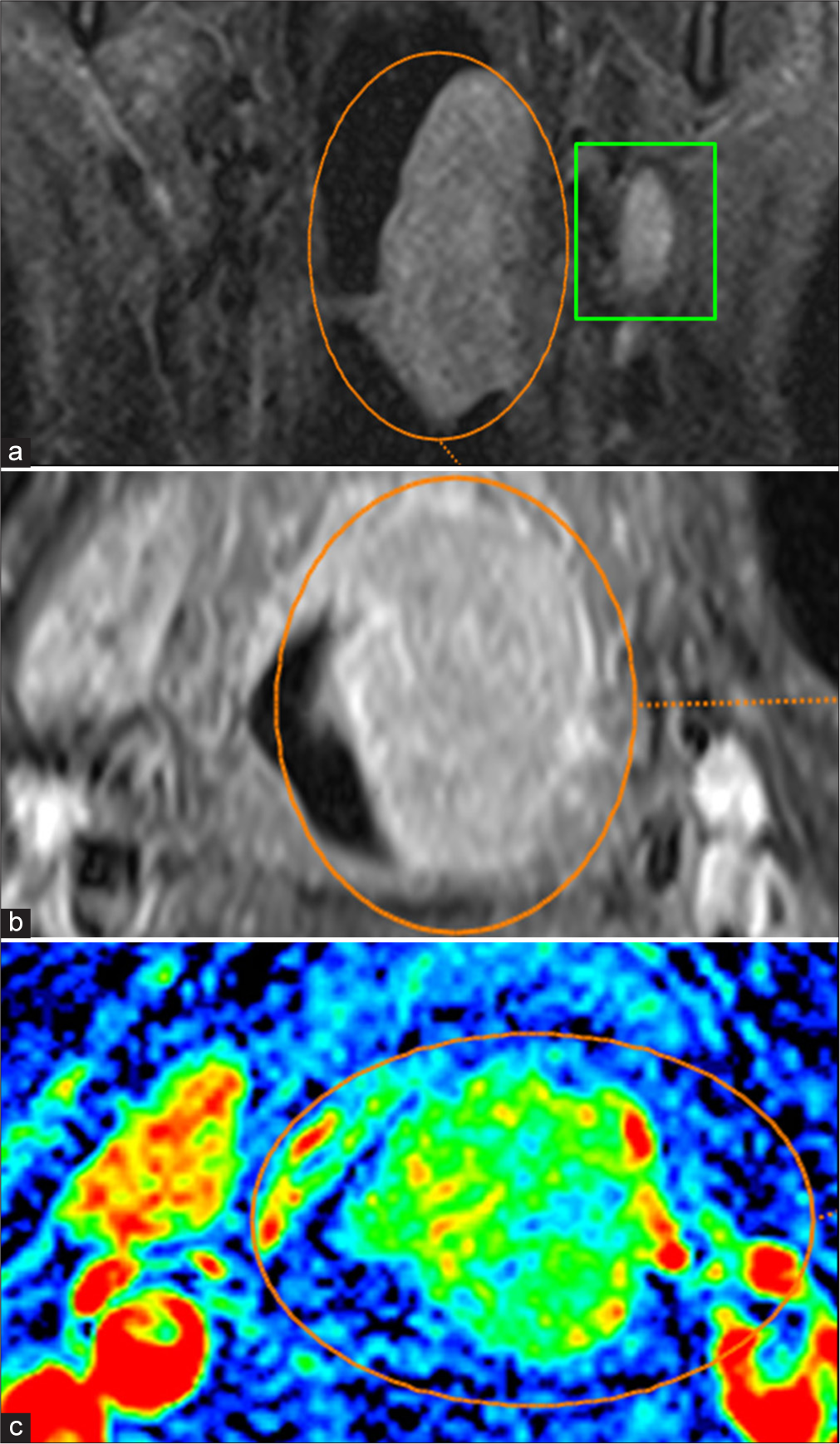
- A 58-year-old patient presents with persistent sore throat, dysphagia, and a sensation of a leftsided neck mass. Physical examination revealed hypertrophy of the left tonsil with visible ulceration. (a) Staging of left oropharyngeal neoplasm, revealing a lesion with high signal intensity on T2, endophytic to the lumen (orange circle), and an atypical lymph node adjacent to the lesion (green rectangle). (b) The lesion exhibits intense enhancement with contrast (orange circle). (c) Voxel-by-voxel color permeability map illustrating increased blood volume at the site (orange circle), supporting the hypothesis of a primary lesion.
- A 62-year-old patient with a history of right tonsil carcinoma treated surgically presents for routine follow-up imaging. Magnetic resonance imaging revealed a new enhancing lesion at the surgical bed of the right tonsil, with irregular margins and extension to the lateral oropharyngeal wall, suggestive of tumor recurrence that was confirmed after biopsy. (a) A lesion with low signal intensity on T1 is observed in the right tonsillar fossa (orange circle). (b) There is confluence of the lesion with areas of post-treatment edema (orange circle), making it difficult to accurately delineate the lesion and assess involvement of the carotid artery (pink arrow). (c) The color-coded permeability map demonstrates increased blood volume at the site (orange circle). Compare with the contralateral site. (d) Although some artifacts, it can be seen that the permeability curve has a rapid wash-in and slow, descending plateau washout, commonly observed in malignant lesions.
- A 59-year-old patient with a history of vallecular squamous cell carcinoma on the right side, treated with chemoradiotherapy, presents for restaging. Magnetic resonance imaging shows post-treatment changes in the right vallecular region, including fibrosis and soft tissue thickening, but there was an enhancing area, suspect for recurrence. This patient underwent surgery following the study, and the histopathological examination confirmed a positive finding for local recurrence. (a) Restaging of right vallecular neoplasm, revealing a possible residual lesion (orange circle) but with assessment hampered by edema resulting from post-treatment changes. (b) The lesion demonstrates mild enhancement with contrast medium (orange circle), with a focal area of increased enhancement observed (blue arrow), raising suspicion of residual or recurrent disease. (c) Voxel-by-voxel color permeability map illustrating mild elevated blood volume at the location (orange circle), strengthening the hypothesis of a residual lesion.
Another application is in identifying and differentiating between benign and malignant lymph nodes, as the former usually exhibit a higher permeability.[9] In the context of lymph nodes, studies have also been conducted to determine whether the presence of metastatic lymph nodes can predict patients’ prognosis posttreatment. There is evidence suggesting that their response to chemotherapy and radiotherapy depends on the amount of oxygen present in the tumor. Thus, lymph nodes with reduced permeability are likely to have a worse prognosis[9] [Figure 11].
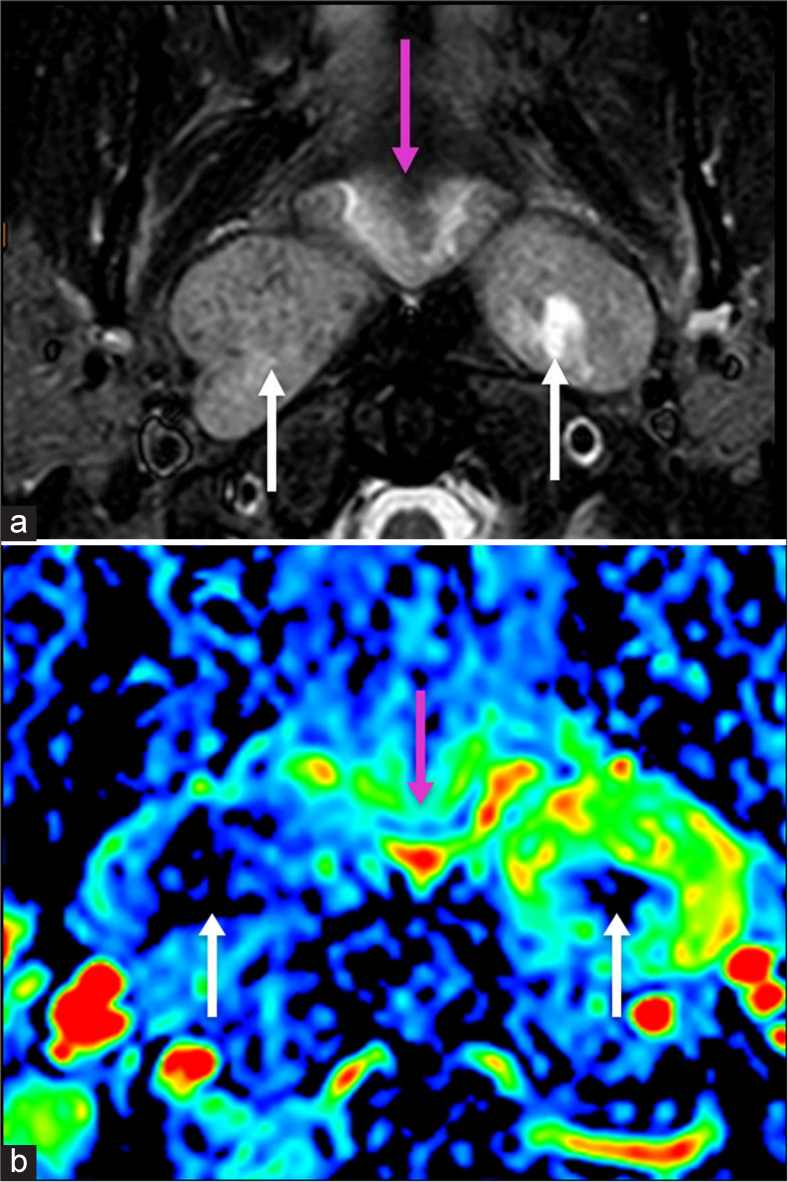
- A 42-year-old patient comes from evaluation of a nasopharynx squamous cell carcinoma. Lymph node evaluation demonstrates metastatic lymph nodes at retropharyngeal space. (a) Nasopharynx lesion (pink arrow) and retropharyngeal lymph nodes (white arrows) with a metastatic appearance. (b) Permeability images reveal increased blood volume in the nasopharynx (primary tumor – pink arrow) and at the retropharyngeal lymph nodes, supporting the hypothesis of metastatic lymphadenopathy. Note that the right and the center of the left lymph nodes (white arrows) have a decreased permeability, probably due to central lack of oxygen common in lymph node necrosis.
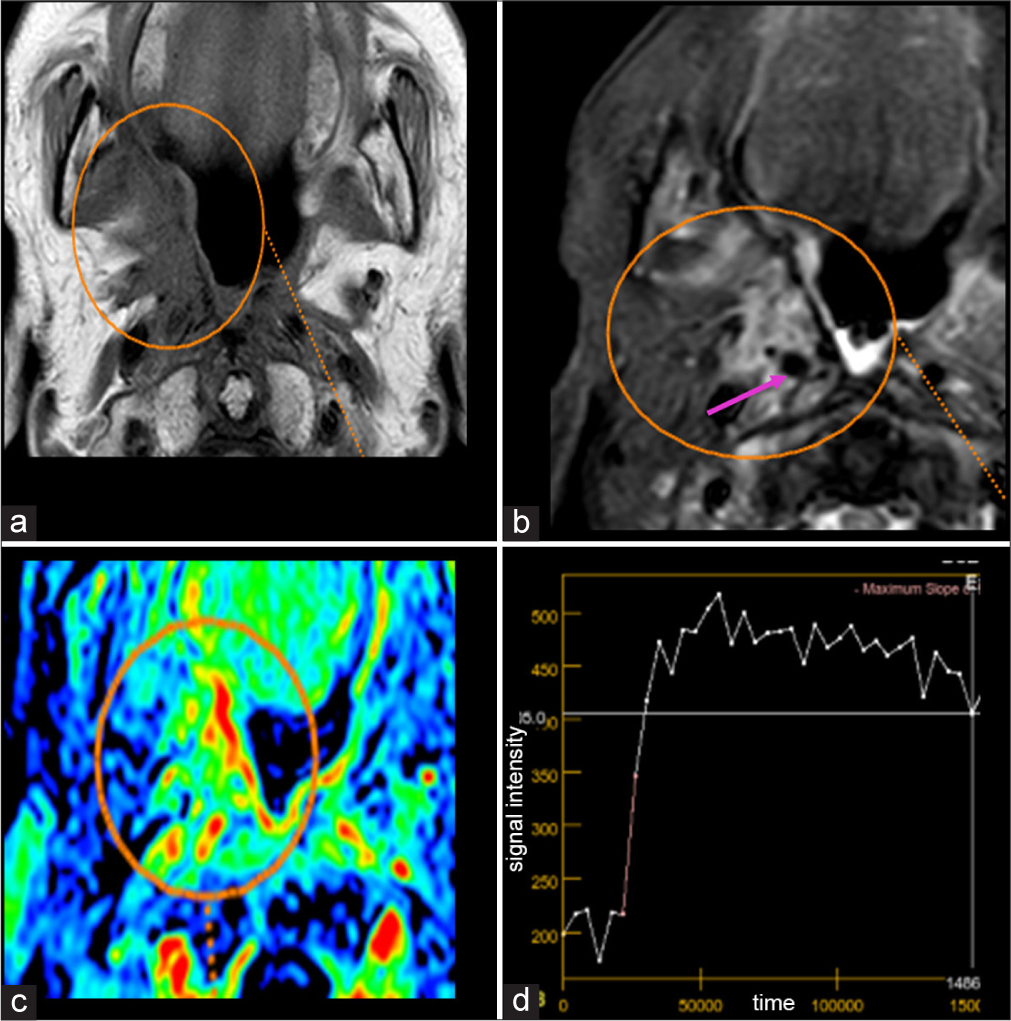
Permeability imaging has been explored in head and neck tumors beyond its established roles previously depicted. Notably, it aids in differentiating neural sheath tumors and paragangliomas, with schwannomas typically exhibiting slower wash-in and wash-out curves reflecting their more structured microvascular architecture [Figure 12]. In contrast, paragangliomas due to their high vascularity show rapid wash-in and washout [Figure 13] and also higher Ktrans and Kep.[10] In addition, permeability imaging has shown promise in the differentiation of benign and malignant thyroid and orbital tumors, further expanding its clinical applications.[10] These differences highlight the potential of DCE-MRI in improving diagnostic accuracy and reducing the need for invasive procedures.
- Incidental finding in a 70-year-old patient that underwent carotid magnetic resonance (MR) angiography for headache. A dedicated neck magnetic resonance imaging was performed, confirming a well-defined lesion in the right carotid space, suggestive of a vagal schwannoma. (a) Lesion with hypointensity on T1 (orange circle). (b) Lesion homogenous and with hyperintensity on T2 (orange circle). (c) Post-contrast enhancement (orange circle). (d) Color permeability map with region-of-interests in the lesion (white arrow) and adjacent vessel (pink arrow). (e) Permeability graph comparing the vessel (pink arrow) and the lesion (white arrow), showing slow wash-in and gradual ascending washout.
- 56-year-old patient with cervical pain, presenting a vascularized expansile lesion in the left carotid space with flow-voids, consistent with a vagal paraganglioma and confirmed after surgical removal. (a) T2-weighted image showing flow voids (orange circle). (b) Post-contrast image with heterogeneous enhancement (orange circle). (c) Color-coded permeability map with region-of-interest in the lesion (white arrow), indicating increased blood volume. The adjacent vessel is not shown in this slice but was assessed in another section. (d) Permeability graph comparing the wash-in of the lesion (white arrow) and the vessel (pink arrow), demonstrating rapid wash-in, close to the vessel and rapid washout immediately after the peak.
All of this demonstrates the versatility and importance of DCE in the daily study of head and neck tumors.
CONCLUSION
Permeability imaging through DCE-MRI has become a great tool in the evaluation of head and neck tumors, offering enhanced diagnostic accuracy, staging, and treatment monitoring. Its ability to quantify vascular dynamics and differentiate between benign and malignant lesions complements conventional MRI, reducing false positives and negatives, and improving sensitivity and specificity. Beyond parotid tumor characterization, its applications extend to staging and recurrence of HNSCC, lymph node analysis, and ongoing studies exploring tumor biomarkers and other tumor types.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Reviewing the epidemiology of head and neck cancer: Definitions, trends and risk factors. Br Dent J. 2022;233:780-786.
- [CrossRef] [PubMed] [Google Scholar]
- Perfusion and permeability imaging for head and neck cancer: Theory, acquisition, postprocessing, and relevance to clinical imaging. Magn Reson Imaging Clin N Am. 2018;26:19-35.
- [CrossRef] [PubMed] [Google Scholar]
- Interpretation pearls for MR imaging of parotid gland tumor. Eur Ann Otorhinolaryngol Head Neck Dis. 2013;130:30-5.
- [CrossRef] [PubMed] [Google Scholar]
- Dynamic contrast-enhanced MR imaging in head and neck cancer: Techniques and clinical applications. AJNR Am J Neuroradiol. 2016;37:588-95.
- [CrossRef] [PubMed] [Google Scholar]
- Functional magnetic resonance imaging of head and neck cancer: Performance and potential. Neuroradiol J. 2019;32:36-52.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitative dynamic contrast-enhanced MR imaging can be used to predict the pathologic stages of oral tongue squamous cell carcinoma. BMC Med Imaging. 2020;20:117.
- [CrossRef] [PubMed] [Google Scholar]
- Detection of local recurrence in patients with head and neck squamous cell carcinoma using voxel-based color maps of initial and final area under the curve values derived from DCE-MRI. AJNR Am J Neuroradiol. 2019;40:1392-401.
- [CrossRef] [PubMed] [Google Scholar]
- The correlations between dynamic contrast enhanced magnetic resonance imaging and immunohistochemical data in head and neck squamous cell carcinomas. Turk J Med Sci. 2022;52:26.
- [CrossRef] [PubMed] [Google Scholar]
- Dynamic contrast-enhanced magnetic resonance imaging as a predictor of outcome in head and neck squamous cell carcinoma patients with nodal metastases. Int J Radiat Oncol Biol Phys. 2012;82:1837-44.
- [CrossRef] [PubMed] [Google Scholar]
- Dynamic contrast-enhanced magnetic resonance imaging for differentiating head and neck paraganglioma and schwannoma. Head Neck. 2021;43:2611-22.
- [CrossRef] [PubMed] [Google Scholar]







