Translate this page into:
Magnetic Resonance Enterography Findings in Crohn′s disease in the Pediatric Population and Correlation with Fluoroscopic and Multidetector Computed Tomographic Techniques
Address for correspondence: Dr. Parul Patel, University of Rochester Medical Center, 284 Wintergreen Way, Rochester, NY - 14618, USA. E-mail: parul_patel@urmc.rochester.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Traditionally, fluoroscopic examinations such as enteroclysis, upper GI studies, and small bowel follow through exams have been the procedures of choice in evaluating inflammatory bowel disease (IBD) in pediatric populations. With the advent of multidetector computed tomography (MDCT), it has subsequently become a complementary examination in imaging inflammatory bowel disease. A major advantage of MDCT over fluoroscopic examination is its ability to directly visualize bowel mucosa, as well as demonstrate extra-enteric complications of IBD such as abscesses, fistulae, and sinus tracts. The major disadvantage of CT however is exposure to ionizing radiation, especially in IBD patients of the pediatric age group who maybe repeatedly imaged due to exacerbations. As a result, magnetic resonance enterography (MRE) is becoming increasingly important in the evaluation and follow-up of pediatric patients with IBD. This pictorial essay will summarize the multi-modality imaging findings of IBD with emphasis on MRE including the imaging protocol and procedure. For the purposes of this article, patients less than 17 years of age have been considered to represent the pediatric population.
Keywords
Inflammatory bowel disease
magnetic resonance enterography
pediatric
INTRODUCTION

The incidence of pediatric inflammatory bowel disease is rising in the western world.[1] Traditionally, fluoroscopic examinations, such as enteroclysis, upper GI studies, and small bowel follow through studies have been the examinations of choice in evaluation of inflammatory bowel disease (IBD) in the pediatric population. With the advent of multidetector computed tomography (MDCT), it subsequently became a complementary exam in imaging IBD. Radiation exposure related to MDCT, especially in the pediatric population has led to recent advances in the utilization of magnetic resonance enterography (MRE) as a tool in the evaluation of IBD. In this pictorial essay, we use case examples to highlight the strengths and weaknesses of the various imaging modalities used in the evaluation of Crohn′s disease. For the purposes of this article, patients less than 17 years of age are considered to represent the pediatric population.
Pediatric inflammatory bowel disease
IBD typically presenting in teens and early twenties, is thought to have a multi-factorial etiology, involving genetic, immunologic, and infectious factors. The two major subtypes of IBD are ulcerative colitis and Crohn′s disease. In children, the incidence of Crohn′s disease is twice as high as ulcerative colitis.[1] This pictorial essay will focus on the multi-modality imaging findings of Crohn′s disease.
IBD typically presents in late childhood and early adolescence. However, with the increase in incidence in a pediatric population, now patients are presenting at younger ages. Crohn′s disease affects the bowel extending from the mouth to the anus, whereas ulcerative colitis is confined to the colon. Also, with ulcerative colitis, active lesions are contiguous, whereas skip lesions are seen with Crohn′s disease. There is a higher malignant potential with ulcerative colitis, however malignancy is also associated with colonic involvement in Crohn′s disease. Major complications of Crohn′s disease include strictures and fistulas, and imaging studies are commonly performed to evaluate these lesions.
Traditional imaging of inflammatory bowel disease
Traditionally, fluoroscopic examinations, including upper GI studies and small bowel follow through exams were imaging studies of choice in evaluation of IBD. Flouroscopic studies provide information about intraluminal disease extension, stricture formation, wall thickening, and abnormalities in small bowel motility.[2] These exams are however limited in their ability to provide direct information regarding extra-intestinal findings of IBD, as well as the ability to directly visualize the bowel mucosa [Figures 1a and b].

- (a) Overhead image from a small bowel follow through in a patient with history of Crohn's disease demonstrates evidence of terminal ileal wall thickening, causing narrowing of the lumen. (b) Spot view of the terminal ileum in a small bowel follow through demonstrates similar findings in a second patient with terminal ileitis.
With the advent of MDCT, it has become a complementary exam in following exacerbations of IBD. MDCT is superior to fluoroscopic exams in its ability to directly visualize bowel mucosa, while also allowing for the evaluation of extra-enteric complications of IBD. A major disadvantage of MDCT, however, is the exposure to a higher dosage of ionizing radiation. A study by Jaffe et al demonstrates that effective doses are up to five times higher with MDCT when compared with small bowel follow through (SBFT) examinations.[3] This is especially important when imaging the IBD in the pediatric age group, as these patients may be repeatedly imaged due to multiple flares.
Previously, MRI had a limited role in the evaluation of bowel due to motion artifact and poor contrast resolution. With the advent of faster techniques that are less sensitive to motion (single shot spin echo images, fat supressed breath hold images), MRE is being increasingly used for the evaluation of IBD in children as it offers a test which can be repeated and reproduced without the ill effects of repeated exposure to radiation. A study by Seung Soo lee et al demonstrated that MRE has a diagnostic effectiveness comparable to that of CT enterography.[4] Furthermore, because MRE findings have been found to correlate well with clinical evaluation, endoscopy, and histological findings, surgeons and gastroenterologists are becoming more and more comfortable ordering these exams.
Magnetic resonance enterography
Patient preparation and imaging protocol
Proper bowel distension with oral contrast is a key part of patient preparation for MRE, and crucial for a good quality, diagnostic exam. Oral contrast reduces luminal air that can cause susceptibility artifact. The ideal contrast agent stays within the bowel lumen for the duration of the exam, is absorbed minimally, and evacuated completely.
Oral contrast can be ingested or administered via a nasogastric tube. Most centers administer orally to minimize patient discomfort. In adults, several oral contrast agents have been used, however in children, only a few have been used. Biphasic agents that are low signal on T1 weighted images and high signal on T2-weighted images are used. Initially, a mixture of mannitol and polyethylene glycol was used as an oral contrast agent in children. Volumen, is a biphasic oral contrast agent that has been increasingly given to children. It consists of a mixture of low concentration barium and sorbitol. The role of mannitol and sorbitol in their respective formulations is to draw fluid into the bowel lumen, this is due to their high osmolarity. Known possible adverse effects of these oral contrast agents include abdominal discomfort, cramping, nausea, vomiting, and diarrhea. Several pediatric studies have demonstrated that a total volume of up to 1000 ml, 1 hour prior to scan is optimal for good bowel distension.[5] At our institution, we have seen good results with a minimum of 800 ml Volumen.
When performing MRE examinations, anti-peristaltic agents are routinely utilized as a tool to halt peristalsis (decrease motion artifact), and reduce cramping related to oral contrast agents. In the USA, glucagon is the commonly used agent. Usually, two doses are administered. The first dose, 0.25 mg glucagon, is given subcutaneously when the patient is on the table, prior to starting the scan. The second dose, also 0.25 mg is given intravenously over 1 min, prior to gadolinium administration.[5] At our institution, we routinely omit the second dose to decrease patient discomfort, without affecting image quality.
Patients should have taken nothing by mouth (NPO) 6 hours before the examination. Patients are asked to void prior to getting on the table, as a full bladder can obscure visualization of the sigmoid colon and distal small bowel loops. Patients are positioned prone on the MRI table as pressure from the table causes increased bowel distention in at least the most anteriorly placed bowel loops.
The MR protocol at University of Rochester Medical Center (URMC) includes a field of view from the splenic flexure to the pelvis. T2-weighted sequences including single shot fast spin echo (SSFSE) allow fast imaging and limit motion blurring. A typical scan consists of initial coronal and axial SSFSE, dynamic contrast sequences (LAVA on GE equipment, THRIVE on Phillips equipment, VIBE on Seimen′s equipment and Radiance on Toshiba equipment) and delayed coronal and axial SSFSE images. The delayed SSFSE images are useful in differentiating peristalsis from fixed wall thickening or luminal narrowing of bowel loops. Figures 2a and 2b illustrate a normal MRE study. Figures 3a and 3b demonstrate a case of poor luminal dilatation. In a case such as this one, it would be difficult to assess areas of wall thickening and luminal narrowing versus poor distension.

- Normal study with good bowel distension: (a) T2-weighted postcontrast coronal view of the abdomen demonstrates good bowel distension (arrows) and no abnormal areas of wall thickening or luminal narrowing. (b) Note the bowel wall enhancement is similar to that of the kidneys at the same vascular phase.

- (a) Coronal and (b) axial T2-weighted images of the abdomen demonstrate an example of poor bowel distension. Compare the amount of intraluminal contrast in this study with that seen in Figure 2.
Image interpretation
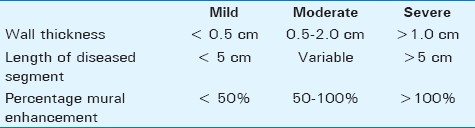
MRI criteria of disease severity have been previously described as a function of wall thickness, length of diseased segment, and percentage of mural enhancement [Table 1]. Disease severity is categorized as mild when a less than 5 cm segment of bowel is noted to demonstrate less than 0.5 cm wall thickness and less than 50% mural enhancement. With severe disease, a greater than 5 cm segment of bowel demonstrates more than 1 cm wall thickness and greater than 100% mural enhancement. With moderate disease, there is 0.5 to 2.0 cm wall thickening and 50-100% mural enhancement of a variable length of the bowel.[6] Figures 4a–c provide an example of severe disease based on these criteria.

- (a) Coronal T2-weighted and (b) post-contrast T1-weighted images of the abdomen demonstrate a long segment of small bowel wall thickening, and intense wall enhancement. (c) The degree of wall enhancement was equal to that of the renal parenchyma at the same vascular phase. Findings are compatible with severe disease.
When evaluating bowel wall enhancement, three factors should be taken into consideration: timing, intensity, and location. Acute disease typically presents with early, intense, and persistent enhancement. Chronic disease more typically presents with mild, delayed enhancement. Intensity of enhancement of bowel should be equal to that of the kidneys at the same vascular phase. Enhancement equivalent to or greater than renal cortex is abnormal and most often reflects the presence of inflammatory change.[6] It is also important to evaluate the location of bowel wall enhancement. Specifying whether enhancement is transmural versus limited to the mucosa allows one to differentiate active disease versus a chronic, or less acute process.
Small bowel disease
The early and late T2-weighted coronal images are important for the evaluation of small and large bowel disease. These images allow one to identify any areas of bowel wall thickening, or luminal narrowing, such as with strictures. If an abnormality is seen on the early images, it is important to re-assess the same area on the delayed images to confirm the findings. If the abnormality is not present on delayed images, the finding on the early images likely to represent a focus of peristalsis. Once an abnormality has been confirmed, evaluation of the post-contrast images is important to further characterize the abnormality. An area that demonstrates intense, early, persistent enhancement is likely to represent acute disease, whereas an area of slight enhancement seen only on the delayed images is likely to be a chronic process, such as stricture or fibrosing scar.
Case 1
Figure 5 illustrates a case of a young boy with known history of Crohn′s disease with normal upper GI and SBFT in 2008 [Figure 5a]. The patient also had another prior normal upper GI study in 2006. Despite these normal studies, the patient presented with multiple relapses and elevated upper ESR levels. An MRE was performed [Figures 5b–d] and it showed evidence of a persistently thick-walled loop of the distal small bowel, with enhancement similar to that of the renal cortex. The enhancement was seen on the arterial phase and was persistent on the delayed images. In addition, mesenteric inflammatory changes and adenopathy were also seen, suggesting acute disease. Although the small bowel follow through from 2008 was normal, mesenteric inflammatory changes, if present, would not have been picked up.

- Young boy with known history of Crohn's disease. (a) Small bowel follow through initially completed in 2008 was normal. Note there is no evidence of bowel wall thickening or separation of loops. (b) Coronal T2-weighted image from an MRE demonstrates moderate separation of loops with mesenteric adenopthy. (c) Coronal contrast enhanced T1-weighted image demonstrates a thick-walled loop of bowel with enhancement similar to that of (d) the renal cortex. This loop was unchanged on the delayed images, and findings were compatible with active Crohn's disease.
Terminal ileitis
Small bowel follow through examinations and CT studies are able to demonstrate terminal ileitis well, however with small bowel follow through studies, it can be difficult to determine the acuity of the process. Also, as noted above, extra-intestinal abnormalities are more often not picked up by small bowel follow through imaging.
Case 2
Figures 6a–c illustrate the CT and MRE findings of terminal ileitis. A CT scan was obtained when the patient initially presented with acute symptoms in the ED. At that time, contrast-enhanced CT (CECT) was completed to evaluate for acute appendicitis and demonstrated moderate wall thickening involving the terminal ileum. Moderate surrounding mesenteric inflammatory changes were also present with prominent mesenteric vessels, displaying the “comb sign.” The findings were compatible with acute terminal ileitis due to a Crohn′s disease flare. The patient was treated, and a follow up MRE was performed 3 months later to assess for change. MRE demonstrated terminal ileitis involving a similar length of bowel. Post-contrast images demonstrate that the wall enhancement is slightly less than that of the renal cortex, suggesting chronic rather than acute disease [Figures 6b and c].

- Young patient presenting with right lower quadrant pain. (a) A CT demonstrates moderate wall thickening involving the terminal ileum (arrowhead) and surrounding mesenteric inflammatory changes, displaying the “comb sign” (arrow). Three months after treatment follow-up MRE, (b) Coronal T1-weighted post-contrast MRE images demonstrated wall thickening involving a similar length segment of the terminal ileum as seen on the prior abdominal CT. The wall enhancement was slightly less than that of (c) the renal cortex suggesting findings are chronic rather than acute.
Abscesses and inflammatory masses
One of the major advantages of cross-sectional imaging in the evaluation of Crohn′s disease is the ability to evaluate for extra-intestinal abnormalities such as abscesses and inflammatory masses that may be missed on small bowel follow through studies.
Case 3
Figures 7a–c demonstrate a case of a patient with known history of Crohn′s (diagnosed initially by small bowel follow through) found to have an inflammatory mass by MRE. Initially, a small bowel follow through was done [Figure 7a]. This demonstrated narrowing and separation of the terminal ileum, consistent with Crohn′s disease. It is however difficult to ascertain if findings are acute or chronic based on small bowel follow through images alone. Again, the patient was treated. However, approximately 1 year later, patient presented again with symptoms. An MRE examination was completed. This demonstrated terminal ileitis with adjacent inflammatory mass [Figures 7b and c]. If a small bowel follow through study had been done again, this inflammatory mass would have likely not been identified. A follow up MRE completed 1 month after the start of treatment demonstrated resolution of terminal ileitis and the inflammatory mass.

- Patient with known history of Crohn's (a) Small bowel follow-demonstrates evidence of moderate terminal ileal wall thickening, compatible with terminal ileitis. (b) Coronal T2-weighted MRE image demonstrates terminal ileal wall thickening, in a similar pattern to that seen on prior small bowel study (arrow). In addition, a small collection was seen adjacent to this area of terminal ileitis (arrowhead). (c) Coronal contrast-enhanced MRE image demonstrates intense enhancement of the terminal ileum as well as this collection, compatible with active terminal ileitis and adjacent abscess.
Case 4
Figures 8a–d demonstrate a case of an 11-year-old patient with known history of Crohn′s disease presenting with persistent abdominal pain. Initially, a small bowel follow-through was performed. It demonstrated evidence of terminal ileitis [Figures 8a and b]. A contrast-enhanced CT was performed because of persistent pain. It again demonstrated evidence of terminal ileitis [Figure 8c]. The lack of surrounding inflammatory changes in the mesentery suggests findings are chronic rather than acute. Six months later, the patient presented with increased abdominal pain. At that time a second contrast enhanced CT was performed and it showed terminal ileitis as well as a focal abscess within the right lower quadrant [Figure 8d]. Of note, if a small bowel follow through had been repeated, this abscess would have been missed. Also, an MRE would have demonstrated the abscess without exposure to ionizing radiation.

- 11-year-old patient with known history of Crohn's disease. (a) Overhead and (b) Spot images from a small bowel follow through demonstrate evidence of terminal ileal wall thickening, with separation of bowel loops in that region. (c) A subsequent contrast-enhanced CT again demonstrates evidence of terminal ileitis. (d) A contrast enhanced CT of the abdomen completed 6 months later, demonstrates interval development of an abscess adjacent to an area of active terminal ileitis. Note the adjacent mesenteric inflammatory changes, not present on the prior CT.
Case 5
Figures 9a and 9b demonstrate a case of an abscess detected by MRE in a 14-year-old patient with known history of Crohn′s disease. The patient presented with severe lower abdominal pain. MRE was the initial examination completed, and demonstrated an abnormally configured collection of air adjacent to the terminal ileum [Figure 9a]. Axial images demonstrated an air fluid level in location of this collection [Figure 9b]. Post-contrast images showed rim enhancement surrounding this collection, compatible with an abscess [Figure 9c]. This extra-intestinal finding would have been missed on a small bowel follow through examination. In addition, a CT scan would have exposed this young patient to radiation.

- 14-year-old female with recent diagnosis of Crohn's disease. (a) Coronal T2-weighted images from an MRE demonstrate an abnormally configured collection of air adjacent to the region of the terminal ileum (arrowhead). (b) This collection is well appreciated on the axial T2-weighted images, which demonstrate an air fluid level in the collection (arrow). (c) Coronal T1-weighted post-contrast images demonstrate intense rim enhancement in this collection, compatible with an abscess.
Fistula formation
Case 6
A 12-year-old patient with history of Crohn′s disease underwent a small bowel follow through examination because of a concern about disease exacerbation. The small bowel follow through examination demonstrated at least two fistulae [Figure 10a]. Contrast-enhanced CT was also done and it demonstrated these fistulae between a thick-walled loop of small bowel and the colon [Figure 10b]. MRE was completed to further evaluate the extent of disease. Although both fistulae were also visualized by MRE, these could have been easily missed if prior fluoroscopic images were not available [Figures 10c–e].

- (a) SBFT demonstrates a fistula (circle) between a small bowel loop and distal colon (b) CECT of the abdomen, the corresponding fistulae (arrows) are seen within a thick-walled loop of small bowel and the colon. (c) Coronal T2-weighted images demonstrate the corresponding fistulae (arrows) are seen. At the time of this study, the small bowel wall thickening had resolved. (d) Early T2-weighted post-contrast images demonstrate mild enhancement of several small bowel loops. There is a linear area of enhancement (arrow) compatible with the known fistula. (e) Note that the level of renal enhancement is similar to that of the bowel wall enhancement, concerning for an acute process.
CONCLUSIONS
Magnetic resonance imaging and computed tomography are superior to flouroscopic examinations in their ability to evaluate extra-intenstinal disease, and are more accurate in the assessment of disease chronicity. Fluoroscopic examinations may be superior to MRE in the evaluation of fistulae; however, MRE may be used to follow up known fistulae. Magnetic resonance imaging is superior to computed tomography in that it is a radiation free exam and may allow a more accurate assessment of disease chronicity. Extra-enteric complications such as interloop abscesses, which may not be seen on fluoroscopic exams may also be followed by MRE, rather than subjecting patients to repeated CT radiation doses. MRE is a sensitive radiation-free exam for the evaluation of Crohn′s disease in the pediatric population.
ACKNOWLEDGMENTS
We would like to thank Mary Jo McMannis for her significant contributions to the development of the MRE protocol at University of Rochester Medical Center. In addition we would like to thank Katie Tower for her help with illustrations used in this paper, as well as Margaret Kowaluk for her tremendous help with the images.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/41/83399
REFERENCES
- Epidemiologic and clinical characteristics of children with newly diagnosed inflammatory bowel disease in wisconsin: A statewide population-based study. J Pediatr. 2003;143:525-31.
- [Google Scholar]
- Small bowel imaging - still a radiologic approach? Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2010;154:123-32.
- [Google Scholar]
- Radiation doses from small-bowel follow-through and abdominopelvic MDCT in crohn′s disease. AJR Am J Roentgenol. 2007;189:1015-22.
- [Google Scholar]
- Crohn disease of the small bowel: Comparison of CT enterography, MR enterography, and small bowel follow-through as diagnostic techniques. Radiology. 2209;251:751-61.
- [Google Scholar]
- MR imaging of the bowel: Pediatric applications. Magn Reson Imaging Clin N Am. 2008;16:467-78.
- [Google Scholar]
- Abdominal-Pelvic MRI (2nd Ed). NewYork (NY): Wiley Publishers; 2005.






