Linear Atelectasis around the Hilum on Chest Radiography: A Novel Sign of Early Lung Cancer
Address for correspondence: Dr. Kerem Ozturk, Department of Radiology, Uludag University Faculty of Medicine, Bursa, Turkey. E-mail: keremozturk@uludag.edu.tr
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Linear atelectasis is a focal area of subsegmental atelectasis with a linear shape. Linear atelectasis may occur as a consequence of subsegmental bronchial obstruction.
Aims:
We propose an early roentgen sign of obstructing lung tumors, namely perihilar linear atelectasis, and ascertain whether this phenomenon could be used as a sign to detect radiographically occult primary lung cancer.
Materials and Methods:
We performed a retrospective review of 45,000 posteroanterior chest radiographs to determine the frequency of appearance and characteristics of perihilar linear atelectasis. The perihilar region of chest radiographs was evaluated for the presence of linear atelectasis. When linear atelectasis was found, the total thickness was measured. Student's t-test was used to evaluate statistical significance, correlating the thickness of atelectasis and the presence of obstructing central primary lung cancer.
Results:
Perihilar linear atelectasis was demonstrated in 58 patients. Atelectasis was caused by an obstructing tumor in 21 (36%) cases and a variety of other conditions in 37 (64%) patients. A statistically significant relationship (P < 0.001) was observed between the dimension of perihilar linear atelectasis and primary lung cancer, with 16 of 19 patients with thick (>5.5 mm) perihilar linear atelectasis found to have primary lung cancer.
Conclusion:
Thick perihilar linear atelectasis is a new diagnostic roentgen sign that suggests subsegmental bronchial obstruction. In this patient subgroup, who are otherwise asymptomatic, a persistent linear atelectasis can be due to primary lung cancer.
Keywords
Pulmonary atelectasis
thoracic radiography
spiral computed tomography

INTRODUCTION
Linear atelectasis is a focal area of subsegmental atelectasis with a linear shape. It is normally horizontal and sometimes oblique or perpendicular. Linear atelectasis may occur as a consequence of obstruction in the bronchus of a pulmonary subsegment. The collapsed lung tissue could be flattened, and it may be seen as a relatively thick, well-demarcated, linear opacity.[1]
To the best of our knowledge, linear atelectasis, especially located in the lower lung parenchyma, has usually been observed in simple hypoventilatory changes (i.e., the lung folding in on itself) in addition to some benign conditions such as pulmonary embolism or pneumonia or following aspiration.[2] Nevertheless, the linear focal atelectatic changes in perihilar lung parenchyma have not been reported to be associated with primary lung cancer.
In this study, we propose to describe an early roentgen finding of obstructing tumors, namely thick perihilar linear atelectasis, and ascertain whether this phenomenon could be used as a sign to detect radiographically occult primary lung cancer.
MATERIALS AND METHODS
Subjects
The Institutional Review Board approved this retrospectively designed study. Between May 2012 and December 2016, 45,000 patients with posteroanterior (PA) chest radiographs for routine chest imaging were retrieved from the radiology database. Lateral chest radiographs were not gathered routinely in our department and ordered by the clinicians who initially encountered the pathological findings on the radiographs. The perihilar region of the lung parenchyma on chest radiographs was evaluated for the presence of linear atelectasis. Among them, 58 patients (0.012%) demonstrated perihilar linear atelectasis on PA chest radiographs that were selected for investigation.
Our exclusion criteria were poor image quality; patients with known lung cancer and apparent mass lesion on the chest X-ray resembling lung cancer, prior lung surgery or radiation therapy affecting the perihilar region; and patients without consecutive chest X-ray or thorax computed tomography (CT) for follow-up.
The qualitative assessment of the images without knowledge of the final causes was performed. The following factors were also evaluated quantitatively on PA chest radiographs: The localization and maximum diameter of atelectasis.
Clinical findings and the cigarette smoking status of the patients with linear atelectases were acquired from the hospital database.
For the chest radiographs, the following findings were also recorded: narrowing or cutoff of the bronchus, pleural effusion, bronchiectasis, nodule and evidence of mediastinal lymphadenopathy. A decision was made as to whether the findings were suggestive of atelectasis produced by an obstructing tumor.
Patients with suspected lung cancer on plain radiographs underwent complete diagnostic procedures, including CT of the chest and/or fiberoptic bronchoscopy if needed.
If atelectasis was detected, follow-up chest radiographs of these patients were excluded to obviate sampling bias. In addition, our patients were not admitted to our clinic through the cancer screening program.
Imaging technique
All chest PA radiographs consisted of a PA view and were obtained using equipment (Samsung, GE080) with a high kilovolt potential (i.e., 110–150 kVp) at a tube-to-receiver distance of 180 cm and with a high grid ratio.
CT scans were obtained with a multidetector row scanner equipped with 128 detector rows (SOMATOM Definition, Siemens Medical Solutions, Forchheim, Germany). On the scanner, after obtaining a scout view, examinations were completed by a helical scan of lungs from the apex to the end of the adrenal glands, which was a routine protocol in our department for chest CT examinations. From the raw data of each acquisition, contiguous 5-mm thick axial slices were obtained using reconstruction algorithms for both lung and mediastinal windows. CT examinations were obtained routinely without intravenous contrast material otherwise indicated.
Image analysis
PA roentgen images were independently evaluated for the identification of perihilar linear atelectasis by board-certified chest radiologists in a blinded manner. Perihilar linear atelectasis was recorded as negative or positive on PA chest radiograph with additional concurrent pathologies. In addition, the diameter and perihilar localization of atelectasis was further recorded. The location of perihilar atelectasis and concurrent primary lung cancers were confirmed by CT imaging, bronchoscopic findings, and surgical reports. All readers were blinded to the prior results of chest radiographs as well as to the results obtained from any other diagnostic technique. If a lesion was not mentioned in the original radiologic report by a radiologist, it was considered visible but not detected.
Quantitative analysis
The diameter of each linear atelectasis was calculated as the diameter greatest in dimension, mostly acquired on the craniocaudal plane of PA radiographs and its distance from the cardiac border was determined as a minimum 1 cm to not include any hilar vascular structures or lymph nodes [Figure 1].
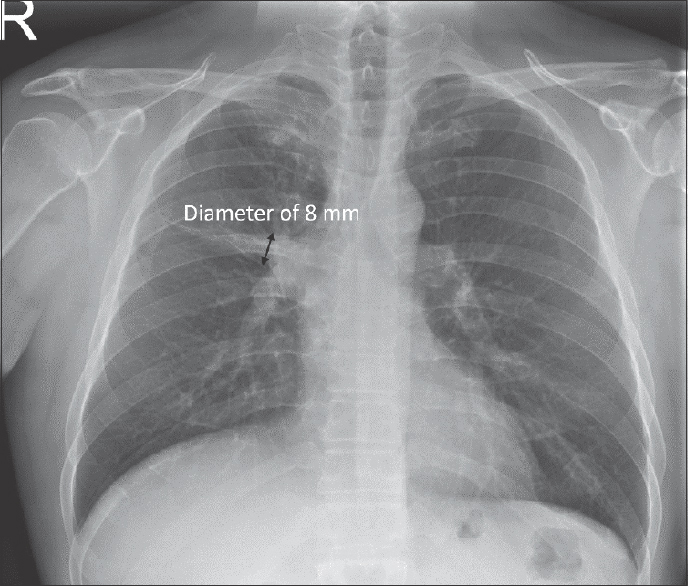
- Diameter of perihilar linear atelectasis acquired on craniocaudal plane on posteroanterior radiograph.
The distribution of the perihilar linear atelectases was localized as follows: perihilum near the superior vena cava (SVC), perihilum near the right atrium and left-sided perihilum [Figure 2].
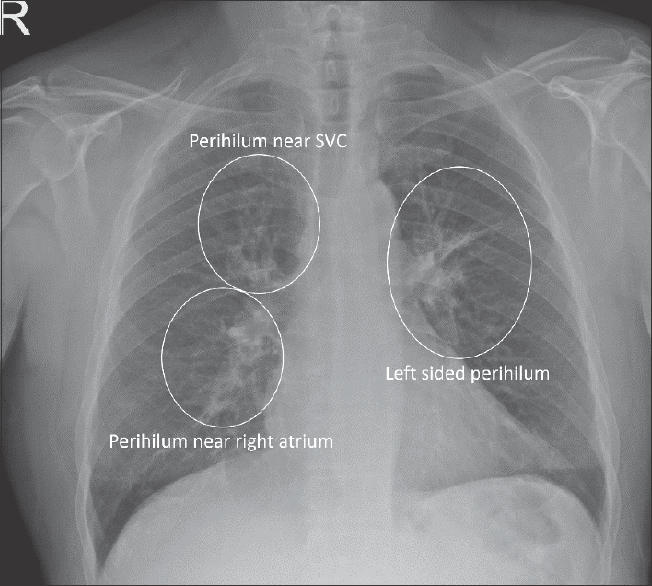
- The distribution of perihilar linear atelectasis was categorized as perihilum near superior vena cava, perihilum near right atrium and left-sided perihilum.
Statistical analysis
All statistical comparisons between the linear atelectases with or without concurrent central primary lung cancers were performed using Statistical Package for the Social Sciences software (SPSS, version 23.0; SPSS, Chicago, IL, USA). Receiver operating characteristics (ROC) analysis was performed using an analysis program (MedCalc for Windows, Ostend, Belgium). Descriptive statistics are given as the mean ± standard deviation (SD) for continuous variables and the count with the percentage for categorical variables. Gender was compared using Pearson's Chi-square test, and Student's t-test was used for the patients’ ages.
The association of perihilar linear atelectasis with primary lung cancers was estimated with Pearson's Chi-square test. ROC analysis was utilized to assess the optimal cutoff value for linear atelectasis with the best differentiation scores (minimal false-negative and false-positive results) between the two groups. To determine whether there was any difference in atelectasis thickness between perihilar linear atelectasis produced by centrally located lung tumors and benign conditions, an independent t-test was performed. P < 0.05 was considered statistically significant.
RESULTS
Perihilar linear atelectasis was observed in 58 (0.012%) patients. Atelectasis was caused by an obstructing tumor in 21 (36%) patients [Figure 3] and a variety of other benign conditions in 37 (64%) patients [Figure 4 and Table 1].
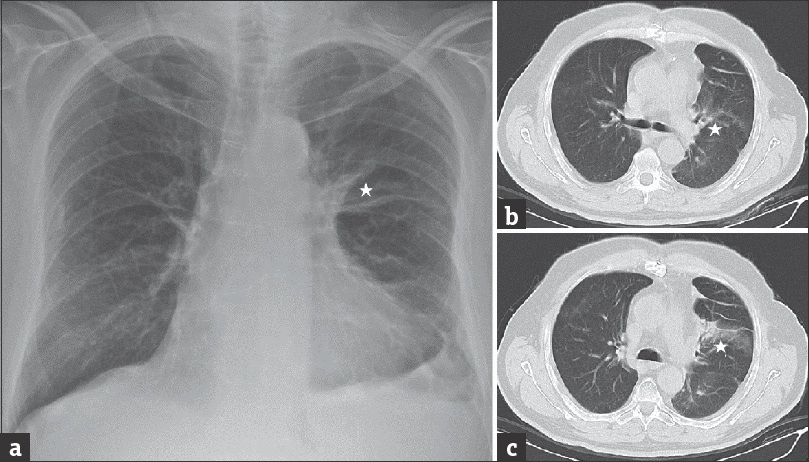
- Left, (a) chest radiograph with left-sided perihilar linear atelectasis (asterisk) was caused by central bronchogenic carcinoma. Right, (b and c) computed tomography confirmed the linear atelectasis (asterisk) and also identified obstructing bronchogenic carcinoma.
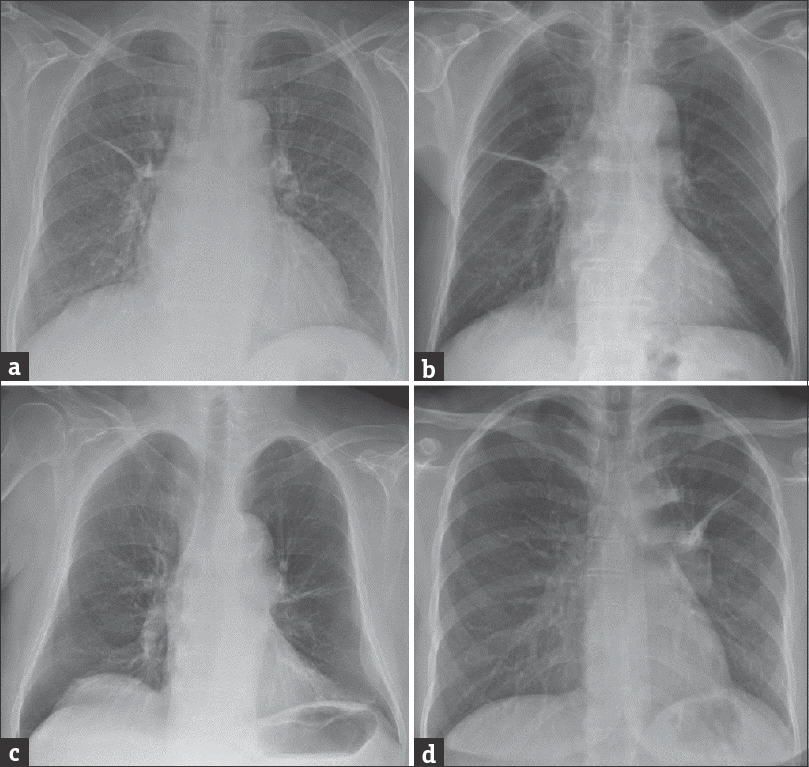
- (a-d) Posteroanterior chest radiographs demonstrate perihilar linear atelectasis was caused by variety of benign conditions.
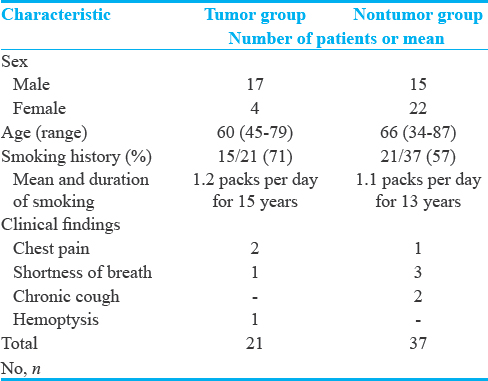
Age and sex in atelectasis with or without concurrent central primary lung cancer: The mean age was 60.14 ± 9.26 years (range, 45–79 years) in the group with tumor and 65.73 ± 12.65 years (range, 34–87 years) in the group without concurrent tumor. There was no significant difference between the groups (P = 0.228). The group with tumor (female-to-male ratio: 4/17) and the group without tumor (female-to-male ratio: 22/15) were significantly different according to gender (P = 0.003) [Table 1].
Smoking history in patients with linear atelectasis: Fifteen out of 21 (71%) patients with primary lung cancers were smoked cigarettes, at a mean of 1.2 packs per day for 15 years (mean: 15.2 years; SD: ±4 years), and 21 out of 37 (57%) patients without tumors smoked cigarettes, at a mean of 1.1 packs per day for 13 years (mean: 13.3; SD: ±3.5 years). There was no significant difference between the groups (P = 0.315) [Table 1].
Three patients with linear atelectasis were found to have chest pain, four patients had shortness of breath, two patients presented with chronic cough, and one patient presented with hemoptysis as a symptom when the chest roentgenograms were acquired. There was no significant difference between the groups with or without lung cancer for the initial symptoms when the chest roentgenograms were acquired (P = 0.171) [Table 1].
None of the patients with linear atelectasis had associated ancillary findings of lung cancer on chest radiographs including narrowing or cutoff of the bronchus, pleural effusion, nodule, bronchiectasis, and evidence of mediastinal lymphadenopathy.
Craniocaudal dimensions of the atelectasis
The mean diameter of linear atelectasis was 6.95 (range: 2.5, 13.6) (SD: ±2.69) mm in the tumor group and 4.12 (range: 1.7, 7.8) (SD: ± 1.23) mm in the nontumor group. There was a statistically significant difference in diameter between the groups (P < 0.001) [Figure 5].
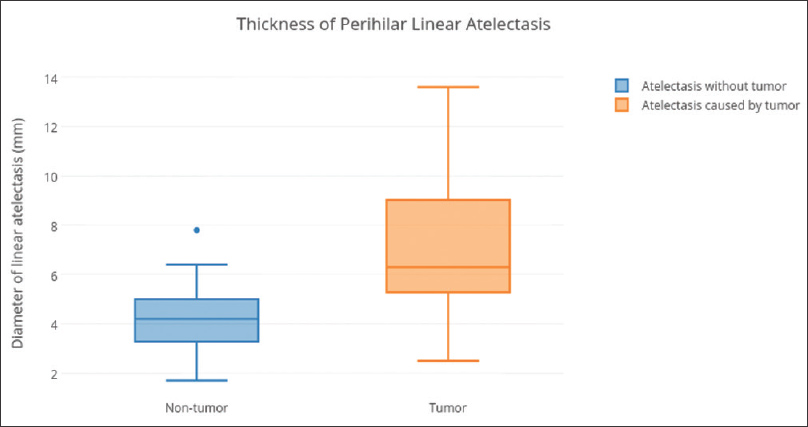
- Thickness of perihilar linear atelectasis was compared between the atelectasis caused by bronchogenic carcinoma or benign conditions.
Localization of atelectasis
The distribution of perihilar linear atelectasis was as follows: perihilum near the SVC, 54%; perihilum near the right atrium, 7%; and left perihilum, 39%. There was no significant difference between right- and left-sided lesions (P = 0.872).
Receiver operating characteristics analysis
The area under the ROC curve for the differentiation of atelectasis with or without concurrent primary lung cancer was 0.838 (95% confidence interval: 0.720, 0.956) according to the diameter of the linear atelectasis, and it was extracted for the optimal cutoff values by two readers in combination. According to the acquired optimal cutoff value, an atelectasis with a craniocaudal dimension >5.5 mm was considered to be caused by a central obstructing lung tumor.
The final diagnosis of the confirmed tumors was obtained by means of the following methods: histopathological examination of primary tumors by biopsy or thoracotomy in 15 patients and by bronchoscopy with histopathological examination in six patients.
Histopathological examination of the biopsy specimens found squamous cell carcinoma in fifteen patients, small cell lung cancer in five patients and carcinoid tumor in one patient.
Thirty-seven patients had other causes of perihilar linear atelectasis, including postoperative (five patients with abdominal surgery) or posttraumatic atelectasis (three patients) in eight; pneumonia or other acute airspace disease in five; compression caused by pleural effusion in three; bronchiectasis in three; radiation fibrosis (patients who had radiation therapy for the head and neck tumors involving infrahyoid neck region) in two; and other benign conditions in sixteen patients.
In four (18%) of the 21 patients, a centrally located lung tumor was missed on consecutive chest radiographs, and in two (10%) patients, the tumor was missed more than twice on routine chest roentgenogram. Superposing structures were more frequently present in radiographs with missed lesions, and the diameter of the atelectasis was smaller.
CT successfully detected the five missed carcinomas and confirmed obstructing tumors in the remaining 15 cases, giving a correct diagnosis in 95% of the cases in which the cause of atelectasis was unknown. Only one obstructing lung tumor which was related to linear atelectasis was missed on chest CT examination. Consecutive bronchoscopic examination revealed the primary obstructing lung tumor as a cause of linear atelectasis.
CT allowed the location of the bronchial lesion, the length of which ranged from a few centimeters to 3 cm in the greatest dimension in 20 cases (20/21). The appearance of the tumor was polypoid in 16 cases, nodular in three cases, and superficial in one case.
DISCUSSION
Primary lung cancers tend to originate from the bronchial walls and sometimes constitute a bronchial obstruction and may manifest radiographically as an atelectasis.[3] In the alveoli distal to the obstruction, the air could be trapped, leading to the appearance of obstructive atelectasis. Atelectatic changes in the tributary lung distal to the bronchial obstruction are relatively common abnormal radiographic findings in adults with obstructing tumors.
As atelectasis occurs following bronchial or bronchiolar obstruction, normal lung tissue with elastic features immediately above and below the atelectasis becomes emphysematous and permits collapse to occur in a horizontal direction. These focal linear atelectatic changes are usually found in the lower third of the lung fields, either unilaterally or bilaterally.[45] Most frequently, it is seen immediately above the diaphragm and always secondary to some other lesion, either intrathoracic or intra-abdominal.[67] Nevertheless, even after a decade, many radiologists and clinicians fail to utilize this important diagnostic finding of obstructing primary lung cancer to the best advantage. The focal atelectatic changes distal to the obstruction may be seen when some of the smaller pulmonary bronchi are occluded. The resulting areas of focal changes, such as linear atelectasis, may be suggestive of a diagnosis of occult lung cancers on the chest roentgenograms.
The diagnosis of central lung tumors is often difficult to establish on chest roentgenogram, especially when the tumor is small and obscured by the hilar structures.[8] The detection of radiographically occult lung cancer was made possible by the appearance of various radiologic findings.[9] Narrowing of the affected bronchi or focal bulging of the fissure bordering the collapsed lobe have been described in the literature[10] and could be identified rarely in chest radiographs of obstructive atelectasis. Identifying such roentgen findings, including signs of perihilar linear atelectasis, could be viewed as synonymous with taking the opportunity to make an early diagnosis of primary lung cancer. Nearly two-thirds of patients with primary lung cancer, which was difficult to detect by chest radiograph, were found to have early lung cancer. Because the survival rates of early bronchogenic cancers following resection are much higher than those of advanced stage, the effect of the recognition and detection of these roentgen findings are indeed substantial.[1112]
The propensity for bronchogenic cancer to cause atelectasis by occluding central bronchi has been studied previously. Byrd et al.[13] reviewed the initial chest radiographs of 114 patients with bronchogenic lung cancer, finding 76% of these patients had a hilar mass and 30% had signs of bronchial obstruction such as volume loss, consolidation, or obstructive pneumonitis. Chute et al.[14] found that 79% of 326 patients with small cell lung cancer presented with hilar or mediastinal involvement and that 35% had some degree of atelectasis.
Chest radiography may be an excellent diagnostic tool for showing segmental or lobar atelectasis and can be used to document central tumors as the cause of atelectasis on the basis of two major findings: evidence of a central hilar mass and evidence of perihilar thick linear atelectasis. Using both findings as plain film signs, the chest radiograph may identify atelectasis with a low false-positive rate. However, the chest radiograph is generally less sensitive than CT, indicating that in some cases, the chest radiograph cannot be used to determine if a central tumor is the cause of atelectasis.[15]
CT is able to diagnose obstructing tumors as a cause of atelectasis with an acceptable false-positive rate. In patients with postoperative acute atelectasis, clinically documented pneumonia or obstructive gross tumors on chest roentgenograms, the cause of atelectasis usually does not represent the diagnostic difficulty.[16] However, the demonstration of the pathologic cause of obstructive atelectasis in the absence of these findings may be a problem. Recent studies demonstrated that the bronchial patency and absence of a centrally located mass lesion on CT are reliable imaging findings that can be used to exclude primary lung cancers as a cause of atelectasis.[1718]
In general, the detection of hilar cancer is difficult due to the presence of variations in the anatomy of the hilar region.[19] In a screening program, Muhm et al.[20] found that 65% of lung cancers arising in the hilum were missed. In our study, lesions were skipped once in the chest roentgenogram of three patients. In one of these patients, the lesion showed little progress over a few years. The radiologist interpreted the lesions as benign linear atelectasis and did not express any suspicion of a possible tumoral lesion.
We retrospectively estimate that this 28% miss rate, which is detected in patients having perihilar linear atelectasis on chest radiograph, can be improved with the contribution of our results to the literature. The detection of early stage lung cancers may have a major impact on prognosis. Therefore, we think that chest radiographs with perihilar linear atelectasis need to be further evaluated by CT or bronchoscopy in high-risk groups.
We believe our study has some advantages. Our method of measuring linear atelectasis with quantitative assessment seems to be more objective and easy to interpolate in daily radiology practice.
Our study was retrospective, and as a result, there were some inherent limitations. The retrospective nature of the study hindered us from accurately registering the number of linear atelectasis on chest radiographs, and thus, the exact analysis of the accuracy of perihilar linear atelectasis could not have been determined. A plan to conduct a prospective study is needed to answer the following important questions: What is the prevalence of perihilar linear atelectasis? What are the sensitivity and specificity of screening using perihilar linear atelectasis?
CONCLUSION
To the best of our knowledge, no studies have been reported to address the association of perihilar linear atelectasis on chest radiography with the detection of early-form centrally located lung cancer in clinical practice. Thick perihilar linear atelectasis is a new diagnostic roentgen sign that could be suggestive of a diagnosis of primary lung cancer.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/27/237278
REFERENCES
- Diagnosis of chronic obstructive pulmonary disease in lung cancer screening computed tomography scans: Independent contribution of emphysema, air trapping and bronchial wall thickening. Respir Res. 2013;14:59.
- [Google Scholar]
- Fleischner society: Glossary of terms for thoracic imaging. Radiology. 2008;246:697-722.
- [Google Scholar]
- Atelectasis: Mechanisms, diagnosis and management. Paediatr Respir Rev. 2000;1:274-8.
- [Google Scholar]
- Radiographic manifestations of lobar atelectasis. J Thorac Imaging. 1996;11:109-44.
- [Google Scholar]
- Miss rate of lung cancer on the chest radiograph in clinical practice. Chest. 1999;115:720-4.
- [Google Scholar]
- Differentiation of central lung tumor from postobstructive lobar collapse by rapid sequence computed tomography. J Thorac Imaging. 1991;6:28-31.
- [Google Scholar]
- Early mortality after surgical resection for lung cancer: An analysis of the English national lung cancer audit. Thorax. 2013;68:826-34.
- [Google Scholar]
- Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24(Suppl 6):vi89-98.
- [Google Scholar]
- Radiographic abnormalities in carcinoma of the lung as related to histological cell type. Thorax. 1969;24:573-5.
- [Google Scholar]
- Presenting conditions of 1539 population-based lung cancer patients by cell type and stage in New Hampshire and Vermont. Cancer. 1985;56:2107-11.
- [Google Scholar]
- Detection of early-stage lung cancer: Computed tomographic scan or chest radiograph? J Thorac Cardiovasc Surg. 2001;121:1053-7.
- [Google Scholar]
- Tumors in the tracheobronchial tree: CT and FDG PET features. Radiographics. 2009;29:55-71.
- [Google Scholar]
- Computed tomography of lobar collapse: 1. Endobronchial obstruction. J Comput Assist Tomogr. 1983;7:745-57.
- [Google Scholar]
- Computed tomography of lobar collapse: 2. Collapse in the absence of endobronchial obstruction. J Comput Assist Tomogr. 1983;7:758-67.
- [Google Scholar]
- Early hilar lung cancer – Clinical aspects and long term survival. Identification of a subgroup of stage IA patients with more favorable prognosis. Lung Cancer. 2000;27:119-24.
- [Google Scholar]
- Lung cancer detected during a screening program using four-month chest radiographs. Radiology. 1983;148:609-15.
- [Google Scholar]






