Translate this page into:
“Knot Stent”: An Unusual Cause of Acute Renal Failure in Solitary Kidney
Address for correspondence: Dr. Moufid Kamal, Residence Dream Garden; Villa no. 52; Sidi Abderrahman La corniche, Casablanca, Morocco. E-mail: monsieurmoufid@yahoo.fr
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
The insertion of indwelling ureteric stents is a routine procedure in urology practice. Complications secondary to the insertion of these stents have also increased, such as stent encrustation, stent fragmentation, stone formation, and recurrent urinary tract infections. Knot formation within the renal pelvis or in the coiled portion of the ureteral stent is an extremely rare condition, with less than 15 cases reported in literature. The authors report a rare case of knotted stent, complicated by an obstructive acute renal failure and urosepsis, in a patient with a solitary functioning kidney.
Keywords
Knot
renal failure
solitary kidney
ureteral stent
urosepsis
INTRODUCTION

Ureteral stents are widely used in urology practice. Because of their widespread use, complications secondary to stent placement have also increased, such as stent encrustation, stent fragmentation, stone formation, and recurrent urinary tract infections. Knot formation within the body or coiled portion of the ureteral stent is an extremely rare condition, with less than 15 cases reported in the literature.[1] Nevertheless, this condition may lead to legal and medical problems for urologists, health institutions, and also for patients. The authors report a rare case of knotted stent (KS) complicated by an obstructive acute renal failure and urosepsis, in a 32-year-old man with a solitary functioning kidney.
CASE REPORT
A 32-year-old male with solitary left functioning kidney was admitted with complaints of lumbar pain, which radiated to the groin, burning urination, fever, and moderate dyspnea that had persisted for 2 days. Prior to this presentation patient had under gone ureteroscopy for the treatment of ureteral stone, following which ureteral stent was left in place. Laboratory findings on admission showed the following: serum creatinine 44 mg/dL, blood urea nitrogen 14.7 mg/dL, hemoglobin level of 10 g/dL, C-reactive protein 95 mg/L, and total white blood cell count of 14000/mm3 with 88% polymorphs. Diuresis was 400 mL/24 h and dyspnea was ameliorated by nasal oxygen administration.
Plain-film radiograph of abdomen revealed entire double J stent coiled in the left renal pelvis. In our institution the double J stent is placed under endoscopic and fluoroscopic monitoring. The urologist and the surgical report, of the previous ureteroscopy, confirmed that the stent was placed without problem after ureteroscopy. KUB X-ray performed after the insertion of the stent confirmed its good placement. Renal ultrasonography revealed moderate hydronephrosis with hyperechoic intrapelvic stent. The patient was admitted with a diagnosis of oliguric acute renal failure and urosepsis due to obstructive KS.
A 7-F ureteral catheter was inserted, under local anesthesia, to relieve the renal obstruction [Figure 1]. After 3 days, the urosepsis was relieved with drainage and antibiotic therapy, and the patient recovered from the acute renal failure with serum creatinine of 1.8 mg/dL and , blood urea nitrogen 20.7 mg/dL. When the patient was stable, ureteroscopy was performed. Under spinal anesthesia, in the rigid ureteroscopy position, the right lower limb was kept in the lithotomy position, and the left limb bent in the lowest position. A hydrophilic guidewire was inserted in the ureteral catheter and coiled in the renal pelvis. An 8-F rigid ureteroscope was advanced beside the guidewire through urethra, bladder, and then the left ureter. The double-J stent was found in the proximal ureter. The stent end was grasped with a basket and progressively extracted under fluoroscopic guidance. When the stent knot had reached the proximal ureter, there was a slight resistance. By gentle continuous traction, the knot was slowly pulled through the ureter until complete stent was removed. Retrograde ureterography at the end of the maneuver excluded any ureteral injury. A 7-F ureteral catheter was inserted on the guidewire until it was in the renal pelvis. On the fourth postoperative day, the ureteral catheter was removed.
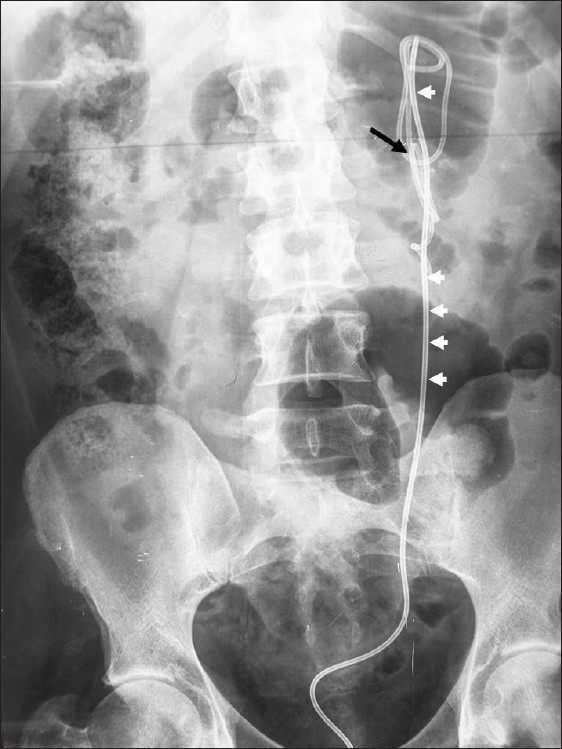
- A plain X-ray film of the abdomen shows the original coiled JJ stent with formation of a complete knot (black arrow). An additional ureteral stent was inserted for rapid decompression of infected solitary kidney (white arrowhead).
The postoperative period was uneventful and prompt recovery was noted.
DISCUSSION
The first report on the KS in literature was by Groeneveld in 1989.[1] Sometimes, the stent may knot inside the ureter, representing a therapeutic challenge with the potential risk of ureteral avulsion. Conservative retrieval remains difficult in patients with solitary kidney, ureteric implantation, or uretero-intestinal anastomosis. KS can occur at any age: Corbett et al.,[2] and Flam et al.,[3] reported two cases a 4-year-old and 86-year-old patient, respectively. According to literature, the male to female ratio is 3:2. Many different ureteral stent configurations are available, including single -J, double-J, and multi-length stents. Some authors have hypothesized that excessive length stent, as well as, coil configuration increase the likelihood of knot formation.[124] Most of these knots involve the proximal end of the stent near the coil, but any part of the stent can be involved. Quek et al.,[4] reported a case in which the knot was formed in the middle of the stent while Eisner et al.[5] depicted a patient who had knots in two separate indwelling stents. KS comes to notice when the patient's symptoms reappear, during incidental imaging, or acute renal function with urosepsis, like in our patient.
Given the potential morbidity of both percutaneous and open procedure, we opted for a retrograde ureteroscopy after initial placement of retrograde ureteral catheter, to achieve adequate urinary drainage, and antibiotic therapy for urosepsis. Flam et al.,[3] after failure of ureteroscopic extraction at initial attempt, inserted a second ureteral stent alongside the KS to allow the passage of a 9.5F ureteroscope 1 week later.
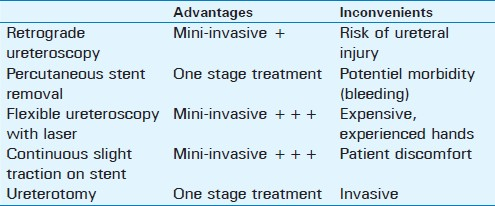
No guidelines exist for successful management of KS.[4–6] Various methods of treatment like combinations of retrograde ureteroscopy, percutaneous removal, and open surgery have been used for retrieval of these knotted stents.[13–7] Table 1 summarizes the main advantages and inconvenient disadvantages of each technique. The standard clinical approach to management of KS is ureteroscopic removal when it is feasible with simple, gentle traction, both under direct vision and fluoroscopy. This traction can be immediate or delayed after initial placement of ureteral stent to promote dilation of the ureter below the KS for two or three days.[3] The occurrence of resistance to moderate traction during ureteroscopy or hematuria requires stopping the maneuver to avoid ureteral injury. Sometimes, traction on the KS worsens the prognosis, making the knot tighter. Baldwin et al.,[6] used simple traction with guide wire assistance. Kundargi et al.,[7] and Braslis et al.,[8] achieved successful percutaneous extraction of dysfunctioning stent while Sighinolfi et al.,[9] used 3 days of continuous staged traction on the stent tied at the leg with a common catheter strip at the distant coil allowing its spontaneous expulsion. Richards et al.,[10] report the successful use of flexible ureteroscopy with Holmium laser in treating a case of a retained Double J stent. In this case, the laser was found helpful in breaking the center of the knot and removing the stent in two pieces. Failure of mini-invasive approach results in open removal. In our patient, due to potential morbidity related to percutaneous approach, we chose the retrograde approach, both to treat obstruction of the urine flow and to promote ureteral dilation in a poorly compliant patient. Retrograde approach is less invasive and has a lower risk of bleeding compared with percutaneous surgery.
Prevention remains the most important priority in the fight against complications. The close follow-up of stented patients is valuable for the early detection of morbidity or complications. Ureteric stent monitoring is essential and should include regular monthly urine cultures, monitoring of serum creatinine levels, and X-ray KUB.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/36/97758
REFERENCES
- A knotted ureteral stent: A case report and review of the literature. Urol Ann. 2010;2:80-2.
- [Google Scholar]
- Knotting of a double pigtail stent within the ureter: An initial report. J Urol. 1995;154:1858-9.
- [Google Scholar]
- Knot formation at the mid portion of an indwelling ureteral stent. J Urol. 2002;168:1497.
- [Google Scholar]
- Repeat knot formation in a patient with an indwelling ureteral stent. Int Braz J Urol. 2006;32:308-9.
- [Google Scholar]
- Knotted ureteral stent: A minimally invasive technique for removal. J Urol. 1998;159:2065-6.
- [Google Scholar]
- Knotted upper end: A new complication in the use of an indwelling ureteral stent. J Urol. 1994;151:995-6.
- [Google Scholar]
- Spontaneous knotting of a pigtail ureteric stent in the ureter requiring percutaneous removal. Aust N Z J Surg. 1992;62:825-6.
- [Google Scholar]
- A knotted multi-length ureteral stent: A rare complication. Urol Res. 2005;33:70-1.
- [Google Scholar]
- Successful treatment of stent knot in the proximal ureter using ureteroscopy and holmium laser. Case Report Med. 2011;2011:50219.
- [Google Scholar]






