Translate this page into:
Immediate effect of upright position on lumbar disc using multiposture MRI: Preliminary results

*Corresponding author: Tosiaki Miyati, Faculty of Health Sciences, Institute of Medical, Pharmaceutical and Health Sciences, Kanazawa University, Kanazawa, Japan. ramiyati@mhs.mp.kanazawa-u.ac.jp
-
Received: ,
Accepted: ,
How to cite this article: Furihata K, Miyati T, Ohno N, Kobayashi S. Immediate effect of upright position on lumbar disc using multiposture MRI: Preliminary results. J Clin Imaging Sci. 2024;14:12. doi: 10.25259/JCIS_11_2024
Abstract
Objectives:
Gravity loading on lumbar intervertebral discs (IVDs) is affected by body position. Although the long-term effects of gravity on IVDs have been reported, the immediate effects of gravity on IVDs remain unclear. We considered that changes in IVD structure in the upright and supine positions provided new diagnostic information. Therefore, we compared the apparent diffusion coefficient (ADC), transverse relaxation time (T2), and morphology of the lumbar spine between the quickly changing upright and supine positions using an original magnetic resonance imaging (MRI) system that can obtain images in any position (multiposture MRI).
Material and Methods:
On a 0.4-T multiposture MRI, diffusion-weighted images of the lumbar spine in seven healthy volunteers were obtained using single-shot diffusion echo-planar imaging (b = 0 and 600 s/mm2) in quickly changing upright and supine positions. Moreover, spin-echo images with multiple echo times (echo time = 30, 60, 90, and 120 ms) were obtained in each position. We calculated the ADC and T2 of each IVD (L1 and S1) without any disc degeneration. In addition, the lumbar lordosis angle and length of the lumbar spine were measured to evaluate the morphology of the lumbar spine.
Results:
The T2 of the IVD between L4 and L5 in the upright position was significantly lower than that in the supine position (P < 0.05). No significant differences were observed in the ADC. The morphology of the lumbar spine did not differ significantly between the two positions.
Conclusion:
The T2 of the IVD between L4 and L5 was likely decreased by the effect of gravity due to the postural change from supine to upright.
Keywords
Multiposture MRI
Magnetic resonance imaging
Gravity effects
Spine
Intervertebral discs
INTRODUCTION
Lumbar intervertebral discs (IVDs) are affected by gravity. The previous studies have reported changes in the shape and composition of IVDs before and after diurnal activity under gravity loading.[1,2] In addition, studies have reported that the length of IVDs becomes shorter during the daytime and that a decrease in height occurs during the first hour after rising.[3,4] These studies revealed the long-term effects of gravity loading during the daytime in upright and sitting positions. Although the long-term effects of gravity loading on IVDs have been reported, their immediate effects remain unclear. We considered that changes in IVD structure in the upright and supine positions provided new diagnostic information.
Magnetic resonance imaging (MRI) is highly sensitive to tissue water content and is therefore a useful tool for assessing IVDs. In particular, functional information such as transverse relaxation time (T2) and apparent diffusion coefficient (ADC) is used to assess the degeneration of IVDs.[5-7] Using conventional MRI systems, functional information in the standing or sitting position is limited because subjects can only be examined in the supine position. Although some MRI systems are capable of imaging in the standing position, many studies are limited to the evaluation of morphology only.[8,9] In other words, there have been no reports of morphological and functional evaluation of the lumbar spine in the standing and supine positions. To overcome this limitation, we developed an original MRI system called “multiposture MRI” by improving an existing MRI system using a 0.4-T permanent magnet, enabling us to perform MRI examinations in different positions.[10,11] As a preliminary study to elucidate the effects of gravity on the lumbar spine, we evaluated the ADC, T2, and morphology of the lumbar spine before and after a postural change from a supine to an upright position using multiposture MRI.
MATERIAL AND METHODS
Subjects and study design
This study included seven healthy male volunteers with no known history of back pain or spine disease (mean age, 23.7 ± 2.7 years) with a mean weight and height of 59.9 ± 5.0 kg and 172.6 ± 3.6 cm, respectively.
The study was conducted in the morning, as it is well known that the spine becomes shorter during the daytime and recovers during the night.[2,3]. To perform the study after full recovery of the IVDs from compression, the subjects were kept in the supine position for 8 h before image acquisition except for the time to defecation. No restrictions were imposed on the supine posture (e.g., supine and prone).
To avoid loading the intervertebral discs during imaging, imaging was performed in the supine and upright positions.
Multiposture MRI
Our laboratory developed an original MRI system called multiposture MRI [Figure 1] by improving an existing MRI system using a 0.4-T permanent magnet, enabling us to perform whole-body MRI examinations in different positions.[10,11]
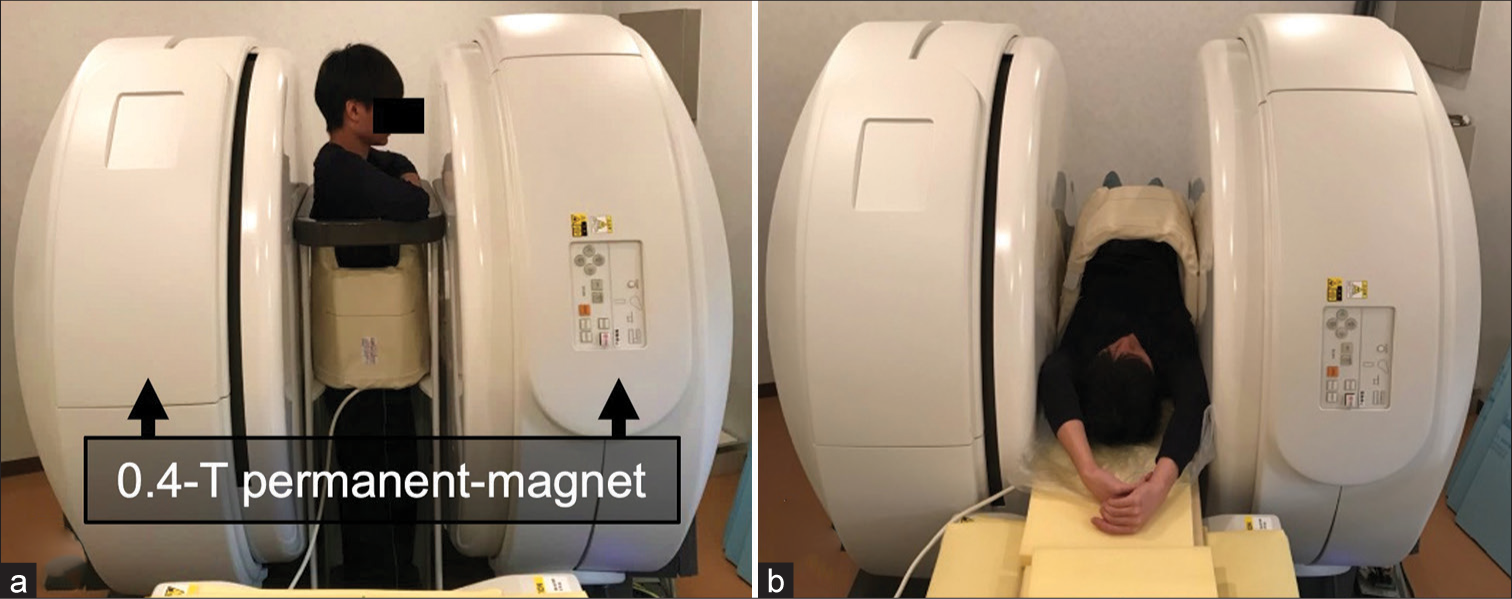
- Multiposture magnetic resonance imaging using a pair of 0.4-T permanent magnets in (a) upright position and (b) supine position.
Image acquisition and analytical procedure
The multiposture MRI system was used to obtain midsagittal diffusion-weighted images of the lumbar spine in quickly changing upright and supine positions in seven healthy volunteers by single-shot diffusion echo-planar imaging (b = 0 and 600 s/mm2) with a QD Flexible Body coil (M) made by HITACHI, JAPAN [Figure 1]. Other imaging parameters were repetition time = 5000 ms, echo time = 123.7 ms, flip angle = 90°, slice thickness = 7 mm, imaging matrix = 64 × 128, field of view = 280 × 280 mm, echo train length = 72, number of signals averaged = 16, and total scan time = 5 min and 30s. In addition, midsagittal spin-echo images with multiple echo times (TE) were obtained in each position using the following parameters: Repetition time = 2500 ms, echo time = 30–120 ms (30 ms × 4 echoes), flip angle = 90°, slice thickness = 7 mm, imaging matrix = 256 × 160, field of view = 280 × 280 mm, number of signals averaged = 1, and total scan time = 6 min and 19s.
Next, we calculated the ADC and T2 for each IVD at levels from L1 to S1, excluding those with disc degeneration. Grades I and II in the Pfirrmann grading system were defined as IVDs without disc degeneration.[12] IVD grading was confirmed by a radiologist with 32 years of experience in radiology. To determine the signal intensities of the IVDs, we manually placed regions of interest (ROIs) within the IVDs on the diffusion-weighted images. Diffusion-weighted images and examples of ROIs are shown [Figure 2]. ADC was calculated using the following equation:
where b1 and b2 represent the parameters of the diffusion gradient and S1 and S2 represent the signal intensities at the respective b values. For T2 measurements, we also placed ROIs on T2-weighted images with different TEs to obtain the signal intensity of the IVD [Figure 3]. T2 was calculated by fitting the signal intensities from each echo image using the following equation:
where Sn represents the signal intensity at TEn and S0 represents the initial signal intensity.

- Diffusion-weighted image with (a) b value of 0 s/mm2 and (b) b value of 600 s/mm2 in upright position. (c) Example of ROIs (red circle) on diffusion-weighted image with b value of 0 s/ mm2. (ROI: Region of interest).
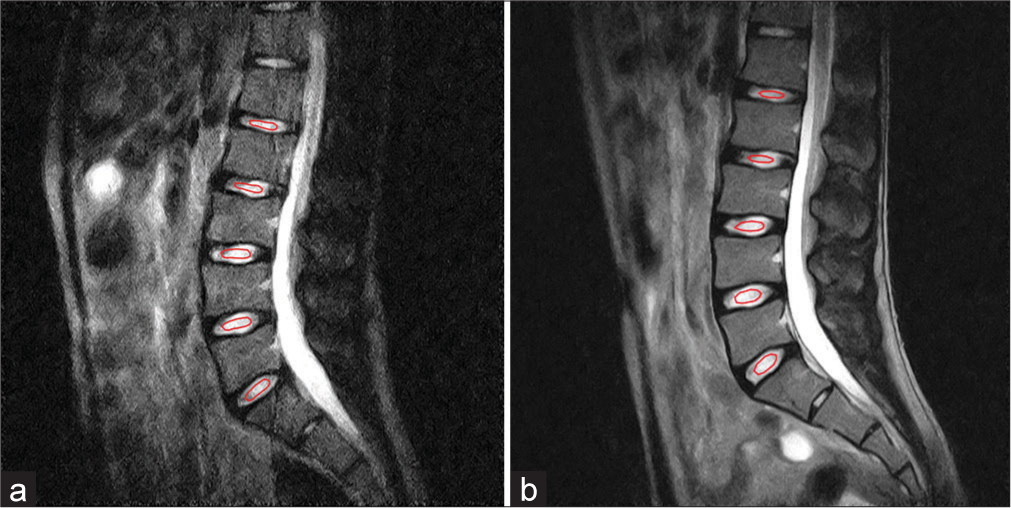
- Example of ROIs (red circle) on T2 weighted images with TE of 30 ms in (a) upright position and (b) supine position. (ROI: Region of interest, T2: Transverse relaxation time, TE: Echo time).
The ROI was drawn manually by a radiological technologist with 2 years of experience and with the mutual consent of the other two authors (a radiologist with 32 years of experience and a radiological technologist with 16 years of experience in MRI). To avoid the influence of partial volume, the ROI was drawn slightly inward from the border between high and low signals. The mean ROI size was 148 mm2 (range, 76–270 mm2).
In addition, the lumbar lordosis angle (LLA) and length of the lumbar spine were measured on a midsagittal T2-weighted image to evaluate the morphology of the lumbar spine. The LLA was defined as the superior open angle intercepted between the two perpendicular lines to the tangent of the superior endplate of L1 and the inferior endplate of L5, as shown in the previous studies.[8] The length of the lumbar spine is the distance between the lower edge of L1 and the upper edge of S1. We determined the midpoint between the upper and lower edges of each vertebral body from L1 to S1 and connected the midpoints with a straight line.
Statistical analysis
Statistical analyses were performed using SPSS for Windows (version 25.0; IBM Corp., Armonk, NY, USA). We compared the T2, ADC, LLA, and length of the lumbar spine between the upright and supine positions using the Wilcoxon signed-rank test. P < 0.05 was considered statistically significant.
RESULTS
The T2 of the IVD between L4 and L5 in the upright position was significantly lower than that in the supine position (P < 0.05). However, there were no significant differences in the T2 values of the other IVDs between the upright and supine positions [Table 1].
| T2 (ms) | P-value | ADC (×10-2 mm2/s) |
P-value | |
|---|---|---|---|---|
| L1/L2 | ||||
| Supine | 76.9±14.3 | 0.09 | 0.89±0.07 | 0.74 |
| Upright | 88.4±11.7 | 0.90±0.07 | ||
| L2/L3 | ||||
| Supine | 97.3±9.5 | 0.24 | 0.90±0.09 | 0.61 |
| Upright | 103.5±9.0 | 0.90±0.12 | ||
| L3/L4 | ||||
| Supine | 107.6±11.5 | 0.31 | 0.91±0.08 | 0.74 |
| Upright | 111.9±10.9 | 0.90±0.11 | ||
| L4/L5 | ||||
| Supine | 109.8±15.3 | 0.04 | 0.89±0.09 | 0.40 |
| Upright | 101.4±10.2 | 0.93±0.09 | ||
| L5/S1 | ||||
| Supine | 96.3±20.9 | 0.18 | 0.86±0.12 | 0.50 |
| Upright | 90.9±17.3 | 0.88±0.12 | ||
T2: Transverse relaxation time, ADC: Apparent diffusion coefficient, IVD: Intervertebral disc, L1~L5: Lumbar vertebrae I-V, S1: Sacral vertebrae I
No significant differences were observed in the ADC of the IVDs between the upright and supine positions [Table 1].
The LLA and the length of the lumbar spine did not differ significantly between the two positions [Table 2].
| Supine | Upright | P-value | |
|---|---|---|---|
| Length (mm) | 158.0±5.7 | 158.4±5.4 | 0.50 |
| LLA (°) | 31.1±5.0 | 34.4±6.5 | 0.13 |
LLA: Lumbar lordosis angle
DISCUSSION
In this study, we compared the IVDs between two different postures using multiposture MRI, and not only morphological information but also functional information was evaluated. We found that the T2 of the IVD between L4 and L5 in the upright position was significantly lower than that in the supine position. This result indicated that the decrease in the water content of the IVD between L4 and L5 was due to gravity. Nachemson[13] and Wilke et al.[14] reported that the pressure inside the IVD was greater in the upright position than in the supine position. Furthermore, it has been demonstrated that the T2 of IVDs correlates strongly with water content.[15] Therefore, the effect of gravity on IVDs in the standing posture may decrease their water content. In addition, only the T2 of the IVD between L4 and L5 decreased significantly, whereas no significant differences were found in the T2 of other IVDs. This indicated that the effect of gravity on the IVD between L4 and L5 was greater than that on other IVDs. This hypothesis is supported by the fact that the most frequent site of lumbar disc herniation is the IVD between L4 and L5.[16,17]
Alkalay et al.[18] reported that the relationship between mechanical loading and diffusion of IVDs and MR diffusivity demonstrated greater sensitivity than that of T2 relaxation times. However, there were no significant differences in the ADC in our study. The study by Alkalay et al.[18] simulates the intradiscal pressure in the standing and supine positions and applies mechanical loading in vitro, but the IVDs used are those of postmortem patients. In addition, most of the discs were IVDs with advanced degeneration. In other words, ADC may be more sensitive to degenerated discs, whereas our study is focused on IVDs that are not degenerated. Therefore, it is possible that there was no significant difference in ADC in this study. Our data showed that T2 relaxation time may be more sensitive than ADC in IVDs without degeneration in vivo.
The LLA and the length of the lumbar spine did not differ significantly between the two positions. The LLA increased from a supine to an upright position, as in the previous reports,[8] but the difference was not significant in this study. This may be due to the subject’s young age and high muscle mass. Ludescher et al. measured the distance between the anterior lower edge of Th12 and the upper edge of S1 in the morning and evening.[2] They reported that although there was no visible morphological difference between morning and evening measurements, the length of the lumbar spine became slightly shorter from early to late measurements. In line with the findings of Ludescher et al.,[2] in our study, there were no morphological changes in the lumbar spine after a postural change from a supine to an upright position. In young subjects, the morphology of the lumbar spine (especially length) may be less changed with postural changes.
A limitation of this study was the small sample size. Moreover, all subjects were healthy young adult males. Therefore, there may be differences in other groups of participants or patients with lumbar spine disease. In addition, manual ROI setting is also a limitation. Although the ROI setting as in Takashima et al.[19] may be desirable to prevent selection bias, we chose this method because the number of samples in the ROI would be too small, which would affect the analysis value. This study revealed the immediate effects of upright position on lumbar discs. Combined with the long-term effects that have already been demonstrated, the pathophysiology of disc disorders such as herniation is expected to be further elucidated. Furthermore, early detection and prediction may become possible.
CONCLUSION
Our study suggests that functional changes occur while morphology remains largely unchanged. The T2 of the IVD between L4 and L5 was likely decreased by the effect of gravity due to the postural change from supine to upright. The results of this study suggest that the use of multiposture MRI provides more detailed information on lumbar IVDs and may help clarify the pathology of lumbar discs.
Ethical approval
This study was approved by the Institutional Review Board at Kanazawa University (approval no. 561-3).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Quantitative analysis of diurnal variation in volume and water content of lumbar intervertebral discs. Clin Anat. 1998;11:1-8.
- [CrossRef] [Google Scholar]
- T2-and diffusion-maps reveal diurnal changes of intervertebral disc composition: An in vivo MRI study at 1.5 Tesla. J Magn Reson Imaging. 2008;28:252-7.
- [CrossRef] [PubMed] [Google Scholar]
- Circadian variation in stature and the effects of spinal loading. Spine (Phila Pa 1976). 1985;10:161-4.
- [CrossRef] [PubMed] [Google Scholar]
- Body height change during upright and recumbent posture. Spine (Phila Pa 1976). 1990;15:202-7.
- [CrossRef] [PubMed] [Google Scholar]
- Apparent diffusion coefficient of intervertebral discs related to matrix composition and integrity. Magn Reson Imaging. 2004;22:963-72.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of apparent diffusion coefficient in normal and degenerated intervertebral lumbar disks: Initial experience. Radiology. 2005;235:569-74.
- [CrossRef] [PubMed] [Google Scholar]
- T1rho and T2 mapping of lumbar intervertebral disc: Correlation with degeneration and morphologic changes in different disc regions. Magn Reson Imaging. 2016;34:932-9.
- [CrossRef] [PubMed] [Google Scholar]
- Lumbar spine MRI in upright position for diagnosing acute and chronic low back pain: Statistical analysis of morphological changes. J Orthop Traumatol. 2013;14:15-22.
- [CrossRef] [PubMed] [Google Scholar]
- Lumbar spine angles and intervertebral disc characteristics with end-range positions in three planes of motion in healthy people using upright MRI. J Biomech. 2019;89:95-104.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of gravity effect on inferior vena cava and abdominal aortic flow using multi-posture MRI. Acta Radiol. 2021;62:1122-8.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of gravity on portal venous flow: Evaluation using multiposture MRI. J Magn Reson Imaging. 2019;50:83-7.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001;26:1873-8.
- [CrossRef] [PubMed] [Google Scholar]
- Lumbar intradiscal pressure. Experimental studies on post-mortem material. Acta Orthop Scand. ;43(Suppl 1960):1-104.
- [CrossRef] [PubMed] [Google Scholar]
- New in vivo measurements of pressures in the intervertebral disc in daily life. Spine (Phila Pa 1976). 1999;24:755-62.
- [CrossRef] [PubMed] [Google Scholar]
- T2 relaxation times of intervertebral disc tissue correlated with water content and proteoglycan content. Spine (Phila Pa 1976). 2009;34:520-4.
- [CrossRef] [PubMed] [Google Scholar]
- The lumbar disc herniation. A computer-aided analysis of 2,504 operations. Acta Orthop Scand. ;142(Suppl 1972):1-95.
- [CrossRef] [PubMed] [Google Scholar]
- A long-term outcome analysis of 984 surgically treated herniated lumbar discs. J Neurosurg. 1994;80:415-21.
- [CrossRef] [PubMed] [Google Scholar]
- MR diffusion is sensitive to mechanical loading in human intervertebral disks ex vivo. J Magn Reson Imaging. 2015;41:654-64.
- [CrossRef] [PubMed] [Google Scholar]
- Lumbar disc degeneration assessment using T2* relaxation time with ultra-short TE. Magn Reson Imaging. 2020;73:11-4.
- [CrossRef] [PubMed] [Google Scholar]






