Translate this page into:
Image-guided Percutaneous Drainage in the Pediatric Population: A Primer for Radiologists
Address for correspondence: Dr. Keerthi Arani, 3210 Belle Court, Royal Oak, USA. E-mail: keerthi3@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Image-guided percutaneous drainage is an excellent minimally invasive method for dealing with infectious complications in the pediatric population. A thorough understanding of drainage procedures in children can often lead to improved patient outcomes. Indications for percutaneous drainage will be reviewed, including abscesses related to appendicitis, post-surgical abscess formation, and abscesses related to Crohn's disease. This pictorial essay will help the radiologist better understand the common etiologies of abscesses in children that may require percutaneous drainage, the special considerations for catheter placement, patient preparation, and anesthesia or sedation issues unique to the pediatric population.
Keywords
Abscess
percutaneous image guided drainage
pediatrics
INTRODUCTION

Percutaneous image-guided drainage procedures are established minimally invasive methods to treat infected or symptomatic fluid collections and to obtain fluid for diagnosis.[1] This has been well described and validated in literature as the preferred first line of treatment in both the pediatric and adult patients.[12] In pediatric population, special considerations, such as adjusted medication doses for sedation, preferential use of ultrasound for image guidance, smaller catheter sizes, and route of access/drainage, should be kept in mind.
Abscess imaging
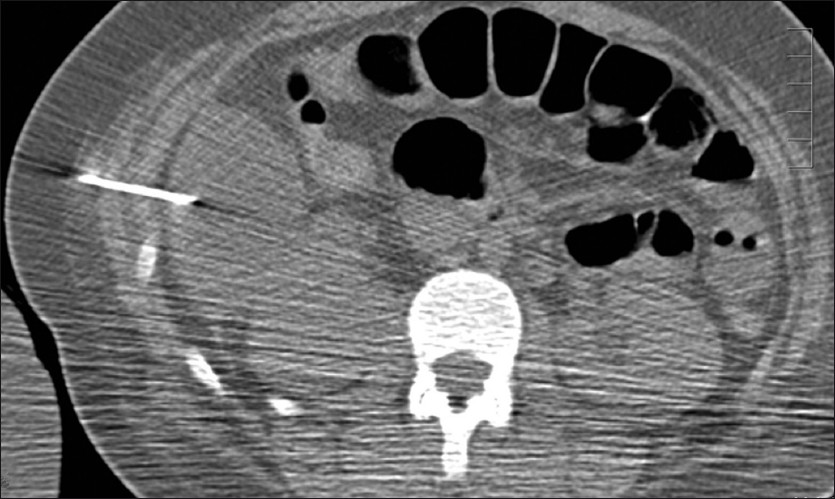
Abscess formation can readily be identified on ultrasound (US) or computed tomography (CT), but specificity is often lacking, given the similar appearances of other fluid collections.[1] Although the presence of gas helps confirm an abscess, lack of air within the fluid collection does not exclude the diagnosis.[2] On CT, an abscess will often appear as a low density region with an enhancing rim.[2] On ultrasound, variable echogenicity is seen, often with a more hyperechoic rim. Layering debris or dirty shadowing secondary to gas can also be identified [Figure 1].[3]
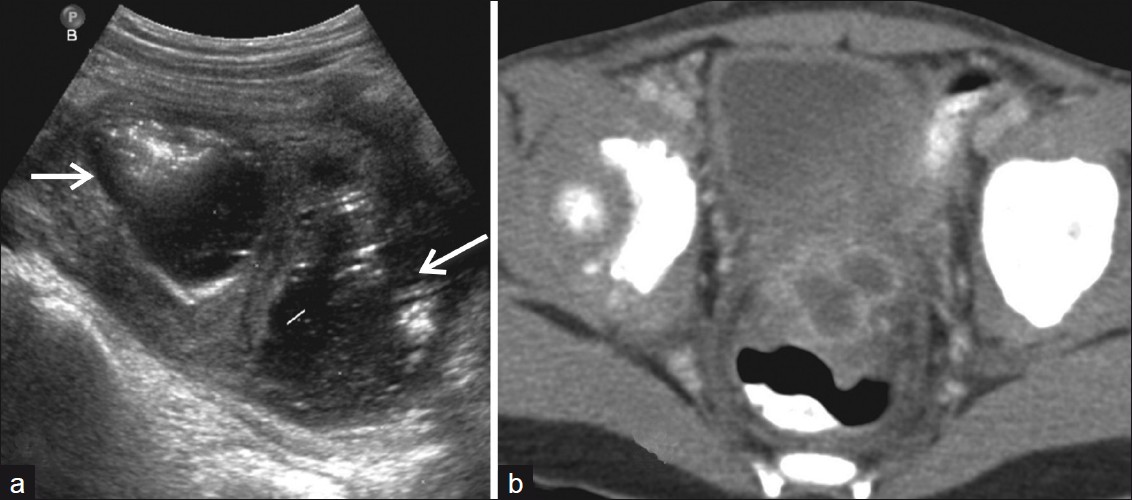
- Abscess formation on ultrasound and CT. (a) Ultrasound shows a heterogeneous fluid collection with dirty shadowing (arrows) consistent with intraluminal gas, a thickened wall and multiple septations in a 13-year-old boy. (b) CT demonstrates a rim enhancing, hypodense, and well-defined bilobed fluid collection in a 15-year-old boy.
Image guidance
Either ultrasound or CT can be utilized for image guidance. Unlike ultrasound, CT can often depict the full extent of an abscess even deep in the abdomen and pelvis. It also offers more precise localization, which is important when there is complex anatomy (e.g. deep pelvis) or when the abscess is adjacent to major vessels or the bowel, specifically the colon.[1] The major disadvantage in using CT for image guidance is the use of ionizing radiation.
The major advantages of ultrasound for image guidance are the lack of ionizing radiation and portable technique. The smaller size of pediatric patients is often ideal for ultrasound imaging. Because ultrasound is not as useful for precise positioning of the catheter, it is more often used in large, easily accessible abscesses [Figure 2].[1] Fluoroscopy can help avoid CT in many cases where ultrasound is used. However, sometimes CT is needed. CT is a frequently used method of image guidance at our institution. In these cases, appropriate techniques are used to reduce radiation dose.
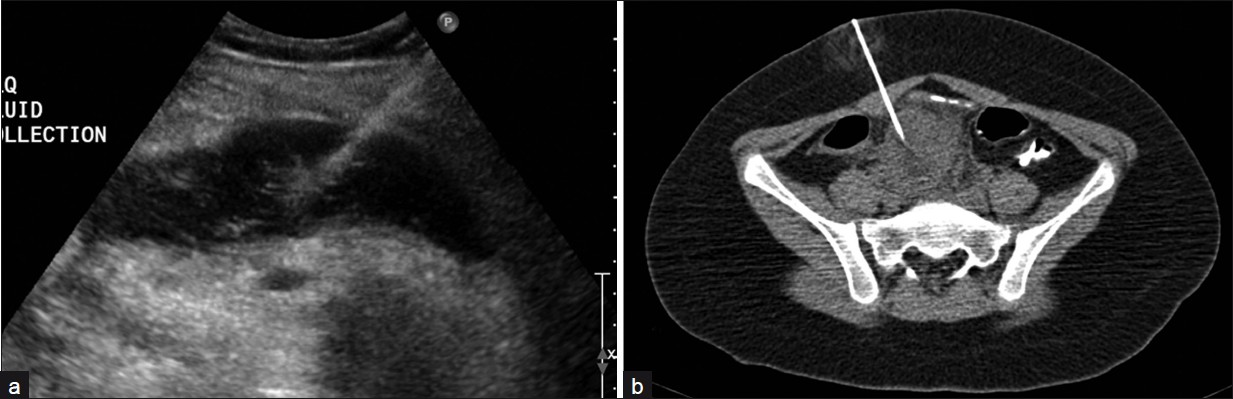
- Ultrasound and CT as a method of image-guided drainage: (a) US guided drainage with trocar placed in a lateral approach into a superficial left lower quadrant abscess in a 17-year-old girl. A 10 French catheter was placed. (b) CT guided trocar placement with an anterior approach in a 12-year-old boy. Both patients demonstrated improvement of clinical signs and symptoms after abscess drainage.
Technical considerations
Catheter placement is most often performed using Seldinger or rarely Trocar technique. An 8F or 10F catheter is often sufficient for pediatric cases, with larger catheters mostly reserved for adolescent patients and collections refractory to initial drainage.[3] Catheters are secured using either external fixation, internal retention, or both [Figure 3].[1] Catheter position should be regularly assessed and the catheter flushed to maintain luminal patency. Catheter complications include clogging and fistula formation. Other complications such as bowel obstruction, perforation or sepsis can result from a malpositioned catheter.[4]
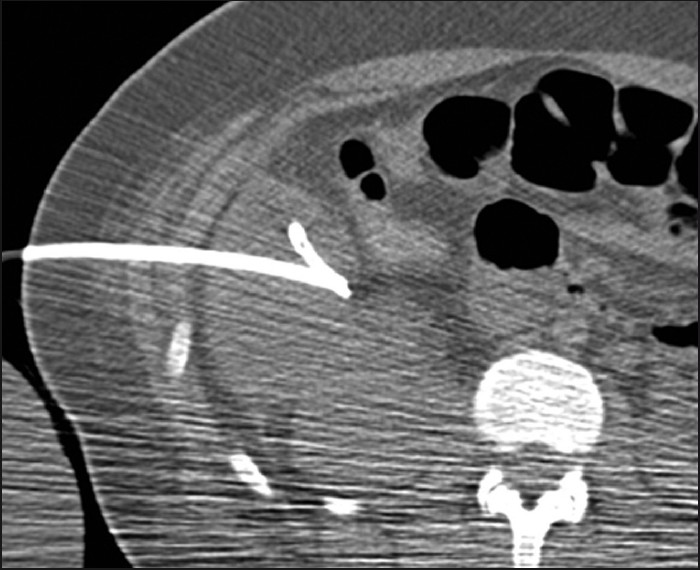
- A 15-year-old girl with ruptured appendicitis and 12 French pigtail catheter placement: The abscess was later shown to decrease in size and the patient had resolution of her fevers and elevated white count.
Contraindications to percutaneous catheter placement include an uncorrected coagulopathy and lack of a safe percutaneous access route.[2] Inadequate percutaneous access also includes the presence of an inter-loop abscess or a large amount of bowel near the abscess [Figure 4].
- Inter-loop abscess: (a) A 14-year-old boy with appendicitis and inter-loop abscess (arrow), (b) A 9-year-old boy with perforated appendicitis and inter-loop abscess (arrow).
Anterior or lateral approach
A lateral approach often necessitates that the patient lie in decubitus position, or prone, after drain placement, which is often less comfortable [Figure 5]. An anterior approach obviously allows the patient to lay supine after catheter placement [Figure 6].
- Lateral approach: A 15-year-old girl with trocar and catheter placed for abscess within the right paracolic gutter from perforated appendicitis. Patient demonstrated improvement of clinical signs after abscess drainage.

- Anterior approach: A 5-year-old girl with trocar placed through an anterior drainage approach for periappendiceal abscess.
Transrectal approach
A transrectal approach is useful for abscesses close to the rectum or posterior to the urinary bladder. This is not a sterile approach, so it should not be used for a possible sterile fluid collection.[1] The transrectal approach is usually well tolerated, has few complications, and allows patients to ambulate and use the toilet normally [Figure 7].

- Transrectal approach: (a) A 13-year-old boy with pelvic abscess after perforated appendicitis. (b) Catheter placed transrectally through endorectal US guidance. The patient showed improvement as evidenced by a decrease in the elevated white count and fever.
Transvaginal approach
Transvaginal drainage may be used in older patients with abscesses found in the cul-de-sac. However, this approach is rarely done, due to the potential psychological impact on the pediatric patient. This route of drainage can be performed in patients who are sexually active, who have had prior pelvic exams or who are accustomed to tampon use[1] [Figure 8].
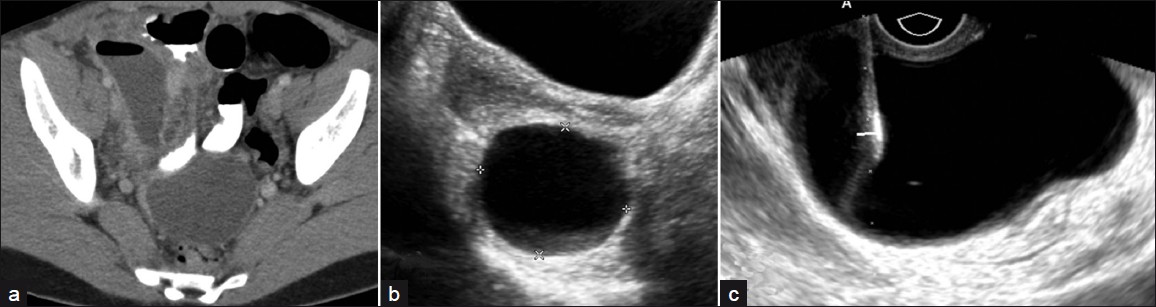
- Transvaginal drainage: (a) A 17-year-old girl with rectouterine fluid collection secondary to perforated appendicitis. (b,c) The patient underwent transvaginal ultrasound guided needle aspiration.
Transgluteal approach
Transgluteal placement involves catheter insertion close to the sacrum, at the level of the sacrospinous ligament. CT guidance is required and the patient is in a prone or decubitus position. Compared to the transrectal approach, the transgluteal approach allows for sterile technique.[5] Of note, in our institution, the transgluteal approach is best performed using a Chiba needle/drain, as close to the sacrum as possible to avoid the more laterally located nerves and vessels (e.g. internal iliac artery and its branches as well as sacral nerves) [Figure 9]. Although potential complications from the transgluteal route include possible nerve damage and infection, studies have shown no major complications.[5]

- Transgluteal drainage: A 11-year-old girl with perforated appendicitis, trocar placed for transgluteal abscess drainage. The patient showed improvement in clinical signs and symptoms after abscess drainage.
Abscess cavity decompression
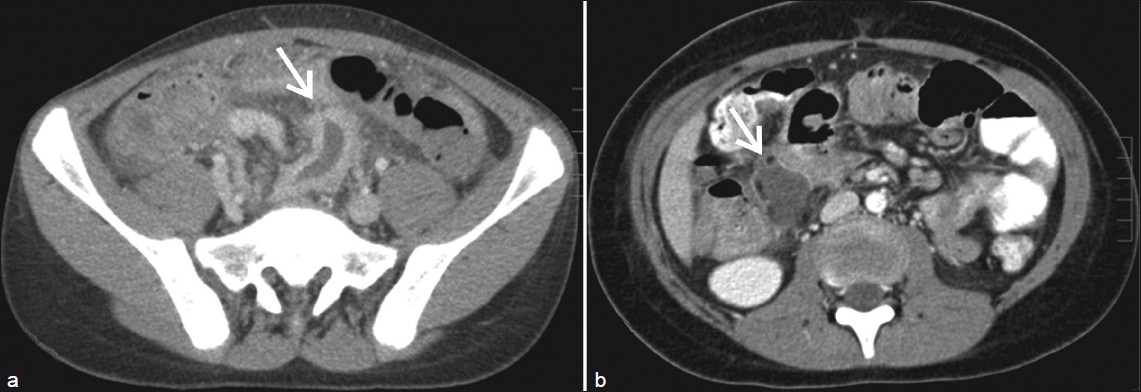
Abscess cavity decompression is performed with direct suction. Some prefer to intermittently irrigate the abscess cavity with 10-15 mL aliquots of saline flush.[4] In addition, research in adult patients has shown the benefit of using urokinase in treating abscesses, especially infected hematomas, loculated abscesses with thick walls and septations, and/or thick purulent debris within the cavity. Even simple irrigation of the abscess cavity allows better drainage of thick debris.[4] Successful drainage is often determined by improving symptoms and laboratory data, along with decreased/resolved fluid collections, which can be monitored by ultrasound or CT. Ultrasound is preferred due to radiation dose issues. If the patient remains symptomatic or the collection persists, consideration should be given to additional aspiration of fluid, drain adjustment/replacement, additional drain placement or if warranted, surgery [Figure 10].[1]

- Monitoring drainage with CT: A 12-year-old boy with (a) right lower quadrant abscess from perforated appendicitis (b) followed by lateral drainage. The patient continued to have abdominal pain and (c) a repeat CT scan showed another rim enhancing, well defined fluid collection in the right paracolic gutter. (d) This was then aspirated and was a sterile hematoma.
Special factors in pediatric percutaneous drainage
Sedation or more likely general anesthesia is often needed in young children during interventional procedures. Anesthesia or sedation necessitates careful monitoring of the patient. Certification in pediatric advanced life support (in combination with basic life support), airway education and competence with sedation is needed for physicians and nurses who perform sedation in children.[1] At our institution, general anesthesia is routinely used in pediatric drainage procedures.
Radiation dose reduction is especially important in children. Consequently, ultrasound is the modality of choice for image guidance, if feasible.[4] If CT must be used, limited scanning is always preferred, along with low dose technique according to the ALARA principle.[5]
Anatomic/body image as well as catheter care issues almost always exclude the use of transvaginal and transperineal drainage routes in pediatrics.
Clinical examples
Common causes of pediatric abscesses include perforated appendicitis, Crohn's disease, bowel perforation secondary to a foreign body, or as a complication of abdominal/pelvic surgery or trauma.[3]
Appendicitis
Perforation is the most common complication of appendicitis and can lead to abscess formation, peritonitis, or both [Figure 11].[25] At our hospital, drainage catheters are frequently placed in patients with abscesses from perforated appendicitis, along with long term intravenous antibiotic use. These patients then undergo delayed elective appendectomy, which reduces morbidity and post-surgical complications.[7]
- A 13-year-old girl with pelvic abscess secondary to perforated appendicitis.
Post operative abscess formation secondary to bowel perforation
Leakage at the site of a surgical anastomosis after bowel surgery (e.g. in patients with ulcerative colitis/ Crohn's disease) is also a relatively common cause of abscess formation in the pediatric population[13] [Figure 12].
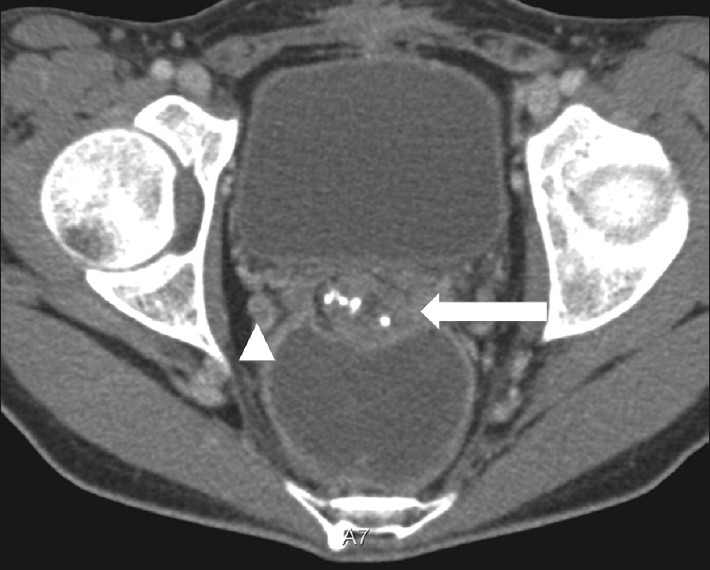
- Postsurgical abscess: A 17-year-old boy with history of ulcerative colitis, s/p total colectomy and ilioanal anastomosis. The patient developed an abscess (arrowhead) adjacent to the anastomatic site (arrow), secondary to an anastomatic leak.
Crohn's disease
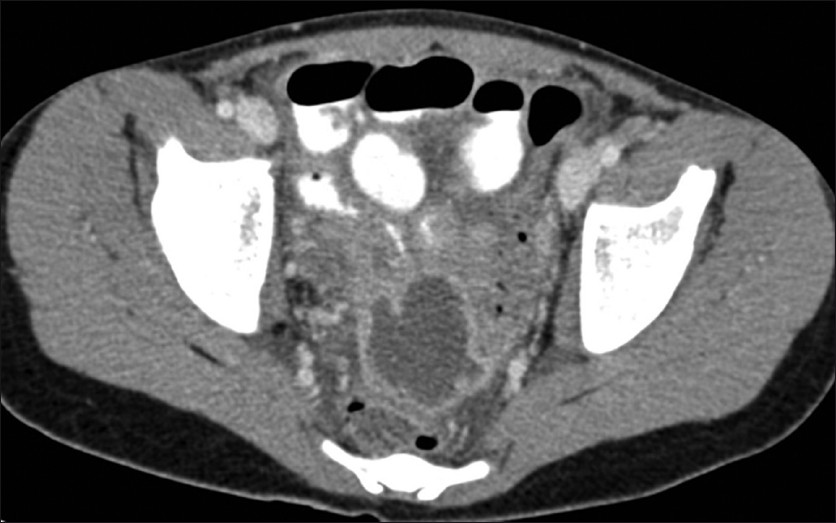
Abscesses can be seen in Crohn's disease and most often occur as a complication of perforation or primary fistula formation [Figure 13]. Pediatric perirectal abscesses are often due to active Crohn's disease.[6] Patients with Crohn's disease also have increased risk of developing recurrent abscesses related to post operative complications, including fistula formation[8] [Figure 14].

- A 15-year-old boy with a perirectal abscess secondary to Crohn's disease.
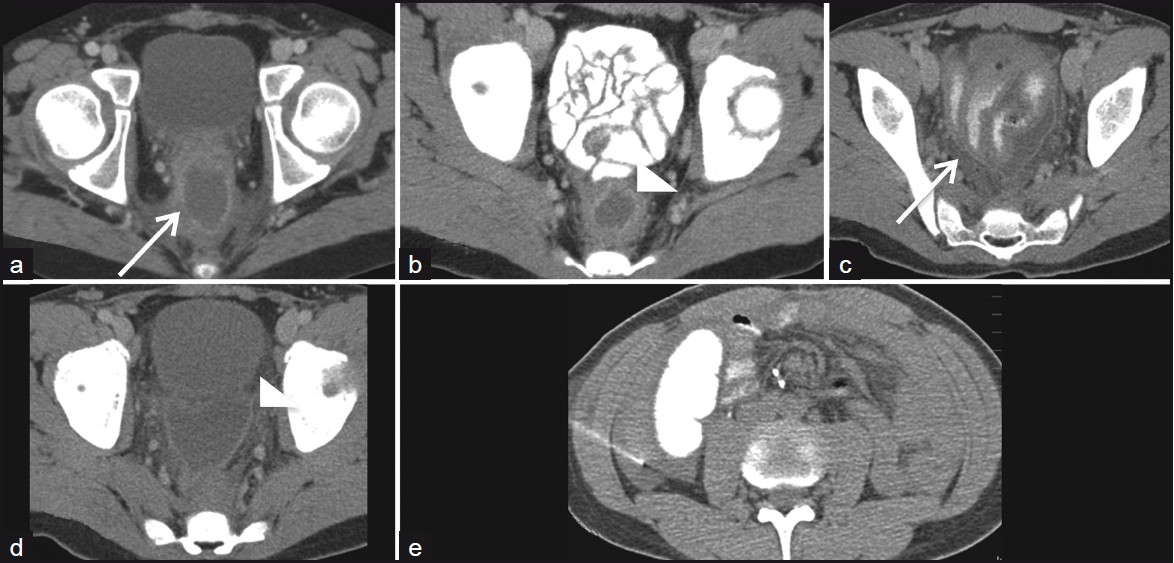
- Postoperative recurrent abscess in Crohn's disease: A 12-year-old boy with history of Crohn's disease and total proctocolectomy for toxic colitis. (a) He had a presacral abscess postoperatively that underwent aspiration (arrow). This resolved on repeat imaging. (b) Nine months later, a recurrent abscess occurred in the same location (arrowhead). (c,d) Two days later, a repeat CT showed enhancement of the peritoneal lining (peritonitis), and intraperitoneal fluid as well as mildly dilated bowel loops (ileus) (arrow, arrowhead). (e) The right paracolic fluid collection was aspirated.
Psoas abscess
Psoas abscesses usually occur as a direct extension of infection from other retroperitoneal structures (e.g. appendicitis, inflammatory bowel disease, tuberculous adenitis, pyelonephritis, or vertebral osteomyelitis).[13] [Figure 15]
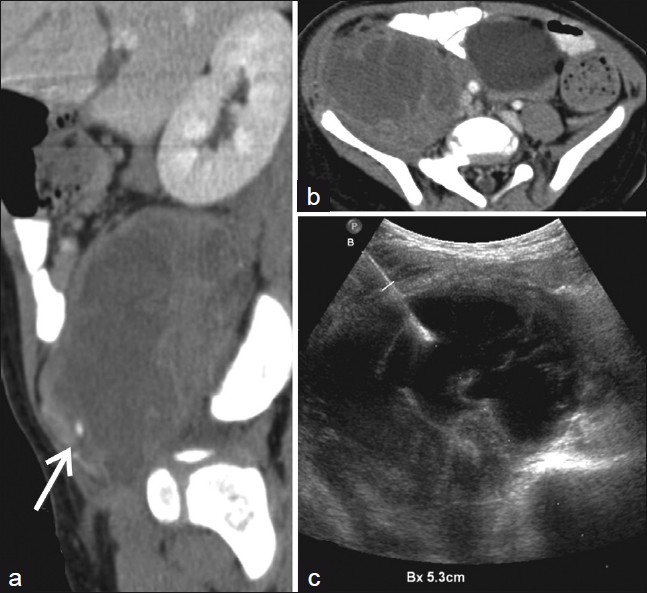
- Psoas abscess: A 2-year-old boy with fever for 6 weeks associated with right leg pain. (a,b) There is a right iliopsoas abscess (arrow) due to Methicillin-sensitive Staphylococcus aureus. (c) The patient had US guided drainage of the abscess. The patient had improvement in clinical signs and symptoms after drainage and was discharged home.
Solid organ abscess
Renal abscess formation usually occurs secondary to inadequately treated acute pyelonephritis.[3] Splenic abscesses usually occur secondary to hematogenous seeding. Hepatic abscesses may be bacterial, amoebic, or fungal in origin [Figure 16].[3]
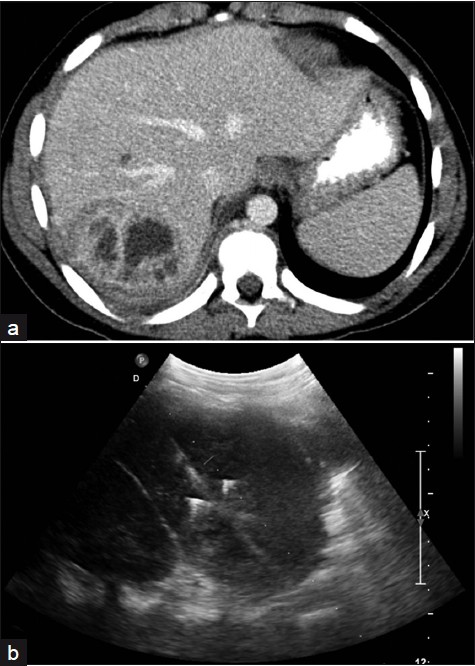
- Hepatic abscess: A 16-year-old boy with multiloculated abscess (a) and drainage through a subcostal approach into the subphrenic hepatic abscess, (b) figure demonstrates needle advanced into abscess. The patient's elevated white count improved and there was less pain after the drainage procedure.
Tubo-ovarian abscess
Pelvic inflammatory disease (PID) affects girls of reproductive age, usually secondary to ascending infection. Infection is usually due to Neisseria gonorrhea or Chlamydia trochamitis.[3] [Figure 17] Multiple approaches can be used for percutaneous drainage, even transvaginal if necessary.[1]

- Tuboovarian abscess: (a, b) 16-year-old girl with pelvic inflammatory disease and a resultant abscess within the cul-de-sac. (c ) 10 French drainage catheter was placed to drain the tuboovarian abscess.
CONCLUSION
Being familiar with pediatric drainage procedures is essential when helping to treat a variety of pediatric diseases and resultant abscesses/ fluid collections.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/31/82243
REFERENCES
- Percutaneous imaging guided abdominal and pelvic abscess drainage in children. Radiographics. 2004;24:737-54.
- [Google Scholar]
- Management of visceral interventional radiology catheters: A troubleshooting guide for interventional radiologist. Radiographics. 2002;22:305-22.
- [Google Scholar]
- CT guided drainage of deep pelvic abscesses: Indications, technique, procedure related complications and clinical outcome. Radiographics. 2002;22:1353-67.
- [Google Scholar]
- Transgluteal approach for draining pelvic fluid collections in pediatric patients. Radiology. 2005;234:893-8.
- [Google Scholar]
- The ALARA concept in pediatric CR and DR: Dose reduction in pediatric radiographic exams—a White Paper Conference Executive Summary. Radiology. 2005;234:343-4.
- [Google Scholar]
- Intracavitary urokinase for enhancement of percutaneous abscess drainage: Phase II trial. AJR Am J Roentgenol. 2000;174:1681-5.
- [Google Scholar]
- Interventional drainage of appendiceal abscesses in children. AJR Am J Roentgenol. 1997;169:1619-22.
- [Google Scholar]






