Translate this page into:
How to Safely Perform Magnetic Resonance Imaging-guided Radioactive Seed Localizations in the Breast

*Corresponding author: Christine Lee, Department of Radiology, Mayo Clinic, Mayo Clinic 200 First Street SW, Rochester, Minnesota 55905, United States. lee.christine@mayo.edu
-
Received: ,
Accepted: ,
How to cite this article: Lee C, Bhatt A, Felmlee JP, Trester P, Lanners D, Paulsen A, et al. How to safely perform magnetic resonance imaging- guided radioactive seed localizations in the breast. J Clin Imaging Sci 2020;10:19.
Abstract
When a breast lesion is seen on only magnetic resonance imaging (MRI) and needs to be excised, pre-operative MRI-guided radioactive seed localization (RSL) is preferred. However, MRI safety and radiation safety issues associated with the inability to recover a potentially lost seed in the MRI scanner room (Zone IV) have precluded this in the past. This manuscript provides a protocol for MRI-guided RSLs that meets MRI safety and radiation safety criteria established by the American College of Radiology and the Nuclear Regulatory Commission. To the authors’ best knowledge, this has never been published in the literature. The complete protocol is provided.
Keywords
Breast magnetic resonance imaging
Magnetic resonance imaging-guided radioactive seed localization
Non-wire localization
Radioactive seed localization
Seed localization
INTRODUCTION
Pre-operative radioactive seed localization (RSL) of breast pathology is a non-wire localization technique that has been shown to shorten perioperative times.[1-7] RSL is usually performed with mammographic or ultrasound guidance, but occasionally, the localization target is not seen on mammogram or ultrasound and is seen only on magnetic resonance imaging (MRI). To the authors’ knowledge, there is nothing in the literature that indicates the number of such RSL cases that would have been better performed with MRI guidance. While an isolated case of MRI-guided RSL has been described in the literature,[8] MRI safety[9-11] and nuclear regulatory[12] concerns precluded, if not prohibited, its use. The MRI safety concern has to do with the stainless steel needle used in pre-loaded seed devices. The nuclear regulatory concern is related to the possibility of losing a radioactive seed in the MRI scan room (Zone IV) without the capability of bringing in a Geiger counter to locate the seed.[9,13] Losing a seed in Zone IV necessitates reporting the loss to the Nuclear Regulatory Commission, which could incur further regulatory actions.
MR safe practices and labeling information[9,11,14-16] distinguish MR safe from MR- conditional items by the degree of hazard in specified MRI environments. MR safe items pose no known hazards in all MRI environments, and MR-conditional items pose no hazard in specified MRI environments and specified use. MR unsafe items pose hazards in all MRI environments. The I-125 seed (Best Medical International, Inc., Springfield, VA) used in RSLs is designed with a tungsten core (MR conditional) and a titanium shell (MR safe).
The seed is pre-loaded in stainless steel (MR unsafe) 18G bevel-tipped needle. One way to obviate bringing the stainless steel needle into Zone IV is to transfer the seed into an MR safe needle in Zone III,[8] but this can be time consuming, particularly when patients are lying prone to the breast coil. An MR safe 18G needle for pre-loading seeds is currently unavailable.
Of more concern is the possibility of losing a seed in Zone IV without being able to bring a hand-held pancake Geiger counter, which is MRI unsafe, into Zone IV. An alternative way to perform MRI-guided RSL when the MRI scanner has a docking table has been developed that meets all safety criteria for MRI and radiation safety at our institution. This manuscript describes the considerations made in this approach, which moves the riskiest component of MRI- guided RSLs into Zone III. The protocol which has been added to the clinical practice is provided.
MATERIALS AND METHODS
MRI-guided procedures, including breast biopsies and wire localizations, are performed on a 1.5T magnet (Singan DV 26, LCC/TRM - 23.0_V02, GE Healthcare, Waukesha, WI) with a docking table. The devices pertinent for MRI-guided RSL and relevant MRI compatibility are listed below.
Needles for the administration of local anesthesia are the same as those for MRI-guided breast procedures.
MRI Coaxial Puncture Needle, 16G, 100 mm (SOMATEX Medical Technologies, Teltow, Germany).
Pre-loaded I-125 seed (manufacturer and product specific, verify MRI compatibility): For example, the Best Medical International I-125 seed (Springfield, VA) is an MR safe titanium shell surrounding an MR conditional tungsten core. The stainless steel needle is MR unsafe in Zone IV.
Pancake detector Geiger counter (Ludlum Model 2 survey meter with Ludlum Model 44-9 pancake Geiger–Muller detector, Sweetwater, TX): MR unsafe in Zone IV.
The static magnetic field in Zone III at various distances from the door between Zone IV and Zone III was measured [Figure 1]. The safety and operability of a Geiger counter in Zone III has precedence with our current PET/MRI systems and procedures.
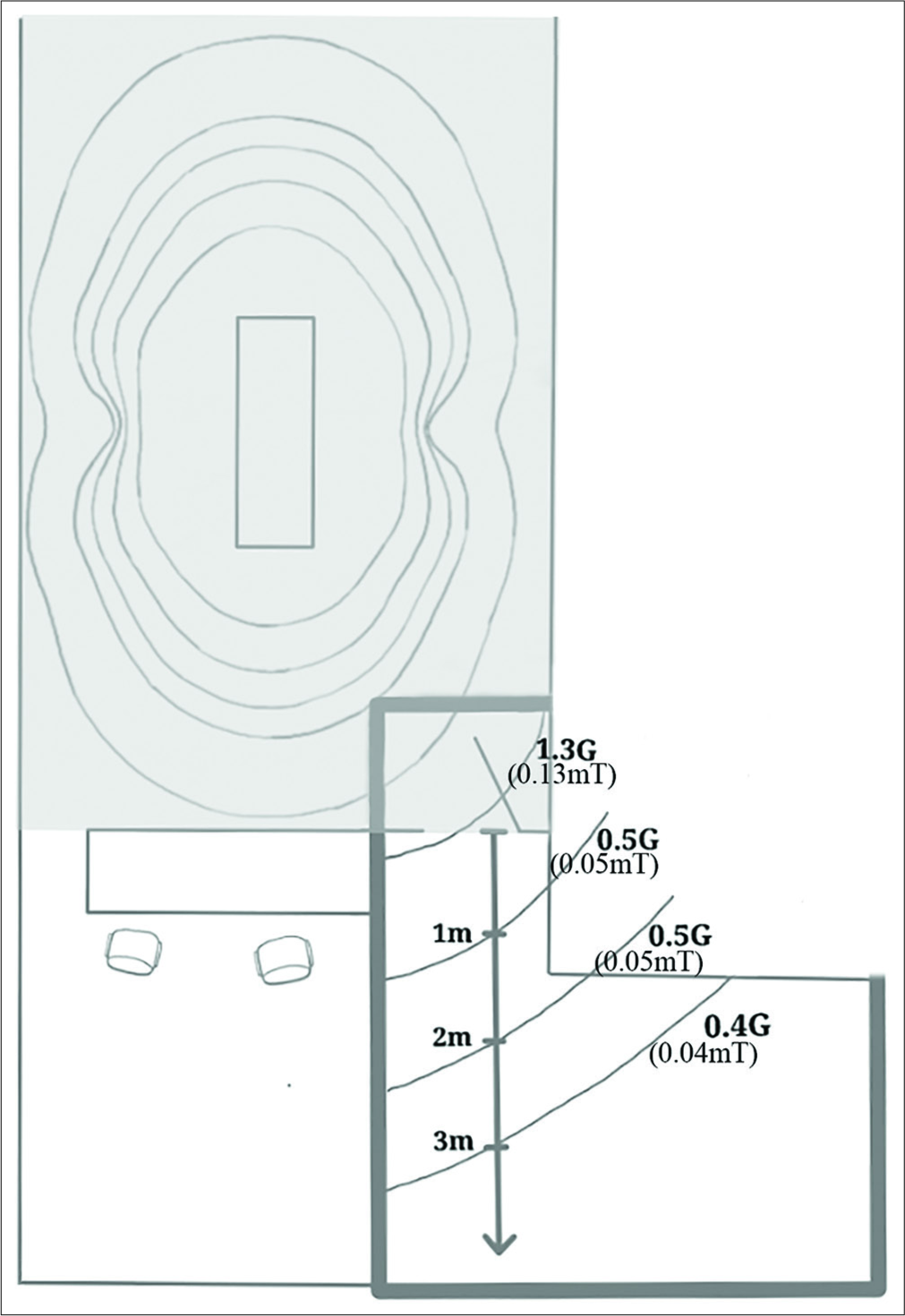
- Schematic diagram of measured static magnetic field at locations from the door within Zone III between Zone IV (gray) and Zone III (white). The area of interest is outlined in dark gray and is the area outside of the magnetic resonance imaging (MRI) scan room with room for the patient and procedure. Here, the measured magnetic fields were 1.3 G (0.13 mT), 0.5 G (0.05 mT), and 0.4 G (0.04 mT) at locations outside of the MRI scan room door.
Protocol
Procedural attire safety check
In alignment with the minimum MR safety standards, insure all team members are wearing MR safe attire, including consideration of pocket less scrubs.
Equipment pause
Confirm Geiger counter in Zone III is labeled and stored/tethered in a dedicated location (similar to PET/ MRI procedures).
-
Procedural whiteboard.
Dynamic count of needles is made on whiteboard.
Needle accounting is performed post-procedure.
MRI-guided breast seed localization
Perform pre-procedural patient evaluation.
Once the patient is brought into to Zone III, perform a pre-procedural time-out to verify patient identity, procedure, site, and physician order. Then, execute a seed-specific time-out: “The number of seeds for this procedure is <#>.”
-
The setup of the MRI table is similar to the setup for a standard MRI-guided breast biopsy or wire localization with slight variations that accommodate the parts of the procedure in Zone III. Anchor a sterile drape underneath the breast coil with enough drape to extend over the table sidearm [Figure 2]. During scanning, the table sidearm is lowered, and the drape is taped to the back of the patient.
Purpose: The sidearm provides a “landing area” for the radioactive seed in Zone III. The sidearm of the table is used in Zone III.
Perform contrast-enhanced breast MRI as for MRI- guided biopsies or wire localizations.[17,18] Identify the target and advance a coaxial puncture needle with adjustments as needed based on MRI acquisitions. This step is completed when the tip of the coaxial needle is in the desired position.
-
Seed placement in Zone III. Undock the MRI table with the patient still in position and move to Zone III. Shut the door to the MRI scanner (Zone IV) tightly.
Once in Zone III, deploy the seed into the coaxial needle system. Then, using a standard coaxial technique, advance the seed into the target.
Remove all devices from the breast. Place Tegaderm (3M, St. Paul, MN) over the skin access site.
Account for all needles and ensure all needles are off the table and properly contained. Perform needle count and confirm with the procedural team.
Confirm that the seed is in the breast using a Geiger counter.
Post-localization MRI in Zone IV. The patient remains on the table as the table is redocked (Zone III to Zone IV). Perform MRI to assess localization.
-
Final check before discharge from Zone III to Zone II. Before the patient leaves the MRI suite (Zone III to Zone II), use the Geiger counter again to confirm that the seed is in the breast. If more than one seed is used (e.g., bracket localization), estimated counts will confirm the presence of more than one seed.
Purpose: Confirming that the seed is within the patient allows the technologist to turn over the MRI room and set up for the next examination. The patient will receive her/his post-localization mammogram.
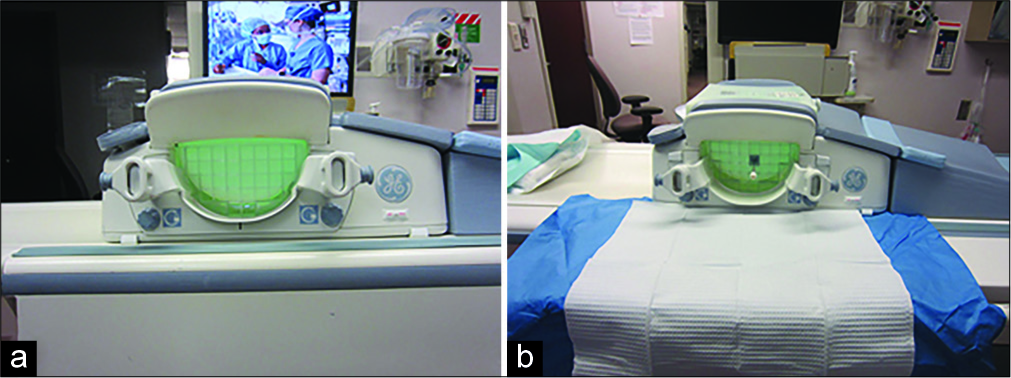
- Draping and use of scan table sidearm. The standard breast coil and setup for MRI-guided biopsies and wire localizations are used (a, table sidearm down). The sterile drape strategically covers the crevices of the magnetic resonance imaging table to prevent losing a seed in the table crevice (b, table sidearm up and draped).
What to do if the seed is not in the breast
-
“Lockdown Zone III.”
When certain counts are not obtained, indicating that the seed is not in the breast, no one should leave Zone III at this point until cleared to do so.
-
“Geiger counter leads.”
To minimize confusion, only the person with the Geiger counter searches for the seed. This person is tasked with evaluating each team member head to bottom of shoes with the Geiger counter and clearing them so they can wait in a designated spot (MRI control room).
“Search systematically.” The most likely location of a lost seed will be on the sidearm of the MRI table, among the sterile drapes, the floor near the MRI table in Zone III, and finally, the floor away from the MRI table in Zone III.
-
“If the lost seed is still not found…”
Lock the door to Zone IV.
Contact the radiation safety on-call person and indicate that there is a lost radioactive source. Radiation safety will assist in the search for the seed, and if the seed is still not located, they will begin the procedure for reporting the lost seed to the state regulators.
Case
Breast MRI to characterize biopsy-proven recurrent invasive ductal carcinoma in the 9 o’clock right breast in a 55-year- old woman showed a 6 mm enhancing mass at the 12 o’clock position adjacent to the fibrous capsule of the implant. This mass was sonographically and mammographically occult, and after a multidisciplinary discussion, the risks and benefits of the procedure were discussed with the patient. After informed consent was obtained, MRI-guided RSL was performed [Figure 3]. Specimen radiograph showed that this 6 mm mass was another site of invasive ductal carcinoma.

- A 55-year-old woman with recurrent invasive ductal carcinoma in the 9 o’clock right breast and a 6 mm enhancing mass seen only on magnetic resonance imaging (MRI) at the 12 o’clock position now needing preoperative localization. Breast MRI showed the biopsy- proven recurrent invasive ductal carcinoma in the right breast at the 9 o’clock position (a, arrow) as well as a 6 mm mass at the 12 o’clock position (b, arrow) that was mammographically and sonographically occult. MRI-guided radioactive seed localization was performed as described in this manuscript with the critical part of the procedure performed in Zone III (c, door to Zone IV is on the left). The position of the tip of the introducer is just anterior to the targeted 6 mm mass (d, arrow). Post-localization MRI (e) shows susceptibility associated with the seed (arrowhead) just superior to the targeted mass (arrow). Post-localization mammogram shows the seed (f, arrow).
DISCUSSION
MRI-guided RSLs in the breast fulfill a clinical need to precisely localize breast cancers seen only on MRI. While MRI-guided wire localizations are available, they are seldom performed at our institution, and the reasons are varied and probably related, in part, to our practice preferences. At our institution, RSLs are favored over wire localizations due to the patient comfort attributed to not having a wire outside of the breast after localization, flexibility in surgical scheduling, reduced overall perioperative time, and decreased risk of wire migration between the time of localization and surgery.[7,19,20]
While cases best served by MRI-guided RSL are few in number compared to mammographic and ultrasound- guided RSLs, the alternatives for MRI-guided RSL when they do occur are limited. These include a best approximation approach by mammogram or ultrasound or placing a clip into the target under MRI guidance and following with mammographic or ultrasound localization. The number of MRI-guided RSLs performed thus far is not large enough to make an evidence-based conclusion, but anecdotally, the time needed to perform MRI-guided RSL as described here takes no longer than an MRI-guided biopsy.
The protocol described here works for our institution, and the steps taken to insure safety clearance of this procedure are reproducible across other practices, where MRI scanners have a docking table. The MRI safety criteria and Nuclear Regulatory Commission safety standards are well documented in the literature.[9,11,21] While enumerating the specific MRI and radiation safety criteria is not within the scope of this manuscript, the authors hope that this will initiate a multidisciplinary discussion with experts and committees responsible for safety oversight in these areas at the reader’s practice. With general guidance from the literature and tailored discussion to address the safety of practice-specific equipment in MRI Zone III environments, it is hoped that MRI-guided RSLs will be available to more patients.
CONCLUSION
The protocol presented provides for safe MRI-guided RSLs in the breast when MRI scanners have a docking table. The protocol is expected to vary to fit practice needs, but the key feature that makes this procedure safe is that the seed is placed in Zone III.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Starting a radioactive seed localization program. Ann Surg Oncol. 2015;22:3197-202.
- [CrossRef] [PubMed] [Google Scholar]
- Radioactive seed localization for breast conservation surgery: Low positive margin rate with no learning curve. Am J Surg. 2017;214:1091-3.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and efficacy of radioactive seed localization with I-125 prior to lumpectomy and/or excisional biopsy. Eur J Radiol. 2013;82:1453-7.
- [CrossRef] [PubMed] [Google Scholar]
- Radioactive seed localization is the preferred technique in nonpalpable breast cancer compared with wire-guided localization and radioguided occult lesion localization. Nucl Med Commun. 2017;38:396-401.
- [CrossRef] [PubMed] [Google Scholar]
- Preoperative localization of breast lesions: Current techniques. Clin Imaging. 2019;56:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Physician preference and patient satisfaction with radioactive seed versus wire localization. J Surg Res. 2017;210:177-80.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of wire localization radioactive seed and Savi scout® radar for management of surgical breast disease. Breast J. 2020;26:406-13.
- [CrossRef] [PubMed] [Google Scholar]
- MRI-guided preoperative125 I seed localizations: Case report. Breast J. 2018;24:397-9.
- [CrossRef] [PubMed] [Google Scholar]
- ACR guidance document on MR safe practices: Updates and critical information 2019. J Magn Reson Imaging. 2020;51:331-8.
- [CrossRef] [PubMed] [Google Scholar]
- Avoiding MRI-Related accidents: A practical approach to implementing MR safety. J Am Coll Radiol. 2018;15:1738-44.
- [CrossRef] [PubMed] [Google Scholar]
- ACR guidance document on MR safe practices: 2013. J Magn Reson Imaging. 2013;37:501-30.
- [CrossRef] [PubMed] [Google Scholar]
- Compliance with the U.S. Nuclear regulatory commission revised licensing guidance for radioactive seed localization. Health Phys. 2018;115:402-8.
- [CrossRef] [PubMed] [Google Scholar]
- Innovations in image-guided preoperative breast lesion localization. Br J Radiol. 2018;91:20170740.
- [CrossRef] [PubMed] [Google Scholar]
- MR implant labelling and its use in clinical MRI practice. Radiologe. 2015;55:682-90.
- [CrossRef] [PubMed] [Google Scholar]
- MR labeling information for implants and devices: Explanation of terminology. Radiology. 2009;253:26-30.
- [CrossRef] [PubMed] [Google Scholar]
- Standards for medical devices in MRI: Present and future. J Magn Reson Imaging. 2007;26:1186-9.
- [CrossRef] [PubMed] [Google Scholar]
- Breast MRI: Guidelines from the European society of breast imaging. Eur Radiol. 2008;18:1307-18.
- [CrossRef] [PubMed] [Google Scholar]
- Breast MRI: EUSOBI recommendations for women's information. Eur Radiol. 2015;25:3669-78.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical utility of radioactive seed localization in nonpalpable breast cancer: A retrospective single institutional cohort study. Int J Surg. 2018;60:149-52.
- [CrossRef] [PubMed] [Google Scholar]
- Preoperative radioactive seed localization for nonpalpable breast lesions: Technique, pitfalls, and solutions. Radiographics. 2015;35:1319-34.
- [CrossRef] [PubMed] [Google Scholar]
- NRC, U.S. United States Nuclear Regulatory Commission. 2018. Available from: https://www.nrc.gov/about-nrc.html [Last accessed on 2020 Jan 25]
- [Google Scholar]






