Translate this page into:
Giant Unruptured Sinus of Valsalva Aneurysm: An Unusual Cause of Right Heart Failure
Address for correspondence: Dr. Tejeshwar Singh Jugpal, Room No. 117, Department of Radiodiagnosis, Lok Nayak Hospital, JLN Marg, New Delhi - 110 002, India. E-mail: tejeshwar.jugpal@gmail.com
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aneurysm of sinus of Valsalva is a rare cardiac abnormality. Unruptured aneurysm of sinus of Valsalva is usually asymptomatic and often discovered incidentally. However, a large aneurysm can, in rare cases, cause compression of the ventricular outflow tract. We report a case of 17-year-old male with congestive right heart failure with a large, partially thrombosed unruptured aneurysm of the right sinus of Valsalva. The aneurysmal sac was compressing the right ventricular outflow tract causing marked dilatation of the right ventricle and atrium that was confirmed on contrast-enhanced computed tomography imaging. Unruptured sinus of Valsalva aneurysm causing right heart failure in adolescence has been rarely reported in literature.
Keywords
Adolescence
aneurysm of sinus of Valsalva
computed tomography
heart failure
right ventricular outflow obstruction

INTRODUCTION
Sinus of Valsalva aneurysm (SVA) is a rare cardiac abnormality seen in 0.09-0.15% of cases with cardiac anomalies.[1] It can be either congenital or acquired. Congenital SVAs are usually encountered in young patients and may be associated with other congenital heart diseases like ventricular septal defect, coarctation of aorta, or bicuspid aortic valve.[2] Unruptured SVAs are usually asymptomatic and rarely discovered, unless they compress adjacent cardiac structures.[3] These cases are mostly seen in middle-aged or elderly patients. SVAs can also rupture and result in an aorto-cardiac shunt that manifests as acute congestive heart failure.[4] Thus, it is important to make a prompt and accurate diagnosis. Contrast-enhanced computed tomography (CT) can provide excellent anatomic depiction of the SVA and also depict any associated complications that may arise.
CASE REPORT
A 17 year-old male presented with a 1-year history of chest pain and dyspnea on exertion. During the past 2 weeks, he had experienced an exacerbation of his symptoms with shortness of breath even at rest, palpitations, pain in the right hypochondrium, abdominal distension, and progressively increasing jaundice.
On clinical examination, he was found to be icteric with hepatomegaly and ascites. There was jugular venous distension and bilateral pedal edema. Cardiac auscultation revealed a pansystolic cardiac murmur in the aortic region and along the left lower sternal border suggestive of aortic and tricuspid regurgitation. On transthoracic echocardiography, he was found to have a large blood-filled sac arising from the aortic root with peripheral thrombus and obstruction of the right ventricular out-flow tract (RVOT). There was severe aortic and tricuspid regurgitation.
Contrast-enhanced CT of the thorax was performed to delineate the anatomical relation of the aneurysmal sac and its level of origin. CT showed a large aneurysmal vascular structure measuring 11.8 × 10.1 × 9.2 cm arising from the right coronary sinus. The lumen of the aneurysm was partially opacified by the contrast, with a large eccentric non-enhancing thrombus noted along the dome of the aneurysmal sac [Figure 1]. There was associated thin peripheral rim of calcification around the wall of the aneurysmal sac. The aneurysmal sac was causing marked compression and attenuation of the RVOT and the main pulmonary artery. The aneurysm was extending along the right atrio-ventricular groove. There was resultant gross asymmetric dilatation of the right atrium and ventricle and associated dilatation of the inferior vena cava and hepatic veins suggestive of congestive changes [Figure 2]. The left cardiac chambers were displaced posteriorly and toward left.
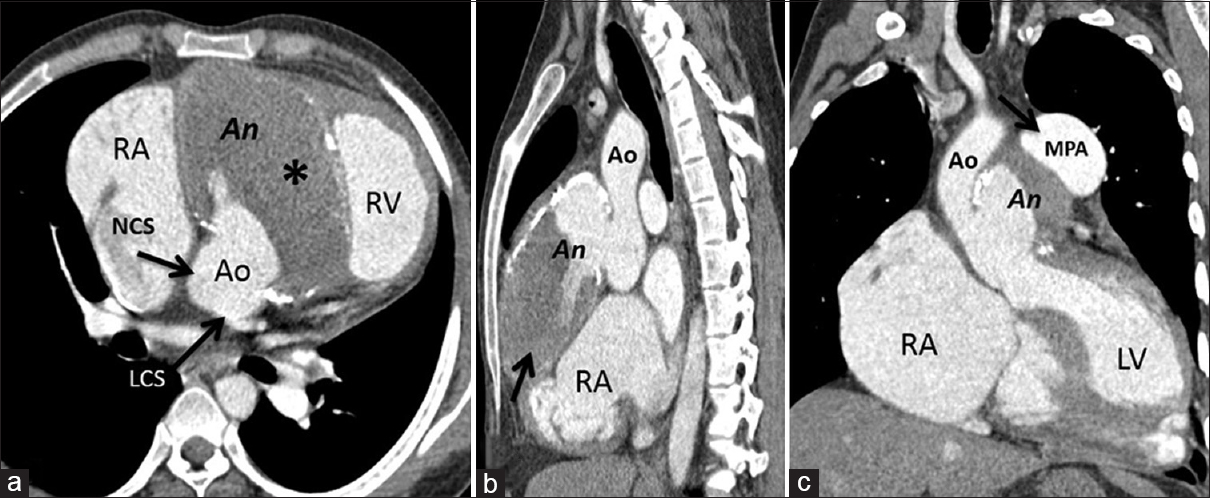
- 17-year-old boy with unruptured right sinus of Valsalva aneurysm, contrast-enhanced CT (a) Axial image reveals a large outpouching (An) arising from the right coronary sinus with eccentric thrombus (*) and peripheral thin calcification and normal LCS and NCS. (b) Oblique sagittal image shows partially thrombosed aneurysm (arrow) with normal aortic root (Ao). (c) Oblique coronal image shows aneurysm with dilated pulmonary artery (arrow) with normal ascending aorta and aortic annulus. Ao = Aortic root, LCS = Left coronary sinus, LV = Left ventricle, MPA = Main pulmonary artery, NCS = Non-coronary sinus, RA = Right atrium, RV = Right ventricle.
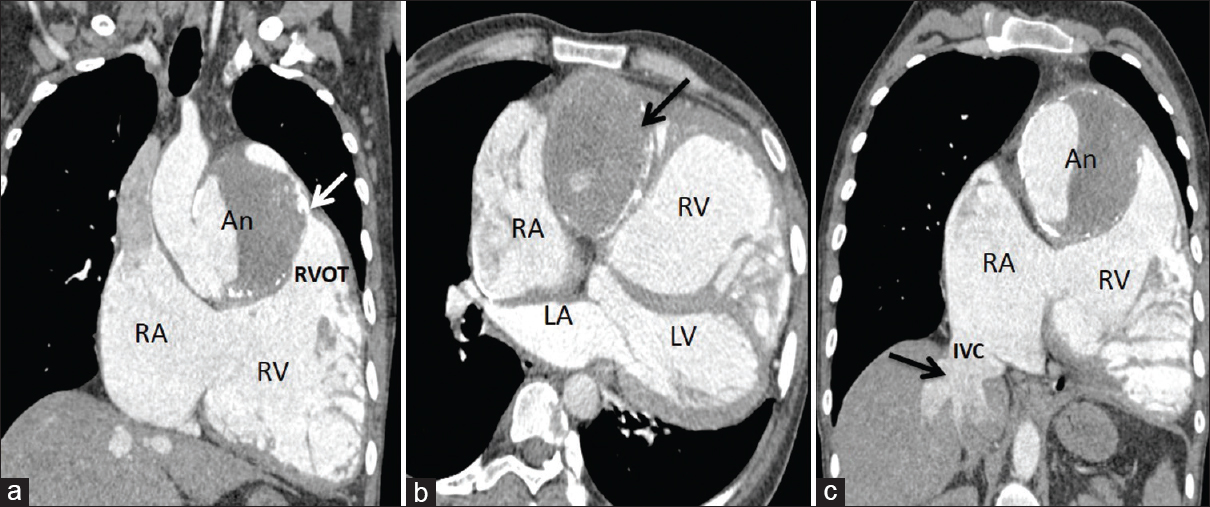
- 17-year-old boy with unruptured right sinus of Valsalva aneurysm, contrast-enhanced CT (a) Coronal image shows aneurysm (An) compressing the RVOT (arrow) with dilatation of RA and RV. (b) Axial image shows the aneurysm extending along right atrio-ventricular groove (arrow). (c) Oblique coronal image shows dilated right cardiac chambers, intrahepatic IVC, and hepatic veins (arrow). An = Aneurysm, LA = Left atrium, LV = Left ventricle, RA = Right atrium, RV = Right ventricle, RVOT = Right ventricular outflow tract, IVC = Inferior vena cava.
The right coronary artery was seen to arise from the tip of the aneurysmal sac. The left coronary and non-coronary cusps appeared normal in morphology. The left coronary artery appeared normal in course and caliber [Figure 1]. Rest of the aorta, arch and its branches were normal in enhancement and morphology.
The patient underwent repair of the aneurysm with a prosthetic patch. Patient had an unremarkable postoperative period. He was discharged on the seventh postoperative day. On follow-up, there was significant improvement of the patient's symptoms.
DISCUSSION
SVAs are a rare clinical entity that can be congenital or acquired.[1] Congenital aneurysm may result from localized weakness of the elastic lamina or an underlying deficiency of normal elastic tissue, with lack of continuity between the aortic media and the aortic annulus leading to weakening and subsequent aneurysm formation. SVA can sometimes be associated with congenital diseases like Marfan's syndrome, Ehlers Danlos syndrome, or Loeys–Dietz syndrome.[4] Acquired SVAs are more common in middle-aged and old patients, and are caused by infectious diseases like bacterial endocarditis and syphilis, or degenerative conditions like atherosclerosis and cystic medial necrosis or aortic root injury from deceleration chest trauma.[34]
The right coronary sinus is the most commonly involved followed by non-coronary sinus.[4] The characteristic diagnostic features of SVA include aneurysmal sac originating above the aortic annulus, saccular shape of the aneurysm, and normal diameter of the aortic root and ascending aorta.[3] SVAs are commonly detected initially by two-dimensional Doppler echocardiography. In most cases, cross-sectional imaging modalities like CT or magnetic resonance (MR) imaging are performed to confirm the findings seen on echocardiography. Nowadays, CT has increasingly been used to evaluate suspected cases of SVAs, especially in the emergency care setting. High spatial resolution and faster scanning have made CT the preferred imaging modality to evaluate SVAs. It provides excellent anatomic detail of the aneurysm and the surrounding cardiac structures. CT can also be used to identify suspected cases of ruptured aneurysm, which appear as a jet of contrast extending from the aneurysm to the cardiac chamber, thereby delineating any aorto-cardiac fistula.[4] MRI can also be used to assess the origin of the aneurysm and define its relationship with adjacent mediastinal structures. They have an added advantage of evaluating the hemodynamic pattern of the left ventricle, identifying any concomitant aortic regurgitation, and quantifying the amount of blood shunting across an aorto-cardiac fistula in cases of ruptured aneurysm. However, limited availability, and increased scan duration and cost are the prohibitive factors in MR evaluation of suspected SVAs.
Unruptured SVAs are usually asymptomatic and incidentally detected. They may become symptomatic if they cause mass effect on the adjacent cardiac structures.[56] These patients usually present with insidiously progressive heart failure with fatigue, dyspnea, palpitation, and features of volume overload. Whereas in patients with ruptured SVA, the clinical presentation depends on the rapidity with which it ruptures and the cardiac chamber with which it communicates. These cases usually present with severe dyspnea, chest pain, and hemodynamic instability or with progressive heart failure.
Therefore, large unruptured aneurysms of the right sinus of Valsalva may compress the RVOT and cause obstruction. When this happens, patients may present with symptoms of right heart failure, similar to what we encountered in our case. Large unruptured SVA causing RVOT obstruction and concomitant right heart failure has usually been reported in middle-aged and old patients.[78] We could find only three cases of young patients with unruptured SVA causing cardiac compression in the literature.[569] The reported cases of SVA with right heart failure in young patients have usually been associated with ruptured aneurysm and resultant fistula formation with right cardiac chambers or RVOT.[410] Thus, our patient who was an adolescent boy presented with a giant partially thrombosed chronic unruptured SVA causing right heart failure. Such a case has rarely been reported.
The mainstay of treating a case of symptomatic unruptured and ruptured SVA is cardiopulmonary bypass surgery with closure of aneurysmal sac and repair of the defect. Percutaneous transcatheter closure can also be used for treating SVAs. In asymptomatic patients where the aneurysmal sac is small, surgery can be deferred; however, large aneurysms should undergo surgical repair to avoid complications.
CONCLUSION
SVAs involve right coronary, non-coronary, and left coronary sinus in decreasing order. They are usually asymptomatic, but can rupture or become large enough to compress cardiac chambers. The clinical presentation of patients with SVA varies from incidentally discovered cardiac murmurs to chest pain, progressive heart failure, and sudden cardiac arrest. Surgical repair is the mainstay of treatment with excellent prognosis in post-operative patients. Therefore, prompt diagnosis and rapid repair is imperative. SVAs are initially detected by echocardiography; however, contrast-enhanced CT images provide excellent anatomic description and prompt diagnosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2015/5/1/64/170733
REFERENCES
- Sinus of Valsalva aneurysm with rupture. Case report and literature review. Cir Cir. 2009;77:441-5.
- [Google Scholar]
- Bicuspid aortic valve and unruptured sinus of Valsalva aneurysm, a rare association. Int J Cardiol. 2015;202:103-5.
- [Google Scholar]
- Valsalva sinus aneurysms: Findings at CT and MR imaging. Radiographics. 2010;30:99-110.
- [Google Scholar]
- A rare case of sudden dyspnea and unexpected death in adolescence: Fistula from aortic sinus of Valsalva to right atrium. Int J Clin Exp Med. 2014;7:2945-7.
- [Google Scholar]
- A patient with aneurysm of both aortic coronary sinuses of Valsalva obstructing both ventricular outflow tracts. Cardiol Young. 2009;19:537-9.
- [Google Scholar]
- Unruptured aneurysm of the sinus of Valsalva presenting with right ventricular outflow obstruction. Tex Heart Inst J. 2003;30:152-4.
- [Google Scholar]
- An unusual case of right- sided heart failure caused by giant sinus of Valsalva aneurysm obstructing right ventricular outflow tract. Eur Heart J. 2014;35:2721.
- [Google Scholar]
- Ruptured right sinus of Valsalva into main pulmonary artery. J Cardiovasc Dis Res. 2012;3:132-4.
- [Google Scholar]






