Translate this page into:
Frequency of myocardial infarcts on conventional, non-gated CT: An often-overlooked entity
*Corresponding author: Jabi Elijah Shriki, Department of Radiology, University of Washington, Seattle, United States. jabielijah@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shriki JE, Prosper AE, Shinbane J, Colletti PM. Frequency of myocardial infarcts on conventional, non-gated CT: An often-overlooked entity. J Clin Imaging Sci. 2024; 14:45. doi: 10.25259/JCIS_114_2024
Abstract
Objectives:
The objective of this study was to determine how often myocardial infarctions are retrospectively visible on conventional, non-gated, non-cardiac computed tomography (CT) scans. Our goal was to evaluate a cohort of patients with myocardial infarctions visible on cardiac magnetic resonance imaging (MRI) to determine how often the area of infarction was retrospectively visible by preceding, conventional CT. We also sought to evaluate how often the diagnosis of myocardial infarction was reported at the time of initial study review.
Material and Methods:
The Institutional Review Board approval was obtained for the creation and retrospective analysis of a database of patients undergoing cardiac MRI. We started with a cohort of 252 patients who had undergone cardiac MRI at our institution, over a 4-year period. We identified 160 patients who had a myocardial infarct visible on MRI.
Results:
Of the 160 patients who had been identified as having an infarct on cardiac MRI, 54 patients had undergone a recent (within 30 days) conventional CT scan, usually done for non-cardiac indications. In addition to the review of reports, non-cardiac CT scans were also evaluated retrospectively by two experienced, cardiothoracic imaging physicians, including a radiologist and a cardiologist. In 26 of these patients (48.1%), an infarct was visible on the CT images. In 12 of these 26 cases (46.1%), the infarct was noted in the initial report. In the remaining 14 of these 26 cases (53.8%), the infarct was unrecognized at the time of initial study interpretation.
Conclusion:
Our retrospective analysis demonstrates that myocardial infarctions may be frequently observed on non-gated, non-cardiac CT scans but may be underrecognized and under-reported.
Keywords
Non-gated computed tomography
Myocardial infarction
Incidental myocardial infarction
Conventional computed tomography
INTRODUCTION
There is increasing emphasis on thoroughly evaluating the heart on computed tomography (CT) for incidental findings, even when patients are scanned for non-cardiac indications.[1,2] Cardiac findings, even when unsuspected, may contribute important findings in the work-up and evaluation of patients presenting for other pathology.[3,4]
Cardiac magnetic resonance imaging (MRI) has emerged as the gold standard for detecting and characterizing myocardial infarctions.[5] Cardiac CT, obtained with gating, can also demonstrate myocardial infarctions.[6] However, myocardial infarctions may also be visible on non-cardiac and non-gated CT scans. A spectrum of appearances of incidentally detected myocardial infarction on CT has been reported. Findings consist of lipomatous metaplasia; mural calcifications; areas of focal wall thinning; areas of focal or subendocardial non-perfusion; aneurysms in typical locations, including apical aneurysms; and apical thrombus.[7] In particular, non-cardiac CT scans may have a role in demonstrating some of these findings, including identifying areas of fatty change along the subendocardial surface of the left ventricular (LV) chamber in the case of lipomatous metaplasia after myocardial infarctions.[8]
With the proliferation of lung cancer screening CT, there is an increased need to enhance recognition of myocardial pathology in a patient population with elevated risk.[9] Improving familiarity with the spectrum of cardiac pathology can enhance reader skill sets and translate to an improvement in the detection of cardiac pathology in clinical settings.[10]
MATERIAL AND METHODS
Following the Institutional Review Board approval, a retrospective study of our cardiac imaging population was initiated. Our institution granted approval for the creation of a database of cardiac MRI reports and for retrospective evaluation of imaging studies based on reported findings.
Patient population
Over a 4-year period at our institution, a large county hospital, 252 patients received cardiac magnetic resonance (MR). Of these 252 patients, 160 were determined to have prior myocardial infarction as evidenced by late gadolinium enhancement. These 160 patients were selected as our known myocardial infarct population. Among these 160 patients with known myocardial infarction, 54 also received conventional CT scans within 30 days before their cardiac MRI study. These 54 patients’ conventional CT images were reviewed for findings of myocardial infarction (none of these 54 conventional CT scans consisted of dedicated cardiac imaging, and all were non-cardiac/non-gated scans).
Image analysis
All cardiac MR images were reviewed by two experienced readers who confirmed that the morphologies of areas of late gadolinium enhancement were consistent with infarction. All CT studies were also reviewed by two expert cardiac readers who evaluated the images for evidence of myocardial infarction. Reader 1 was a radiologist with 5 years of experience in dedicated cardiac imaging. Reader 2 was a cardiologist with 5 years of experience in cross-sectional cardiac imaging (CT and MRI). Both readers were board certified by the Certification Board for Cardiovascular CT.
Studies were initially reviewed individually by each reader and were subsequently re-reviewed with consensus interpretation. However, no discrepancies in scan interpretation were present. (both readers agreed in the interpretation of all the 26 patients who had a myocardial infarction on CT, out of the 54 patients who had also had an infarct visible on cardiac MRI.).
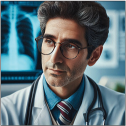
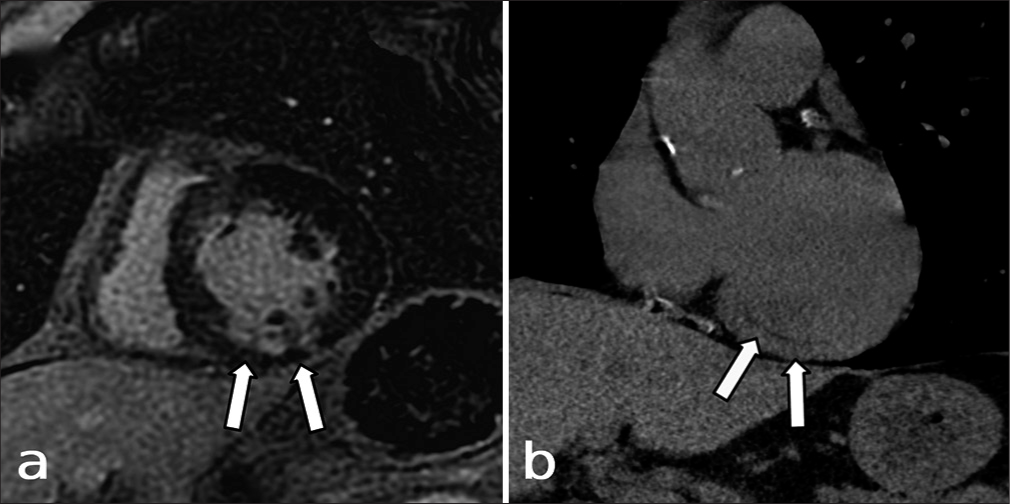
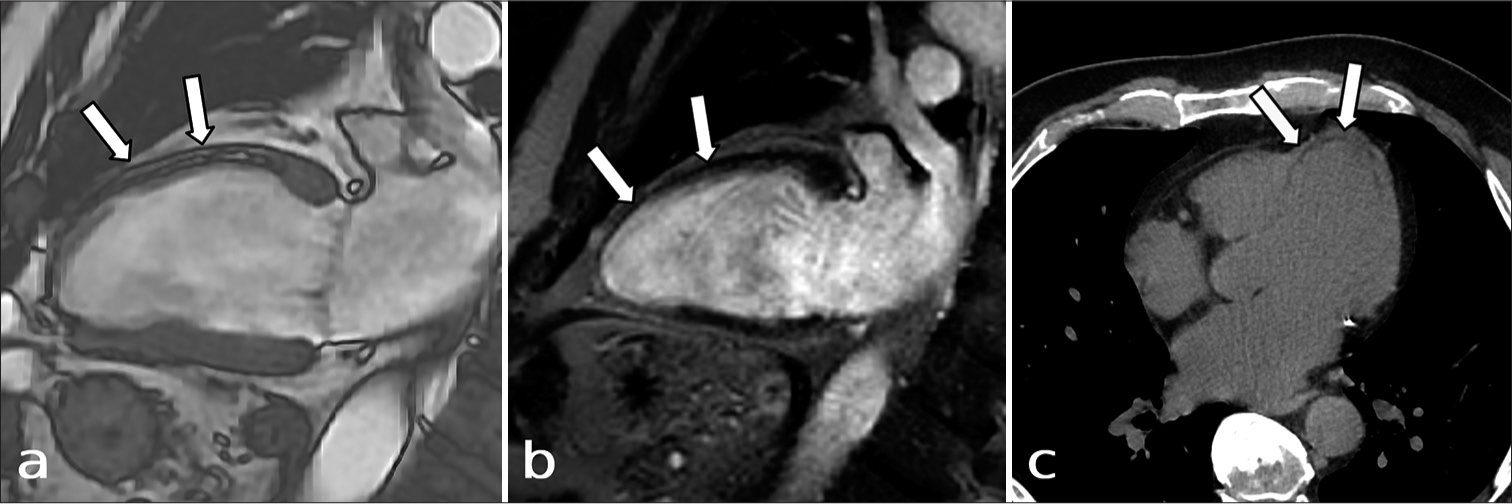
Findings used to identify infarction on CT images included lipomatous metaplasia of the LV wall [Figure 1]; focal myocardial thinning [Figure 2]; subendocardial or focal non-enhancement of the LV wall; aneurysm or pseudoaneurysm; myocardial wall calcifications without any other potential explanation; and the presence of an LV apical thrombus [Figure 3].
- A 72-year-old male with known coronary disease and infarction seen in a scintigraphic study. A non-contrast chest computed tomography (CT) is also done for the evaluation of a pulmonary nodule. Short axis, phase-sensitive inversion recovery late gadolinium enhancement magnetic resonance imaging (a) shows an area of focused, delayed gadolinium enhancement in the inferior wall (white arrows, a). An oblique coronal, non-contrast CT image is also shown (b). The area of infarction corresponds to a subtle area of low attenuation consistent with lipomatous metaplasia (white arrows) in this probable, chronic, myocardial infarct.
- A 64-year-old male undergoing work-up for revascularization. (a) The balanced steady-state free precession, 2-chamber view shows a “double-line” sign (white arrows), as may be seen in the setting of lipomatous metaplasia, and is caused by chemical shift artifact surrounding the area of infarction when fat is present. (b) This is also seen in the corresponding phase sensitive inversion recovery, 2-chamber view with late gadolinium enhancement throughout the wall (white arrows). (c) This is also evident as an area of low attenuation on CT (white arrows), corresponding to the area of wall thinning on the cardiac MRI, consistent with a chronic myocardial infarction.
- A 73-year-old male with acute presentation to the emergency department for failure to thrive. (a) Apical thrombus is noted within the left ventricle on conventional, non-gated, non-cardiac CT (white arrow). (b ) Oblique, 4 chamber, phase sensitive inversion recovery cardiac MR demonstrates an LAD territory area of late gadolinium enhancement (white arrowheads). The apical thrombus is more clearly seen as well (white arrow).
6 of the patients in our cohort with identification of an infarct on MRI had previously undergone a CT pulmonary angiogram. In 38 of the 54 patients who had CT scans before MRI, studies were performed with contrast. In the remaining 10 patients, scans through the heart were non-contrast studies.
RESULTS
Of the 54 patients with myocardial infarction visible on cardiac MRI, and with routine CT images available for review, we determined that 26, 48.1%, had evidence of myocardial infarction on their CT images. Of these 26 patients, 23 patients had focal or subendocardial areas of non-enhancement; 17 patients had areas of lipomatous metaplasia; 10 patients had focal areas of myocardial wall thinning; 3 patients had left ventricular apical thrombi; and 2 patients had myocardial calcifications with morphology consistent with infarcts.
In examining the 26 patients where myocardial infarctions were detectable on CT, there seemed to be a difference in detection rates, based on infarct distribution. In all cases, there was a single or dominant area of infarction, based on the cardiac MRI findings. In other words, none of the patients in our cohort demonstrated large infarcts in multiple territories. The best detection rate was seen in patients with lateral infarcts, among which 7 of the known 9 infarcts (77.7%) were visible in retrospect on CT. The next highest rate of detection was seen in patients with anterior infarcts, of which 5 patients of the known 8 with anterior infarcts on MRI (62.5%) showed evidence of infarction on CT. Patients with septal myocardial infarcts were visible on conventional CT in 4 of the 8 patients with infarction on cardiac MRI. Among the 12 patients with apical infarcts on cardiac MRI, 5 showed signs of infarction on CT. Least detectable on routine CT was the inferior infarcts, which were seen on conventional CT in only 4 of the 16 (25%) patients with known infarctions on cardiac MRI. 1 patient had a large, left anterior descending territory area with diffuse calcifications involving multiple walls. This patient had an aortic dissection with involvement of the left main coronary artery ostium. This patient also had extensive late gadolinium enhancement on MRI in the area of infarction.
Of the 26 patients who we determined to have evidence of myocardial infarction on CT, 12 of these patients had myocardial infarct reported on CT, while the remaining 14 were unrecognized at the time of initial interpretation.
Due to the small sample size, we did not perform further statistical analysis. The presence or absence of contrast administration did not appear to make a difference in the visibility of infarcts on preceding CT scans. Of the 6 patients who underwent CT scanning in the pulmonary arterial phase (CT pulmonary angiograms), 1 infarct was visible. Of the 38 patients who underwent scanning with contrast in a later phase (usually 60 s, per institutional protocol), 22 patients had infarcts which were visible. In the remaining 10 patients who underwent non-contrast imaging, 3 of these patients had visible myocardial infarcts.
DISCUSSION
These results point to the fact that important myocardial findings may be visible on conventional, non-gated, non-cardiac CT. In our study, myocardial infarcts on MRI were found to have correlated with many of the preceding CT scans. However, these infarcts were only reported in 12 out of the 26 patients with visible findings of myocardial infarcts on CT.
This is congruent with other studies which have also shown that cardiac findings are underrecognized and underreported in conventional, non-gated, non-cardiac CT studies. Sverzellati et al. reported that cardiac findings were unreported in 168 out of 266 (63.2%) patients in their cohort.[11] Another review by Choy et al. found that significant cardiac findings were not recognized in 22.3% of 268 patients.[12] Variability in other studies in the reporting of overlooked cardiac findings may be related to the lack of standardization of definitions for significant, relevant, or reportable cardiac findings. However, other reports have similarly underscored that there should be increased recognition of cardiac findings.[1,7]
Our analysis has the strength of using a gold standard of cardiac MR. To our knowledge, no prior study has evaluated CT scans retrospectively with an established gold standard for identifying cardiac pathology. Although all the patients in our cohort underwent cardiac MRI, the large number of infarcts which were visible on conventional, non-gated CT scans suggests that increased attention to the myocardium on CT is necessary.
There is also other significance to the conclusions that follow from our retrospective analysis. First, this review shows that myocardial infarctions are still under-recognized despite the fact that several studies and educational review articles have provided increased attention to myocardial infarction as an underrecognized entity.[7] Our study shows that there is still under-diagnosis of some of the myocardial infarctions that are visible on conventional CT. Second, we have anecdotally observed that there is the utility of reviewing conventional CT images in raising diagnostic confidence when infarcts are difficult to delineate in cardiac MRI studies. Chronic infarcts may show less avid late gadolinium enhancement.[8] In these settings, it is useful to review CT images for lipomatous metaplasia and other findings of chronic infarction. Reviewing conventional CT may be helpful to enhance reader confidence when an infarct is difficult to see on other sequences or when some of the MRI sequences are limited.
However, there are several weaknesses in our analysis. Chiefly, there was a small sample size in our study. As a result, some conclusions that are suggested from our results ought to be studied further for better validation. For example, lateral wall myocardial infarcts were most easily seen. However, inferior wall myocardial infarcts were less commonly seen. This may be related to technical factors. The inferior myocardium is closer to the plane of scanning than other walls. This might contribute to less optimal visualization of inferior myocardial wall pathology. Due to our small sample sizes, this conclusion is difficult to advance with higher certainty.
We also did not have a large enough study population to make specific conclusions about the differential visibility of myocardial infarctions based on the technique of scanning or the presence or absence of contrast administration. Lipomatous metaplasia might be more visible in a non-contrast study, as has been previously suggested.[8,13] Subendocardial or focal perfusion abnormalities in the myocardium, by definition, would only be seen on post-contrast imaging.[14] However, without a larger sample size, it is difficult to validate these claims further.
We also did not consider whether myocardial infarctions were acute (within 7 days), subacute (within 6 months), or chronic (>6 months in age).[15] Acute infarctions are likely to be better seen on perfusion imaging and show more pronounced edema, whereas chronic infarctions are more likely to demonstrate lipomatous metaplasia or calcification.[7] In our cohort, it was difficult to determine the age of myocardial infarctions, and we felt that further stratification of infarcts based on infarct age would be difficult. However, further research could ask the question of whether chronic or acute infarcts are more visible in conventional CT studies.
We also did not evaluate other cardiac findings. Additional cardiac findings including cardiac masses[16] and coronary findings[17] may be visible on non-gated, non-cardiac CT, although this was beyond the scope of our analysis in this study.
CONCLUSION
This study shows that in patients with proven infarcts based on cardiac MRI, conventional CT may often reveal that the infarct is visible. However, we also noted that myocardial infarcts were under-reported in our study, suggesting that radiologists ought to carefully evaluate the myocardium on conventional, non-cardiac/non-gated CT.
Ethical approval
The IRB approval for creation of a cardiac MRI database and retrospective review of the studies and reports is HS-07-00020 dated 6/27/2019.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Managing incidental findings on thoracic CT: Mediastinal and cardiovascular findings. A white paper of the ACR incidental findings committee. J Am Coll Radiol. 2018;15:1087-96.
- [CrossRef] [PubMed] [Google Scholar]
- Incidental cardiac findings on computed tomography imaging of the thorax. BMC Res Notes. 2010;3:326.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of incidental findings in computed tomographic screening of the chest: A systematic review. J Comput Assist Tomogr. 2008;32:214-21.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and clinical significance of incidental cardiac findings in non-ECG-gated chest CT scans. Radiologe. 2011;51:59-64.
- [CrossRef] [PubMed] [Google Scholar]
- Role of cardiac magnetic resonance imaging in myocardial infarction. Curr Cardiol Rep. 2017;19:101.
- [CrossRef] [PubMed] [Google Scholar]
- CT detection of acute myocardial infarction. Am J Roentgenol. 2004;182:1563-6.
- [CrossRef] [PubMed] [Google Scholar]
- Incidental myocardial infarct on conventional nongated CT: A review of the spectrum of findings with gated CT and cardiac MRI correlation. Am J Roentgenol. 2012;198:496-504.
- [CrossRef] [PubMed] [Google Scholar]
- Chemical shift artifact on steady-state free precession cardiac magnetic resonance sequences as a result of lipomatous metaplasia: A novel finding in chronic myocardial infarctions. Can J Cardiol. 2011;27:664.e17-23.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary arterial calcification on low-dose ungated MDCT for lung cancer screening: Concordance study with dedicated cardiac CT. Am J Roentgenol. 2008;190:923-8.
- [CrossRef] [PubMed] [Google Scholar]
- Detection of cardiac incidental findings on routine chest CT: The impact of dedicated training in cardiac imaging. J Am Coll Radiol. 2018;15:1153-7.
- [CrossRef] [PubMed] [Google Scholar]
- Under-reporting of cardiovascular findings on chest CT. Radiol Med. 2016;121:190-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pertinent reportable incidental cardiac findings on chest CT without electrocardiography gating: Review of 268 consecutive cases. Acta Radiol. 2013;54:396-400.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of cardiac and thoracic masses In: Cardiac CT imaging: Diagnosis of cardiovascular disease. London: Springer; 2010. p. :169-85.
- [CrossRef] [Google Scholar]
- CT detection of subendocardial fat in myocardial infarction. Am J Roentgenol. 2009;192:532-7.
- [CrossRef] [PubMed] [Google Scholar]
- The pathophysiology of acute myocardial infarction and strategies of protection beyond reperfusion: A continual challenge. Eur Heart J. 2017;38:774-84.
- [CrossRef] [PubMed] [Google Scholar]
- Differentiation of recent and chronic myocardial infarction by cardiac computed tomography. Am J Cardiol. 2006;98:303-8.
- [CrossRef] [PubMed] [Google Scholar]
- Identifying, characterizing, and classifying congenital anomalies of the coronary arteries. Radiographics. 2012;32:453-68.
- [CrossRef] [PubMed] [Google Scholar]







