Translate this page into:
Emerging insights into cephalic neural crest disorders: A single center experience

*Corresponding author: Shailesh B. Gaikwad, Department of Neuroimaging and Interventional Neuroradiology, All India Institute of Medical Sciences, New Delhi, Delhi, India. sgaikwad_63@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Nayak M, Mishra B, Levejoseph S, Garg A, Sarma K, Sahoo B, et al. Emerging insights into cephalic neural crest disorders: A single center experience. J Clin Imaging Sci. 2024;14:3. doi: 10.25259/JCIS_87_2023
Abstract
Objectives:
Neural crest cells (NCCs) are transient structures in the fetal life in vertebrates, which develop at the junctional site of the non-neural and neural ectoderm, sharing a common developmental origin for diverse diseases. After Epithelio-mesenchymal (EMT) of the NCCs within the neural tube, delamination of NCCs occurs. After delamination, the transformation of these cells into various cell lineages produces melanocytes, bones, and cartilage of the skull, cells of the enteric and peripheral nervous system. After the conversion, these cells migrate into various locations of the entire body according to the cell lineage. Abnormalities in neural crest (NC) formation and migration result in various malformations and tumors, known as neurocristopathy.
Material and Methods:
Herein, this case series describes a single-center experience in cephalic NC disorders over the past 3 years, including 17 cases of varying composition (i.e., vascular, dysgenetic, mixed, and neoplastic forms) involving the brain and occasionally skin, eyes, and face of the patients.
Results:
In our study of 17 patients with cephalic NC disease, 6 (35.3%) patients had vascular form, 5 (29.4%) had dysgenetic form, 4 (23.5%) had mixed form, and 2 (11.7%) had neoplastic form. Brain involvement in the form of vascular or parenchyma or both vascular and parenchymal was seen in all of our patients (100%), skin in 6 (35.3%) patients, eye in 2 (11.7%), and face in 1 (5.9%) patient. Treatment was planned according to the various manifestations of the disease.
Conclusion:
Neural crest diseases (NCDs) are a rare and under-recognized group of disorders in the literature and may have been under-reported due to a lack of awareness regarding the same. More such reporting may increase the repertoire of these rare disorders such that clinicians can have a high degree of suspicion leading to early detection and timely counseling and also improve preventive strategies and help in developing new drugs for these disorders or prevent them.
Keywords
Encephalocraniocutaneous lipomatosis
Dysembryoplastic neuroepithelial tumor
Focal cortical dysplasia
Nevus psiloliparus
Subarachnoid bleed
Neural crest cell
Neurocristopathies
Neural crest derivatives
Neurogenesis
Cephalic neural crest disease
Neural crest migration
INTRODUCTION
Neural crest cells (NCCs) are transient structures in the fetal life in vertebrates, sharing a common developmental origin for diverse diseases. It develops at the junctional site of the surface and neural ectoderm in the late gastrulation and early neurulation period.[1] The formation of the neural crest (NC) is a complex interplay between various embryonic structures, and a sequence of molecular signals and chemical gradients, especially bone morphogenetic protein.[2] After undergoing epithelio-mesenchymal (EMT), delamination NCCs occur and further migration into various locations of the entire body, producing cell lineage of melanocytes, bones, and cartilage of the cranium, cells of the enteric and peripheral nervous system. The types of NCCs are cranial, vagal, trunk, and sacral, corresponding to various locations in the embryonal neuraxis [Figure 1]. The migration of NCCs is presumed to be filopodial extension and retraction and usually follows a specified pattern according to the final cell type present in the body.[3] For example, neurogenic precursors migrate in the medial pathway below the dermomyotome to make their endpoint, which forms the sympathetic ganglia, dorsal root ganglia, and enteric neural system. In contrast, melanocyte precursor cells choose to migrate in a lateral pathway and are finally located in the skin.[4] In the conventional germ layer model, endodermal derivatives are derived from endodermal cells and mesodermal derivatives from mesodermal cells. Although NCCs are an ectodermal derivative, they can be differentiated into mesodermal or endodermal tissues due to EMT[5] and are thus considered the fourth germ layer.[6] Multiple tissues originate from NCCs and are causative factors in many head and neck pathologies. In the present study, we briefly describe the NC derivatives and 17 cases of this rare group of entities (cephalic NC diseases) who presented to our department in the past 3 years.
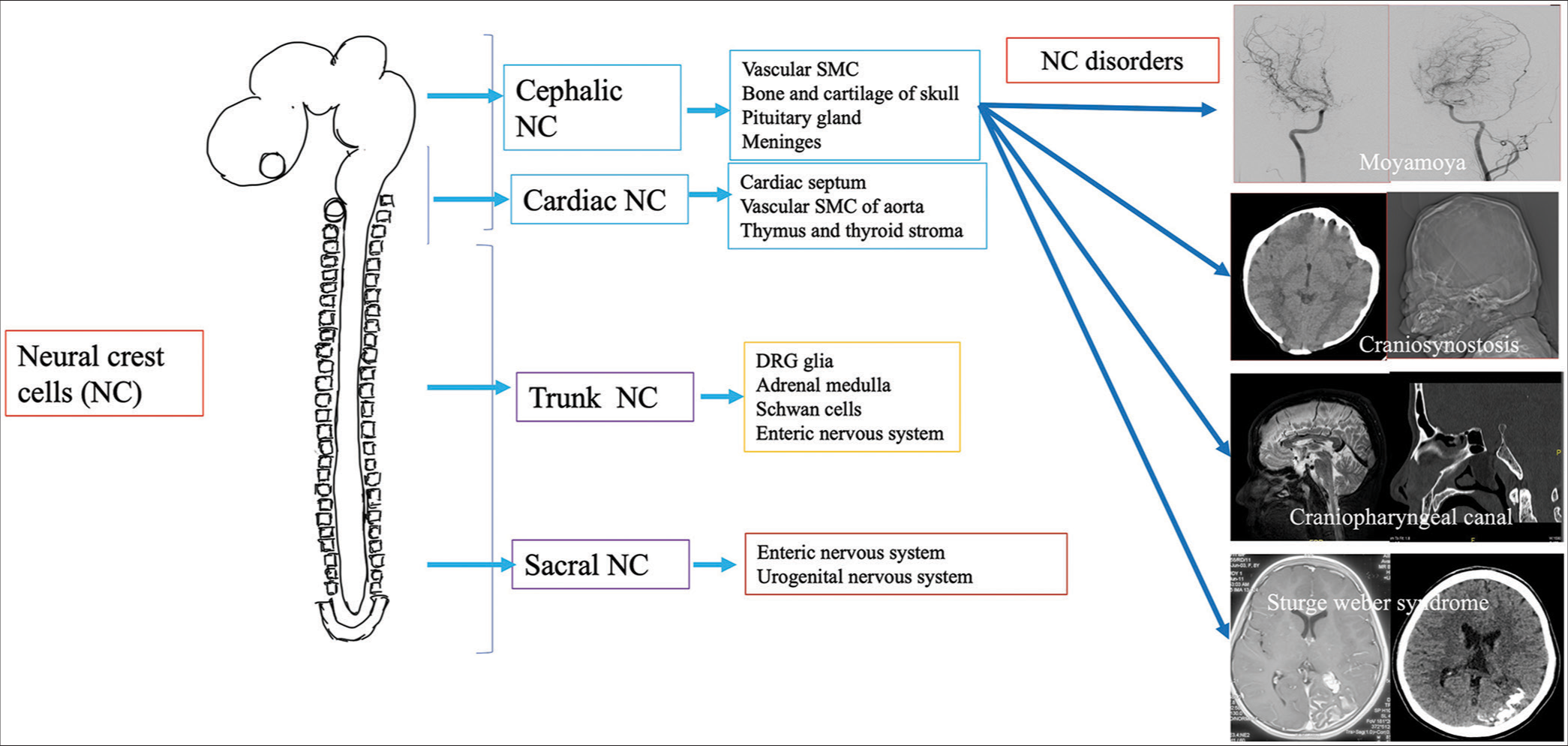
- Schematic illustration of location and migration of neural crest cells (NCC) with their derivatives neural crest (NC) subpopulations have been described in all vertebrate species based on their axial level of origin along the anterior-posterior axis. The first column of the schematic diagram shows the four major subdivisions: Cephalic or cranial, cardiac, trunk, and sacral. The second column of the schematic diagram shows the main NC derivatives contributing to different tissues of the embryo. The third column of the schematic diagram shows some of the diseases associated with cephalic NCCs.
NC DERIVATIVES
NCCs constitute to produce various types of tissues and cells, including cartilage and bone of the face; cells of autonomic, enteric, and peripheral nervous systems; and various organs within the body such as the thyroid gland, heart, eye, and adrenal medulla.[3]
NEUROCRISTOPATHIES (NCPS) CLASSIFICATION
A wide variety of diseases (>50 diseases) are associated with disorders of NCCs, which were discovered mostly after the NC theory by Robert Bolande. As understanding of the NCCs progresses, many unrelated diseases are classified under NCP under a single umbrella-like involvement of endocrine, craniofacial, cardiac, immunologic, dermatologic, and gastrointestinal, neoplastic conditions. NCPs can be classified into dysgenetic form due to defective morphogenesis, neoplasms derived from NCCs, combined dysgenesis, and neoplastic etiology.[7,8] Some authors describe vascular NCP as a distinct entity.[9] From the neuro-interventional radiologist’s perspective, vascular and cranial forms of Neurocristopathies (NCPs) are essential. Understanding pharyngeal arch derivatives is essential as NCCs migrate into pharyngeal arches before the closure of the neural tube in gestational life, developing into structures of the face and neck.[10]
Cranial NCCs predominantly migrate and are located in the first, and second pharyngeal arches and pouches with >30 diseases derived from the cranial NCC are described in the literature.[11] Common diseases include holoprosencephaly, craniosynostosis, Parry Romberg disease, hemifacial microsomia–Goldenhar syndrome spectrum, and Treacher Collin syndrome which are of neuroradiologic importance.
MATERIAL AND METHODS
A retrospective study was conducted at the Neurosciences Centre, All India Institute of Medical Sciences (AIIMS), New Delhi, India. The study encompassed patients diagnosed with neural crest diseases during the period from January 1, 2017, to December 31, 2019. Comprehensive patient clinical information and imaging data were extracted and archived from GE’s Picture Archiving and Communication Software (PACS).
To identify relevant cases, specific keywords such as ‘neural crest cells’ and ‘neurocistopathy’ were employed in the search process. Eligibility criteria were subsequently applied to ensure the inclusion of cases with both imaging records and clinical follow-up information.
Two independent investigators (MKN and KS) conducted a thorough assessment of imaging studies, including computed tomography (CT), magnetic resonance imaging (MRI), and digital subtraction angiography (DSA).
RESULTS
In this three year study duration, seventeen patients were diagnosed with cephalic neural crest disease, revealing distinct manifestations within the cohort. Among the patients, 6 (35.3%) exhibited the vascular form, 5 (29.4%) presented with the dysgenetic form, 4 (23.5%) demonstrated the mixed form, and 2 (11.7%) displayed the neoplastic form. Notably, brain involvement was observed in all patients (100%), manifesting as either vascular, parenchymal, or a combination of both. Skin involvement was identified in 6 (35.3%) patients, while 2 (11.7%) displayed eye involvement, and 1 (5.9%) exhibited facial involvement. Treatment strategies were tailored according to the specific disease manifestations, and the details of these interventions are thoroughly discussed subsequently. In the following section we briefly describe the clinical and radiological findings in these seventeen patients. Additionally, a summary of the salient features of these cases is provided in Table 1 for a clearer understanding of the observed patterns and variations.
| Case with Sl. No. | Age, gender | Age at presentation | Predominant Presenting features | Any other Important Distinguishing Clinical feature | Other Organ Systems Affected apart from CNS | Imaging NCCT MRI | Other imaging | Histolo-gy if any | Genetic Work- up If available |
Final Diagnosis | Type ofNCP | Management | Follow-up Clinical | Follow up-Imaging |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 12 years, female | 12 years | Transient ischaemic attack(TIA) on left side | No | No | Narrowing of both supraclinoid ICAs with collaterals | No | No | No | Moyamoya disease | Vascular | Aspirin | 10 months, no further events | None |
| 2 | 10 years, male | 10 years | TIA on right side | Café au lait macules | Skin | Narrowing of both supraclinoid ICAs with collaterals | No | No | No | Moyamoya syndrome | Mixed | Aspirin | 1 year, one TIA in same territory, planned for ECA-MCA bypass | No |
| 3 | 25 years, female | 23 years | Reddish cutaneous lesion with pulsatile lesion in right upper neck | Reddish cutaneous lesion | Skin | Multiple flow voids from right ECA | No | No | No | AVM with cutaneous patch | Mixed | No | Planned for embolization | No |
| 4 | 42 years, male | 37 years | Migraine, TIA | No | No | White matter hyperintensities, lacunar infarcts | No | No | No | CADASIL | Vascular | Symptomatic | Clinically better o 6 months | No |
| 5 | 5 years, female | 5 years | Stroke in right MCA | No | No | Narrowing both supraclinoid ICAs with straightened vessel and paucity of collaterals | No | No | No | ACTA2 mutation | Vascular | aspirin | 1 year, no further events | No |
| 6 | 48 years male | 48 years | Headache, transient Wernicke aphasia | No | No | Multiple dilated arteries, without draining veins | No | No | No | Pure arterial malformations(PAM) | Vascular | Symptomatic | 10 months, improvement in symptoms | No |
| 7 | 15 years, male | 15 years | Headache, syncope | No | No | Focal non visualization of ophthalmic segments of both ICAs | No | No | No | Segmental dysgenesis of ICAs | Vascular | Aspirin | 1 year, clinically better | No |
| 8 | 55 years male | 55 years | Headache, LOC | Decreased vision in right eye | Eye | Focal bleed in right temporal lobe with AVM | No | No | No | CAMS2 | Vascular | Conservative | 2 years, asymptomatic | No |
| 9 | 12 years, male | 2 years | Left side facial atrophy | Skin | Skin | Atrophy of facial muscles | No | No | No | Parry Romberg disease | Dysgenetic | Conservative | 10 months, clinically stable | No |
| 10 | 10 years female | 7 years | Seizure, left side facial hemangioma | Hemangioma | Skin | Cortical calcifications with angiomas | No | No | No | Sturge weber syndrome(SWS) | Mixed | Antiepileptics | 10 months, no further seizure | No |
| 11 | 13 years, male | 1 year | Seizure, left upper limb weakness | Alopecia | Skin | Cortical calcification, fatty lipoma and pial angiomas | No | Yes | No | Encephalocraniocutaneous lipomatosis syndrome(ECCL) | Mixed | Surgery | 2 years, no seizure following surgery | Yes |
| 12 | 10 months, female | 1 month | Right fronto-temporal swelling | No | No | T1 hyperintense lesion with enhancement | No | Yes | No | Melanotic neuroectodermal tumor of infancy (MNTI) | Neoplastic | Surgery | 8 months chemotherapy for 2 months after surgery, died due to recurrence | Yes |
| 13 | 42 years male | Birth | Decreased vision in both eyes, headache, epistaxis | Vision loss | Eye | Persistent craniopharyngeal canal with encephalocele and lipoma, right pthisis bulbi, left globe calcification | No | No | No | Persistent craniopharyngeal canal, vertebrobasilar dolichoectasia, ? morning glory | Dysgenetic | Planned for encephalocele repair | No | No |
| 14 | 12 years female | Birth | Abnormal skull shape with facial dysmorphism | Face | Face | Brachycephaly with sutural fusion | No | No | No | Craniosynostosis | Dysgenetic | Planned for mesh placement following decompression | No | No |
| 15 | 10 years male | 3 months | Seizure and hypopigmentation | Hypopigmentation in trunk | Skin | Focal abnormal thickened cortex | No | No | No | Hypomelanosis of Ito | Dysgenetic | antiepileptics | 6 months, seizure free | No |
| 16 | 41 years male | 40 years | Gait disturbance and quadriparesis | No | No | T1 hyperintense lesion in pons | No | Yes | No | Melanocytoma | Neoplastic | Surgery | 6 months, improvement in gait | Yes |
| 17 | 6 months | Birth | Development al delay and facial dysmorphism | Face | Face | Single cerebral hemisphere with monoventricle | No | No | No | Holoprosencephaly | Dysgenetic | Conservative | Static, 6 months | No |
TIA: Transient ischaemic attack, MCA: Middle cerebral artery, LOC: Loss of consciousness, ICA: Internal carotid artery, ECA: External carotid artery, AVM: Arterio-venous malformation, CADASIL: Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy, ACTA2: Gene, CAMS: Cerebrofacial arteriovenous metameric syndrome
CASE 1
A 12-year-old female child presented with sudden-onset left-side weakness for 1 day, which improved within the next 24 h. There was a history of a similar episode 3 months back, which recovered within 3 days. At the presentation, she had recovered almost fully and was conscious and oriented without any cranial nerve abnormality and normal tone and power and sensory system examination. Magnetic resonance imaging (MRI) brain showed T2/fluid-attenuated inversion recovery hyperintensity in the sulcal space suggestive of Ivy sign, and digital subtraction angiography (DSA) revealed narrowing of both supraclinoid internal carotid arteries (ICAs) and multiple basal and pial collaterals suggestive of Moyamoya disease [Figure 2a-f]. She was started on aspirin and had no further incidence of stroke or transient ischemic attack with 10 months of follow-up duration.
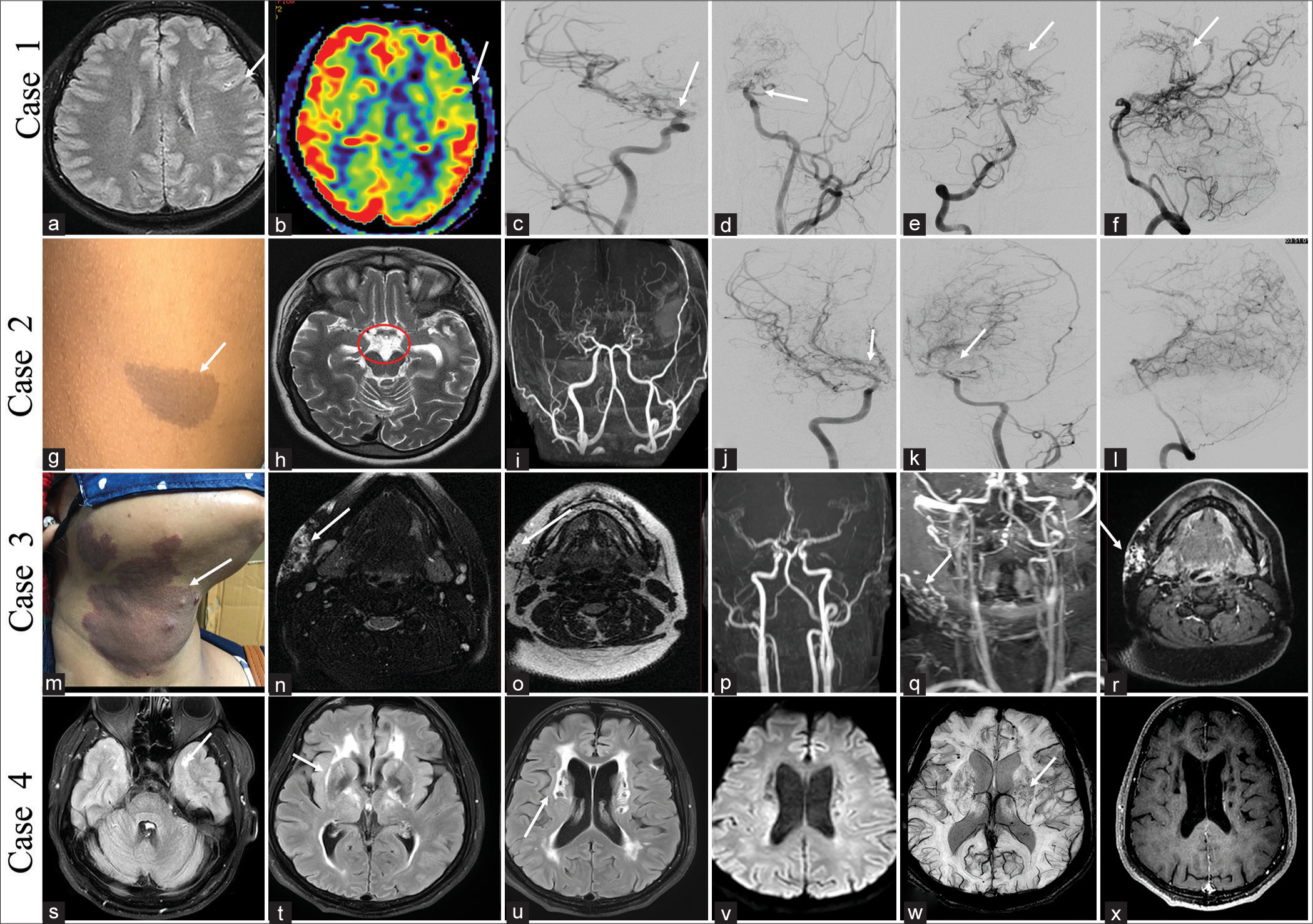
- Case 1 – A 12-year-old female child with Moyamoya disease presented with left-side weakness. (a-f): Magnetic resonance imaging (MRI) (a and b): Fluid-attenuated inversion recovery (a) showed leptomeningeal collaterals (white arrow) and perfusion deficits (white arrow) in the left frontal lobe on arterial spin labeling image (b). Digital subtraction angiography (DSA) image (c-f), right common carotid artery (CCA) (c), and left CCA (d) showed narrowing of both supraclinoid internal carotid arteries (ICAs) (white arrows) with multiple basal collaterals and right vertebral artery (VA) (e and f) showing multiple leptomeningeal and pial collaterals reforming middle cerebral artery (MCA) and anterior cerebral artery (ACA) branches (white arrows). Case 2 – A 10-year-old male child with Moyamoya syndrome presented with right side weakness. (g-l) Clinical image (g) showed café-au-lait macule (white arrow), MRI image (h) multiple basal collaterals (red circle) and time of flight circle of Willis (i) showed narrowing of both supraclinoid ICAs with basal collaterals. DSA image (j-l): Right CCA (j) and left CCA (k) showed narrowing of both supraclinoid ICAs with multiple basal collaterals (white arrows) and right VA (l) showed multiple leptomeningeal and pial collaterals reforming MCA and ACA branches. Case 3 – A 25-year-old female with arteriovenous malformation (AVM) presented with swelling in the right side upper neck. (m-r): Clinical image (m) showed a melanotic patch in the right cervical region (white arrow). MRI image (n-r): Axial T2 (n), T1 (0) image showed multiple abnormal dilated vessels (white arrows). Time-of-flight images (p) and CRMRA (q) showed multiple dilated vessels on the right side of the neck, likely AVM (white arrow). Postcontrast T1 (r) showed focal enhancement within the lesion (white arrow). Case 4 – A 42-year-old male with cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy presented with a headache. MRI brain (s-x): Axial fluid-attenuated inversion recovery (s-u), diffusion-weighted imaging (v), susceptibility-weighted imaging (w), T1PC (x) showed multiple lacunar infarcts (white arrows in t,u), white matter changes (white arrows in s,t,u), predominantly in the anterior temporal lobe, external capsule and microbleeds in basal ganglia (white arrow).
CASE 2
A 10-year-old boy presented with acute right-sided weakness of 3 days duration, which improved completely over 24 h. No history of similar attacks in the past. Examination revealed multiple café-au-lait macules over the trunk and plexiform neurofibroma over the right eyelid. MRI brain showed multiple collaterals in the basal cistern, and a time-of-flight (TOF) image of the circle of Willis (COW) showed narrowing of both supraclinoid ICAs with multiple basal collaterals. DSA showed narrowing of both supraclinoid ICAs and multiple basal and pial collaterals suggestive of Moyamoya syndrome [Figure 2g-l]. He was started on aspirin and one episode of same-sided stroke during 1 year of follow-up. He is planning for external carotid artery (ECA)-middle cerebral artery (MCA) bypass surgery from the neurosurgery side.
CASE 3
A 25-year-old female without comorbidities presented with swelling over the right upper neck for 2 years. On examination, a reddish patch was seen over that region since birth which was warm on the touch. The swelling was pulsatile, firm in its consistency, and warm. MRI of the neck showed multiple abnormal vessels with nidus in the right upper side of the neck with supply from the ECA, likely suggestive of arteriovenous malformation (AVM) [Figure 2m-r]. She underwent DSA followed by embolization of the AVM.
CASE 4
A 42-year-old male without comorbidities presented with a headache suggestive of migraine for the past 5 years. He also had recurrent transient ischemic attacks in the left MCA territory for 1 year. MRI brain showed white matter changes, predominantly in the anterior temporal pole and external capsule, chronic lacunar infarcts, and microbleeds consistent with cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) [Figure 2s-x]. He was managed conservatively and was clinically stable at 6 month follow up.
CASE 5
A 5-year-old girl presented a history of acute onset-left hemiparesis 3 months back, which partially recovered within 3 days. No similar complaint was seen before. Birth and developmental histories were normal. MRI brain and DSA images showed chronic infarct in the right anterior external watershed region with narrowing of both supraclinoid ICAs without significant collaterals and straightening of vessels, consistent with ACTA2 mutation [Figure 3a-f]. ACTA2 is a non-atherosclerotic cerebral arteriopathy which can involve multisystem smooth muscle due to Arg179His mutations. Angiographic features include ectasia and stenosis of vessels, a straight arterial course, and absence of basal collaterals.
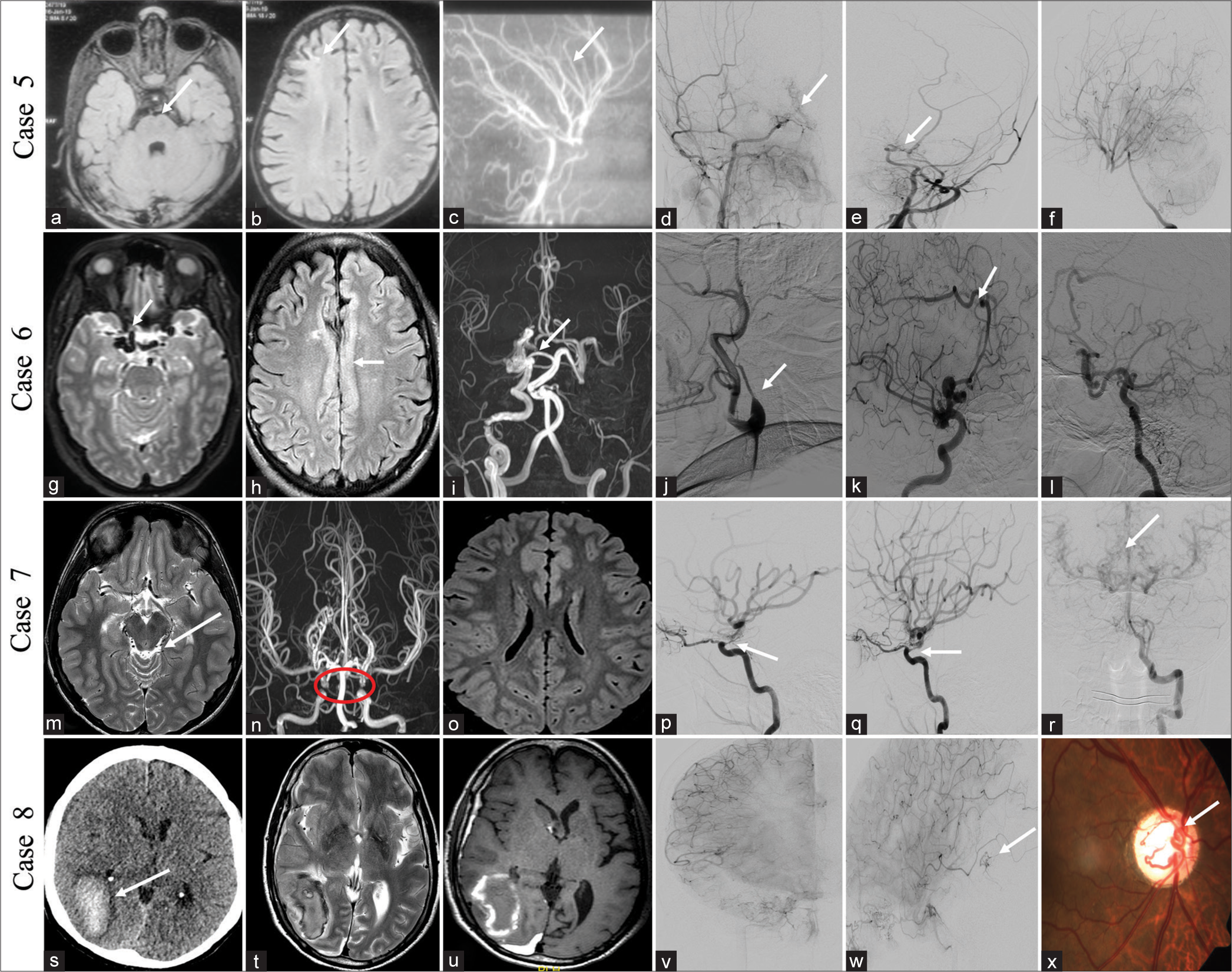
- Case 5 – A 5-year-old female child with ACTA2 mutation presented with the left- side weakness. Magnetic resonance imaging (MRI) (a-c): Axial fluid-attenuated inversion recovery (FLAIR) (a and b) showed basilar artery indentation over pons and chronic infarct in the right anterior watershed territory (white arrows). Time-of-flight (TOF) circle of Willis (COW) (c) showed a straightened appearance of the posterior cerebral artery (PCA) branches (white arrow). Digital subtraction angiography (DSA) image (d-f): Right common carotid artery (CCA) (d) and left CCA (e) showed narrowing of both supraclinoid internal carotid arteries (ICAs) with few basal collaterals (white arrows) and left vertebral artery (VA) (f) showed straightened appearance of the PCA branches. Case 6 – A 48-year-old male with pure arterial malformation presented with headache and transient Wernicke aphasia. MRI image (g-i): Axial T2 (g) image showed multiple abnormal dilated vessels in the right supraclinoid ICA (white arrow) and axial FLAIR (h) showed pachygyria over the cingulate cortex (white arrow). TOF COW (i) showed dilated right supraclinoid ICA and right pericallosal artery without abnormal veins and non-visualization of left ICA (white arrow). DSA image (j-l): Left CCA (j) run showed non-visualization of left ICA (white arrow) and used it as an ascending pharyngeal artery. Right CCA lateral (k) showed abnormally dilated arteries in the right supraclinoid ICA, pericallosal artery with aneurysm without abnormal draining vein (white arrow), and right VA (l) showing multiple collaterals and filling of the left middle cerebral artery (MCA) through the left posterior communicating artery. Case 7 – A 15-year-old male with bilateral segmental dysgenesis of ICA presented with a headache and one episode of loss of consciousness. MRI image (m-o): Axial T2 (m) image showed multiple abnormal dilated vessels in the quadrigeminal cistern (white arrow). TOF COW (n) showed focal non-visualization of the ophthalmic segment of both ICAs (red circle). FLAIR (o) showed no obvious abnormality. DSA image (p-r): Left CCA (p), and right CCA (q) showed focal dysgenesis of the ophthalmic segments of both ICAs (white arrows in p,q) and left VA (r) showing multiple pial collaterals reconstituting MCA and ACA branches (white arrow). Case 8 – A 55-year-old male with cerebrofacial arteriovenous metameric syndrome (CAMS) type 2 presented with headache, vomiting, and loss of consciousness. Non-contrast computed tomography (NCCT) head (s), MRI brain (s-w): Axial T2 (t), T1 (u), showed focal bleed in the right posterior temporal lobe (white arrow). DSA image AP (v) and lateral (w) showed arteriovenous malformation (AVM) in the right posterior temporal lobe with feeder from the right posterior temporal artery and drainage into a vein of Labbe (white arrow). Fundoscopy (x) showed retinal AVM (white arrow). Features are suggestive of CAMS2.
CASE 6
A 48-year-old male without comorbidities presented with intermittent headache, once every month without aura, forgetting names, and irrelevant talk (transient Wernicke aphasia), recovered fully in 4 days. MRI brain findings showed multiple dilated vessels near the right supraclinoid ICA and right pericallosal artery without early draining veins and pachygyria in the underlying cingulate cortex. The DSA images showed a dilated arterial system in the right ICA and right pericallosal artery without abnormal early draining veins suggestive of pure arterial malformations (PAMs). A note was made of the non-visualization of the left ICA from its origin and replaced with an ascending pharyngeal artery [Figure 3g-l]. The patient was managed conservatively and symptomatically improved on 4-months follow-up.
CASE 7
A 15-year-old male presented with an intermittent headache for 1 year which was non-pulsatile, frequency of 15 days duration, without aura, and one episode of loss of consciousness (LOC) lasting for 1 h, 5 days back (syncope). Two episodes of slurring of speech and weakness in the right upper limb 10 days prior to presentation, which improved completely over the next 10 hours. His birth and developmental history are unremarkable. MRI image showed multiple abnormal dilated vessels in the quadrigeminal cistern without any signal changes in the brain parenchyma. The TOF image of COW revealed focal non-visualization of the ophthalmic segment of both ICAs. The DSA image showed focal dysgenesis of the ophthalmic segments of both ICAs and multiple pial collaterals reconstituting MCA and ACA branches from the vertebral artery with the diagnosis of segmental dysgenesis of ICAs [Figure 3m-r]. He was managed conservatively with antiplatelets and symptomatic treatment for headache, clinically better with a follow-up duration of 1 year.
CASE 8
A 55-year-old male without any previous comorbidities presented with an abrupt onset severe headache associated with one episode of vomiting and loss of consciousness for 15 min. On fundoscopy, an AVM was seen in the retina of the right eye. Non-contrast computed tomography (NCCT) head and MRI brain showed right temporo-occipital lobe subacute hematoma, and DSA showed small AVMs right posterior temporal lobe, fed by a posterior temporal branch of right ICA [Figure 3s-x]. A combination of these findings suggests cerebrofacial arteriovenous metameric syndrome (CAMS) type 2. He underwent conservative management and was doing well till a 2-years follow-up.
CASE 9
A 12-year-old boy presented with progressive left-side facial atrophy since the age of 2 years. His birth and developmental history was normal. No history of seizures or numbness over his face. Clinical examination and MRI showed facial muscle atrophy in the left side without brain parenchymal changes [Figure 4a-f]. The above findings are consistent with Parry-Romberg disease. The patient was managed conservatively and asked for a follow-up.
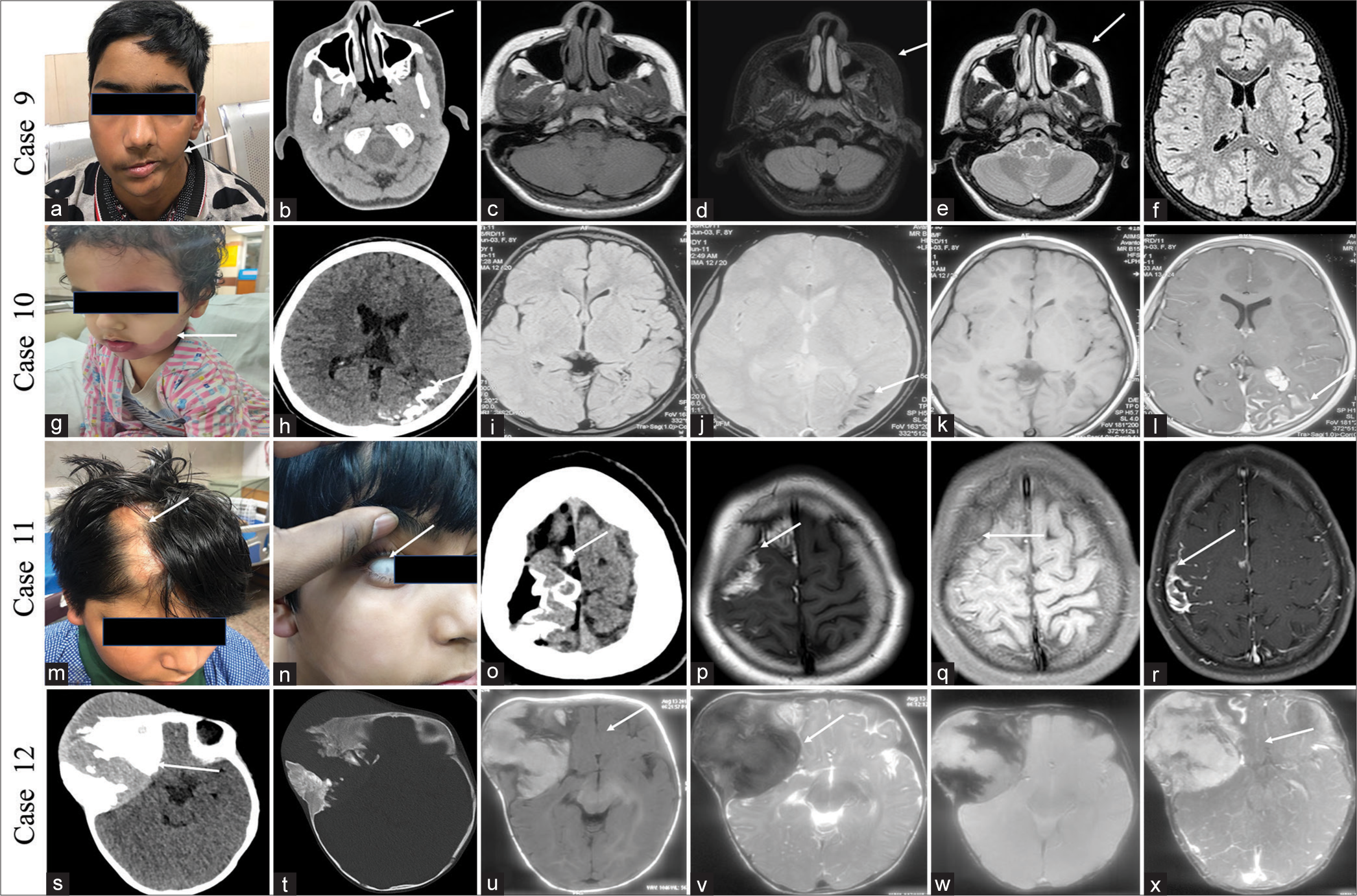
- Case 9 – A 12-year-old male with Parry-Romberg disease presented with progressive left-side facial muscle atrophy. (a-f): Clinical image (a) showed atrophy of the left side facial musculature (white arrow). Non-contrast computed tomography (NCCT) scan (b) showed atrophy of the left side muscles of the face (white arrow). Magnetic resonance imaging (MRI) image (c-f): Axial T1 (c), T1FS (d), T2 (e), fluid-attenuated inversion recovery (FLAIR) (f) image showed atrophy of the left side facial muscles and without any signal changes in brain parenchyma (white arrows). Case 10 – A 10-year-old female with Sturge-Weber syndrome presented with seizure (g-l): Clinical image (g) showed hemangioma on the left side of the face (white arrow). NCCT head (h) showed gyriform calcifications in the left parieto-occipital lobe (white arrow). MRI image (i-l): Axial FLAIR (i), gradient-echo (GRE) (j), T1 (k), and T1PC (l) images showed gyriform calcifications with pial angiomas (white arrows). Case 11 – A 13-year-old male with encephalocraniocutaneous lipomatosis presented with a seizure. (m-r): Clinical images (m and n) showed non-scarring alopecia and a focal conjunctival lesion in the right eye (white arrows). The non-contrast NCCT head (o) showed gyriform calcifications on the right superior frontal lobe with adjacent lipoma (white arrow). MRI image (p-r): Axial T1 (p), T1FS (q) showed lipoma showing fat suppression (white arrows). T1PC (r) image showed gyriform calcifications with pial angiomas (white arrow). Case 12 – A 10-month-old male with melanotic neuroectodermal tumor of infancy (MNTI) presented with gradual progressive swelling of the right forehead. NCCT head (s and t) showed a large mass lesion with lytic changes in the skull in the right frontal region (white arrow). MRI brain (u-x): Axial T1 (u), T2 (v) showed T1 hyperintensity and T2 hypointensity within the lesion (white arrows), and GRE (w) showed peripheral blooming within the lesion (white arrow). T1PC (x) showed enhancement within the lesion. The biopsy showed a melanocytic tumor with a diagnosis of MNTI.
CASE 10
A 10 year female child presented with 1 episode of generalized tonic-clonic seizure for 1 day. She had suffered a similar episode 3 years ago. Examination revealed a reddish swelling over the left side of the face since birth. The NCCT head showed gyriform calcifications in the left parieto-occipital lobe, and the MRI image showed gyriform calcifications with pial angiomas, consistent with Sturge-Weber syndrome [Figure 4g-l]. She was on two antiepileptics and seizure-free for a 10-month duration.
CASE 11
A 13-year-old boy presented with multiple episodes of seizure from 1 year of age and left upper limb weakness for 6 months. He was born of full-term normal vaginal delivery and cried immediately after birth. No history of consanguinity or neurocutaneous manifestations in the family. No history of similar illness in his siblings. Examination revealed patchy hair loss on the right side of the scalp, which has been there for the past 10 years. There was also mild mental retardation. MRI brain showed lipoma with gyriform cortical calcifications in the right superior frontal lobe in both T1, T1 fat saturated, and susceptibility-weighted images. Findings were consistent with the syndrome of encephalocraniocutaneous lipomatosis [Figure 4m-r]. He underwent excision of the lesion, and histopathology showed loss of loss of normal layering with the haphazard arrangement of neurons and fibroadipose tissue. He was seizure-free 2 years after surgery with one antiepileptic.
CASE 12
Ten-month-old female child presented with swelling near the right side of the forehead for 9 months, gradually increasing in size. She was born through a full term normal vaginal delivery, cried immediately after birth, and had a normal birth and developmental history. She was having sequential loss of vision in the right eye, followed by the left eye over 6 months. Examination revealed a hard soft-tissue lesion in the right frontotemporal location. Clinical examination and X-ray of the chest revealed no abnormality. Similarly, clinical and ultrasonography examination of the abdomen revealed no abnormality. NCCT head and brain MRI showed a mixed lytic and sclerotic lesion on computed tomography (CT) and T1 hyperintense lesions with post-contrast enhancement in the right frontal and temporal scalp region [Figure 4s-x]. A biopsy of the lesion showed a melanotic neuroectodermal tumor of infancy (MNTI). Seven cycles of neoadjuvant chemotherapy were given to the child (actinomycin D at 0.5 mg, vincristine at 0.7 mg, and cyclophosphamide at 450 mg) over 2 months. The child died 8 months following surgery due to the recurrence of the tumor.
CASE 13
A 42-year-old male presented with an intermittent headache for the past 10 years and two episodes of epistaxis within the previous 3 years. He is blind in the right eye from birth with the perception of light and decreased vision in the left eye with hand movement positive in the left eye. No history of trauma was present. On examination, the patient was of short stature. His blood cortisol level was low (4.6 μg/dL), and his thyroid-stimulating hormone level was high (7.9 mIU/L). NCCT scan of the brain showed a defect in the floor of the sella with persistent craniopharyngeal canal (CPC) with the right eye phthisis bulbi and left eye choroidal calcification. MRI of the brain showed transsellar encephalocele through persistent CPC, communicating into the nasopharynx, with lipoma near the nasopharynx (type 3c CPC) and thinning of both optic nerves. Left optic nerve head funneling was seen. TOF COW showed dolichoectatic changes in the vertebrobasilar system without a Moyamoya pattern [Figure 5a-e]. He underwent repair of the encephalocele in the department of neurosurgery.
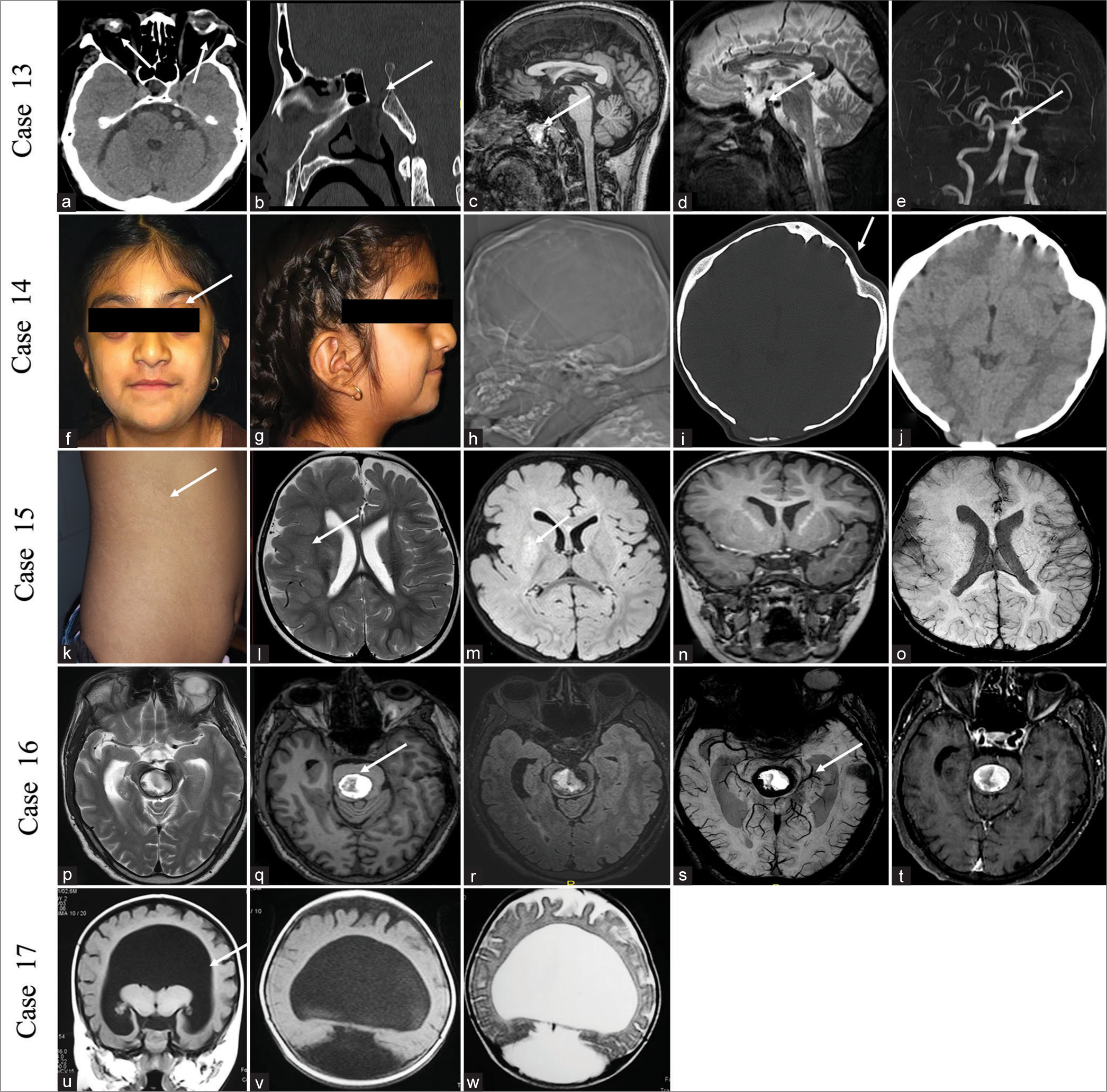
- Case 13 – A 42-year-old male with persistent craniopharyngeal canal (CPC) presented with a headache. Non-contrast computed tomography (NCCT) scan of the head (a and b) showed right phthisis bulbi, left globe calcification with globe deformation, and persistent CPC (white arrows). The magnetic resonance imaging (MRI) brain (c-e) showed transsellar encephalocele with lipoma in the nasopharynx and dolichoectatic changes in the vertebrobasilar system on the time of flight circle of Willis (e) (white arrows). Case 14 – A 12-year-old female with craniosynostosis presented with an abnormal skull shape. (f-j): Clinical images (a and b) showed abnormal skull shape with prominent eyeballs (white arrow). The NCCT head (h-j) showed an abnormal skull shape with shallow orbits (white arrow). Case 15 – A 10-year-old male with Hypomelanosis of Ito presented with focal seizure. (k-o): Clinical image (k) showed hypopigmented macules in the trunk along the line of Blaschko (white arrow). MRI image (l-o): Axial T2 (l), fluid-attenuated inversion recovery (FLAIR) (m), Coronal T1 (n), susceptibility-weighted imaging (SWI) (o) showed focal abnormal thickened cortex with white matter signal changes and paucity of vessels in the right frontotemporal lobe and right hemimegalencephaly (white arrow). Case 16 – A 41-year-old male with melanocytoma presented with difficulty in walking. MRI brain (p-t): AxialT2 (p), T1 (q), FLAIR (r), SWI (s), T1PC (t) showed well-defined focal T1 hyperintense lesion with peripheral blooming on SWI in the central aspect of the pons (white arrows). Blooming is less evident as compared to T1 hyperintensity. Case 17 – A 6-month male child with alobar holoprosencephaly presented with developmental delay. MRI image (u-w): Coronal T1 (u), Axial T1 (v), and T2 (w) images showed monoventricle with fused thalami and single hemisphere (white arrow).
CASE 14
A 12-year-old girl presented with an abnormal skull shape from birth (brachycephaly). Clinical evaluation showed outward protrusion of eyeballs with abnormal skull shape. CT scan showed an abnormal skull shape with reduced antero-posterior (AP) diameter of the skull (brachycephaly) and sutural fusion suggestive of craniosynostosis [Figure 5f-j]. She underwent vault surgery in the department of Neurosurgery.
CASE 15
A 10-year-old boy presented with recurrent left-sided focal seizures since 3 months of age. Examination revealed hypopigmented lines over the skin, present along the lines of Blaschko. MRI brain showed a focal abnormal thickened cortex with white matter signal changes in the right frontotemporal lobe. Findings are suggestive of Hypomelanosis of Ito Hypomelanosis of Ito (HI) [Figure 5k-o]. He was managed with antiepileptics and seizure-free for 6 months duration of follow-up.
CASE 16
A 41-year-old male without any comorbidities presented with difficulty in walking and progressive weakness in bilateral upper and lower limbs for 1 year. He also complained of one episode of slurring of speech 10 days back, which improved completely within 24 h. MRI brain showed a well-defined T1 hyperintense lesion with peripheral blooming in the central aspect of the pons [Figure 5p-t]. An excisional biopsy of the lesion showed melanocytoma. The patient was followed up for 6 months and showed improvement in power in all four limbs with improvement in his gait.
CASE 17
A 6-month-old male child presented with a history of global developmental delay and facial dysmorphism (ocular hypotelorism). MRI image showed non-separation of both cerebral hemispheres with monoventricle and partially fused thalami suggestive of alobar holoprosencephaly [Figure 5u-w].
DISCUSSION
The NCCs are divided into different types according to their location with their specific derivatives and functions.[3] The cephalic NC develops into the cranial and facial skeleton, including the skull, hypobranchial skeleton, jaws (both upper and lower), adenohypophysis, carotid body, and eye tissues. Cephalic NCCs can produce pericytes and smooth muscle cells (SMCs) of cerebral and facial arteries in the forebrain.[12] However, cardiac NC is located within cephalic NC, which extends from the otic region to the 3rd somite, forming tunica media of the great vessels, coronary arteries, and the aorticopulmonary septum.[12] Thus, abnormal cephalic and cardiac NCCs may result in vascular lesions in Moyamoya disease, PHACE syndrome, and ACTA2 mutation syndrome.
During embryonic development, ICA divides into caudal and rostral segments at the posterior communicating artery (PCom). The caudal division involves Pcom and the first segment (P1) of the posterior cerebral artery (PCA) and rostral division constituting ICA and its distal branches after Pcom. However, the distal PCA branches (P2-4) develop from distal annexation between P1 PCA and telencephalic segments of the anterior choroidal artery.[13] According to Lasjaunias, the distal basilar artery after the primitive trigeminal artery is considered to be the caudal division of ICA, and hence, the embryological boundary between both posterior and anterior circulations is located between the superior cerebellar artery and PCA. A similar observation was seen in our cases 1, 2, and 5, where anterior circulation was observed with relative sparing of the posterior circulation.
Cephalic NC constitutes tunica media of arteries of the anterior circulation, while the posterior circulation originates from the mesoderm. However, the endothelium is derived from the mesoderm in all vessels within the body, including cerebral vasculature. For this reason, Moyamoya disease, PHACE syndrome, ACTA2 mutation, and preferential involvement of anterior circulation with sparing of the posterior circulation.[14] ICA develops from seven different segments between carotid bifurcation and Pcom based on primitive arteries as a segmental concept by Lasjaunias.[15] Multiple spectrums of segmental pathologies may be regression, agenesis, duplication, fenestration, dysplasia, stenosis, looping, rete formation, and dolichoectasia. In one of our cases (case 7), we have seen segmental dysgenesis of bilateral ICA where abnormal NC migration resulted in segmental lesions in ICA.[13]
Pure arterial malformations (PAMs) are arterial malformations described as abnormally dilated and tortuous vessels producing a coil-like configuration without having an early draining vein. The most accepted mechanism for PAM is due to arterial dysplasia caused by a congenital defect or an insult by Brinjikji et al.[16] PAM can be linked with focal cortical dysplasia, corpus callosal dysgenesis, and hemimegalencephaly as arterial development is believed to be influenced by underlying brain development.[17]
Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) develops due to an abnormal mutation in the NOTCH3 gene, which resulted in vascular smooth muscle cells (VSMCs), and pericyte degeneration.[18] VSMC is presumed to be of NCC origin, and the Notch gene is responsible for NC differentiation during the cardiovascular system and smooth muscle development.[19]
CAMS is characterized by unilateral cerebral and facial involvement with the medial, lateral prosencephalic group, and lateral rhombencephalic groups.[20] Previous avian studies suggested NCCs and mesodermal cells develop at a single metameric level and migrate into similar regions of the ace and brain, primarily due to hox genes, which are responsible for the segmentation of rhombencephalon and migration of NCCs.[21]
Melanotic neuroectodermal tumor of infancy (MNTI) is a very rare neoplastic lesion with NC percussor and usually presents within 1 year of life.[22] On imaging, these tumors show T1 hyperintensity and T2 hypointensity due to the paramagnetism effect of melanin. Multiple genes such as SHH and ZIC2, which help in the separation of the prosencephalon and the development of facial musculature are believed to be regulated by the NC, resulting in holoprosencephaly.[23] Similarly, different genes such as TWIST and FGF, which regulate the NC-derived mesenchymal tissue, are responsible for the development of craniosynostosis.[24] As adenohypophysis development depends on the NC, there may be an association of the persistent CPC with hypopituitarism, morning glory syndrome, and Moyamoya syndrome.[25] Similarly, we have one case where there is CPC with optic nerve hypoplasia and calcification of the globe with optic nerve hypoplasia.
Neurocutaneous syndromes are a distinct group of diseases that involve abnormalities of both the cerebrum and skin.[26] Abnormalities associated with angiogenesis and NCC derivatives including neuronal tissues (both peripheral and autonomic), adipose tissue, melanocyte precursor, and chromaffin cells are common features in neurocutaneous syndrome. Pigmentation abnormality can occur along the lines of Blaschko, which is thought to be the migratory pathways of melanocytic precursors.[26] Neurofibromatosis 1 (NF1) is an autosomal dominant disorder due to germline mutations in the NF1 gene located at chromosome 17, which suppress the RAS proto-oncogene.[27] NF1 contains neurofibromas and other melanocytic abnormalities (e.g., Lisch nodules, skinfold freckling, and café-au-lait macules), and vascular diseases like Moyamoya syndrome have resulted from abnormalities of NCCs.[28] Tumors related to NC in NF1 patients are malignant peripheral nerve sheath tumors, pheochromocytomas, and non-NC tumors such as glioblastomas and optic gliomas develop due to deactivation of the tumor suppressor effect of the NF1 gene.[29]
Meningiomas and schwannomas of NF2 are associated with NC origin, while ependymomas are non-NC origin. Pigmentation anomalies (hypomelanotic macules and shagreen patches), angiofibromas, angiomyolipomas, and fibromas of TS are NC origin, whereas hamartomas, and Subependymal giant cell astrocytoma( SEGA), are nonNC origin. Vascular malformations of meninges and skin are NC derivatives in the case of Sturge-Weber syndrome. Angiomatosis, hemangioblastomas, pheochromocytomas, and paragangliomas of von Hippel-Lindau are of NC origins. Renal cell carcinomas, pancreatic cysts, and Endolymphatic Sac Tumors (ELSTs), are non-NC origin.[10] Hypomelanosis of Ito (HI) is a rare neurocutaneous syndrome involving skin hypopigmentation along the line of Blaschko with brain involvement, including abnormal cortical lamination, laminar or band heterotopia, polymicrogyria, pachygyria, abnormal neurons in the periventricular region, and white matter, which are presumed to be abnormal germinal matrix formation and abnormal migration of the neurons.[30] Embryologically, melanoblast derivative from the NC and cortical neuronal migration share a common pathway for the involvement of both the brain and skin.[31]
CONCLUSION
The NCCs play a central role in the pathogenesis of various malformation syndromes, congenital birth abnormalities, and tumors. A basic understanding of the concept of neural crest diseases can guide the correlation of seemingly unrelated diseases under a single umbrella, which share a common etiopathogenesis. One ICA may be involved in early cases, and later, there may be involvement of the contralateral ICA. Hence, understanding this disease may preserve the ICA and can avoid intervention. The multipotency and plasticity of NCCs will have promising prospects for treating various NCPs in the future involving stem cell manipulation, cell reprogramming, and gene therapy. Radiologists will have a significant role in the detection of various types of NCPs, and hence, radiologists are an integral part of the team for diagnosis, management, and follow-up of these patients.
Ethical approval
The research compiled with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Development and evolution of the neural crest: An overview. Dev Biol. 2012;366:2-9.
- [CrossRef] [PubMed] [Google Scholar]
- Reiterated Wnt signaling during zebrafish neural crest development. Development. 2004;131:1299-308.
- [CrossRef] [PubMed] [Google Scholar]
- The neural crest: A versatile organ system. Birth Defects Res Part C Embryo Today. 2014;102:275-98.
- [CrossRef] [PubMed] [Google Scholar]
- Review: The role of neural crest cells in the endocrine system. Endocr Pathol. 2009;20:92-100.
- [CrossRef] [PubMed] [Google Scholar]
- Cranial neural crest cells on the move: Their roles in craniofacial development. Am J Med Genet A. 2011;155A:270-9.
- [CrossRef] [PubMed] [Google Scholar]
- The neural crest as a fourth germ layer and vertebrates as quadroblastic not triploblastic. Evol Dev. 2000;2:3-5.
- [CrossRef] [PubMed] [Google Scholar]
- Insights into neural crest development and evolution from genomic analysis. Genome Res. 2013;23:1069-80.
- [CrossRef] [PubMed] [Google Scholar]
- Letter: The neurocristopathies: A unifying concept of disease arising in neural crest development. Hum Pathol. 1975;6:128.
- [Google Scholar]
- Cardio-cephalic neural crest syndrome: A novel hypothesis of vascular neurocristopathy. Interv Neuroradiol. 2017;23:572-6.
- [CrossRef] [PubMed] [Google Scholar]
- Neurocristopathies: Enigmatic appearances of neural crest cell-derived abnormalities. Radiographics. 2019;39:2085-102.
- [CrossRef] [PubMed] [Google Scholar]
- Neurocristopathies: New insights 150 years after the neural crest discovery. Dev Biol. 2018;444(Suppl 1):S110-43.
- [CrossRef] [PubMed] [Google Scholar]
- The cephalic neural crest provides pericytes and smooth muscle cells to all blood vessels of the face and forebrain. Development. 2001;128:1059-68.
- [CrossRef] [PubMed] [Google Scholar]
- Segmental vulnerability and vascular neurocristopathy of the internal carotid artery. Interv Neuroradiol. 2020;26:131-4.
- [CrossRef] [PubMed] [Google Scholar]
- Moyamoya disease is a vascular form of neurocristopathy: Disease of the embryologic cephalic neural crest. Childs Nerv Syst. 2017;33:567-8.
- [CrossRef] [PubMed] [Google Scholar]
- Segmental identity and vulnerability in cerebral arteries. Interv Neuroradiol. 2000;6:113-24.
- [CrossRef] [PubMed] [Google Scholar]
- Arterial vascular abnormality accompanying cerebral cortical dysplasia. AJNR Am J Neuroradiol. 1997;18:144-6.
- [Google Scholar]
- Notch3 mutations in CADASIL, a hereditary adult-onset condition causing stroke and dementia. Nature. 1996;383:707-10.
- [CrossRef] [PubMed] [Google Scholar]
- An essential role for Notch in neural crest during cardiovascular development and smooth muscle differentiation. J Clin Invest. 2007;117:353-63.
- [CrossRef] [PubMed] [Google Scholar]
- Wyburn-Mason or Bonnet-dechaume-blanc as cerebrofacial arteriovenous metameric syndromes (cams). A new concept and a new classification. Interv Neuroradiol. 2001;7:5-17.
- [CrossRef] [PubMed] [Google Scholar]
- Expression patterns of homeobox and other putative regulatory genes in the embryonic mouse forebrain suggest a neuromeric organization. Trends Neurosci. 1993;16:472-9.
- [CrossRef] [PubMed] [Google Scholar]
- Management of melanotic neuroectodermal tumor of infancy. Ann Diagn Pathol. 2004;8:207-12.
- [CrossRef] [PubMed] [Google Scholar]
- The expression of the mouse Zic1, Zic2, and Zic3 gene suggests an essential role for Zic genes in body pattern formation. Dev Biol. 1997;182:299-313.
- [CrossRef] [PubMed] [Google Scholar]
- Malformations of the craniofacial region: Evolutionary, embryonic, genetic, and clinical perspectives. Am J Med Genet. 2002;115:245-68.
- [CrossRef] [PubMed] [Google Scholar]
- Craniopharyngeal canal, morning glory disc anomaly and hypopituitarism: What do they have in common? Oxf Med Case Reports. 2018;2018:omy018.
- [CrossRef] [PubMed] [Google Scholar]
- Embryology of the neural crest: Its inductive role in the neurocutaneous syndromes. J Child Neurol. 2005;20:637-43.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and mortality of neurofibromatosis: A total population study in Finland. J Invest Dermatol. 2015;135:904-6.
- [CrossRef] [PubMed] [Google Scholar]
- Developmental basis of vascular smooth muscle diversity. Arterioscler Thromb Vasc Biol. 2007;27:1248-58.
- [CrossRef] [PubMed] [Google Scholar]
- The NF1 gene revisited-from bench to bedside. Oncotarget. 2014;5:5873-92.
- [CrossRef] [PubMed] [Google Scholar]
- Hypomelanosis of ito with multiple congenital anomalies. Ann Dermatol. 2019;31:576-80.
- [CrossRef] [PubMed] [Google Scholar]
- Hypomelanosis of ito (incontinentia pigmenti achromians)--a clinicopathologic study: Macrocephaly and gray matter heterotopias. Neurology. 1982;32:1013-6.
- [CrossRef] [PubMed] [Google Scholar]






