Translate this page into:
Does Contrast-Enhanced Cervical Ultrasonography Improve Preoperative Localization Results in Patients With Sporadic Primary Hyperparathyroidism?
Address for correspondence: Dr. Elias Karakas, Department of Visceral, Thoracic and Vascular Surgery, University Hospital Marburg, Baldinger Street, 35043 Marburg, Germany. E-mail: karakas@med.uni-marburg.de
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
Pre-operative localization studies are inevitable in patients with primary hyperparathyroidism (pHPT), who are eligible for focused or minimally invasive parathyroidectomy (MIP). High-resolution ultrasonography (US) in combination with planar 99mTc-Sestamibi-scintigraphy (MIBI) and additional single-photon emission computed tomography (SPECT) are the standard procedures to localize enlarged parathyroid glands. Our aim was to evaluate the practicability and significance of contrast-enhanced ultrasonography (CEUS) in patients with pHPT.
Materials and Methods:
All investigations were performed at the University Hospital Marburg. Totally, 25 patients with biochemical proven pHPT underwent preoperative US, MIBI/SPECT, and CEUS. For CEUS, a suspension of phospholipid-stabilized sulfur-hexafluoride (SF6) microbubbles in combination with a special 12 MHz linear US probe was used. All patients were investigated by two sonographers, who did not get to view the findings noted by the other. Finally, surgery was performed and histopathological results were obtained from 24 patients.
Results:
In 17 (68%) patients, US and MIBI/SPECT already raised suspicion of parathyroid lesions and all suspected lesions were reassessed by CEUS. However, no additional information was obtained using CEUS. Especially in eight patients with negative or inconsistent US and MIBI/SPECT results, CEUS did not provide additional information regarding the site of the suspected parathyroid adenoma. Overall, no side effects were observed using CEUS. Surgical cure was achieved in all patients.
Conclusion:
In this limited cohort of patients, no additional information could be obtained using the costly CEUS compared to results of US and MIBI/SPECT.
Keywords
Contrast-enhanced ultrasonography
primary hyperparathyroidism
99mTc-Sestamibi/single-photon emission computed tomography
ultrasonography
INTRODUCTION

Approximately, 85% of patients with primary hyperparathyroidism (pHPT) suffer from a single parathyroid adenoma. The success rate of the initial surgery is above 95%, in experienced hands.[1] Development and improvement of pre-operative noninvasive imaging techniques, particularly the planar 99m Tc-Sestamibi-scintigraphy (MIBI) and additional single-photon emission computed tomography (SPECT), and improvements in high-resolution ultrasonography (US) led to the implementation and further development of focused and minimally invasive surgical techniques.[2–4] In addition, intra-operative rapid parathyroid hormone monitoring (iOPTH) allows for assessing the completeness of parathyroid resection without visualizing all parathyroid glands.[5–7]
Cure rates of the minimally invasive parathyroidectomy (MIP) are equal compared to the conventional bilateral cervical exploration (BCE), which was considered for many decades as the standard approach in patients with pHPT.[5] MIP is also associated with decrease in complication rates.[8]
Recent literature underlines the importance of preoperative US in patients undergoing surgery for pHPT as a highly specific tool to identify parathyroid tumors and potential concomitant thyroid pathologies.[910] It may also provide detailed information regarding the exact site of the suspected parathyroid gland related to adjacent anatomic structures.[10]
Contrast-enhanced ultrasonography (CEUS) is a well-established diagnostic tool regarding parenchymatous organs such as liver, kidney, or spleen.[11–13] However, the significance of CEUS in patients with pHPT prior to the initial surgery has been hardly investigated. The aim of this study was to determine the applicability and significance of CEUS in patients with pHPT.
MATERIALS AND METHODS
25 patients with proven pHPT, preoperative US as well as MIBI/SPECT scans were selected for further evaluation using CEUS at the University Hospital Marburg, Germany.
Once informed consent was obtained and exclusion criteria were ruled out [Table 1], CEUS was performed according to the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) guidelines.[14] US and CEUS were performed by two different sonographers with expertise in head and neck US and both were blind to results obtained by the other.

US was performed using a high-resolution scanner with a high frequency (7-13 MHz) linear-array transducer with conventional color and power Doppler capability (Digital Gaia SA-8800, Kretztechnik AG, Zipf, Austria), including adjustable pulse repetition frequency (scale), focus, and color gain.
All findings suspicious of a parathyroid adenoma, such as, size, echogenicity, and site in relation to adjacent structures were defined.
Subsequently, CEUS was performed using a suspension of phospholipid-stabilized sulfur-hexafluoride (SF6) microbubbles (SonoVue™, Bracco SpA, Milan, Italy) in combination with a special 12 MHz linear US probe (Acuson Sequonia, Siemens medical solution, Erlangen, Germany).
Before intravenous application of the contrast agent, a conventional B-mode and color Doppler US of the thyroid region were done. The contrast agent was administered intravenously via a 20-gauge cannula at a concentration of 45 μg/ml, containing 8 μl/ml SF6 microbubbles. According to the manufacturer's instructions, a maximum of 112- 115 μg contrast agent was applied. A total volume of 2.4 ml was administered followed by a 5 ml saline flush. The agent was administered within 2-3 s, while the US probe focused on the suspected area in the neck. However, intermittent instead of continuous US scanning was performed to avoid US wave triggered damage to the microbubbles, which might influence the significance of the investigation.
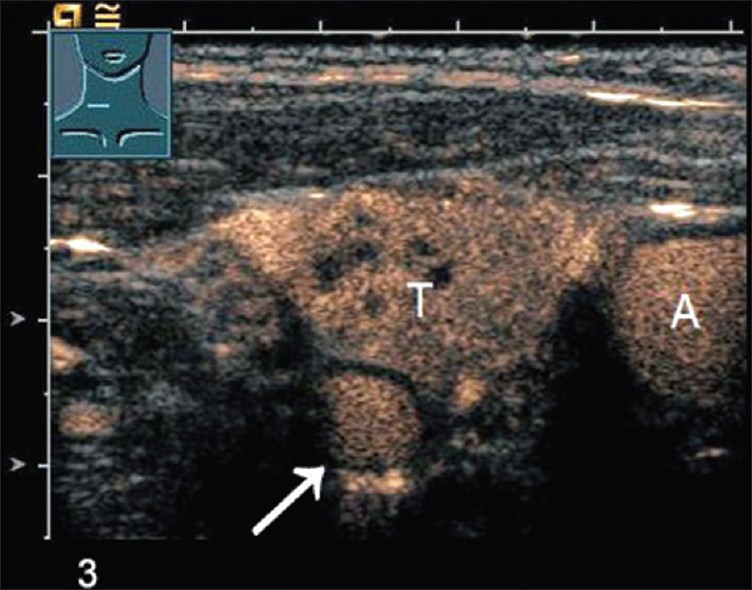
The CEUS investigation was divided into the wash-in and wash-out periods. The wash-in or arterial phase ranges from 0 to 30 s after application of the contrast agent. The wash-out or parenchymatous phase ranges from 30 to 120 s. Echogenicity, vascularization, and wash-in and wash-out characteristics of the suspected formation were defined and compared to the adjacent thyroid tissue within both phases. Results of US and CEUS were evaluated by well-experienced sonographers, who were blind to the other's findings [Table 2].
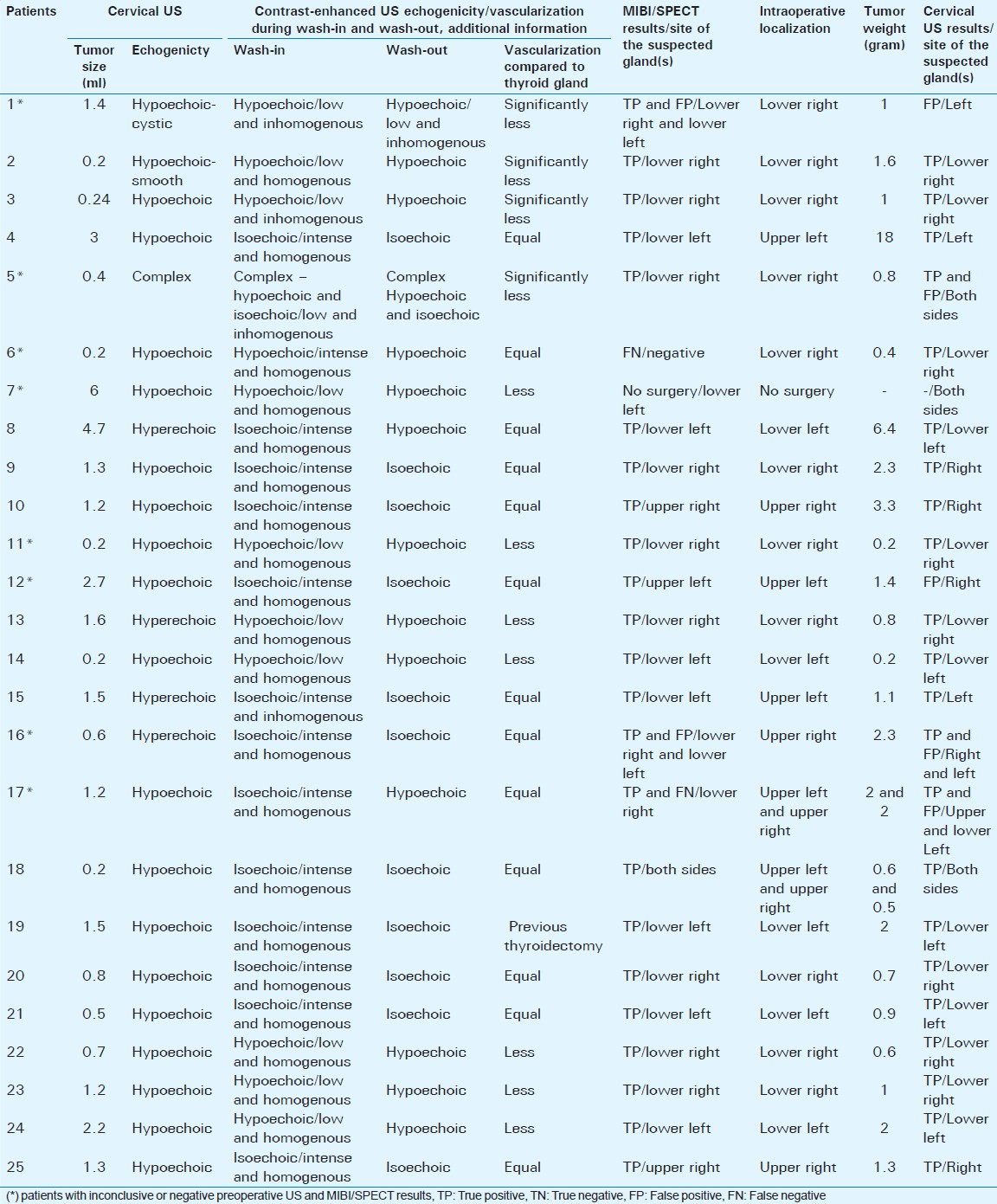
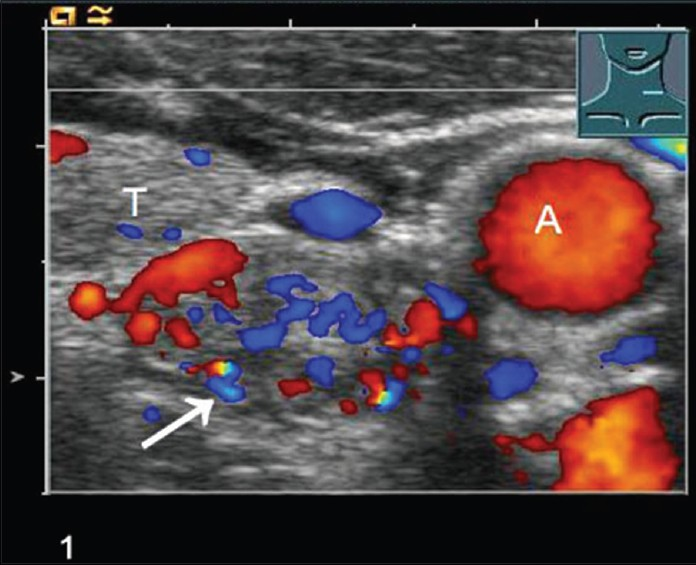
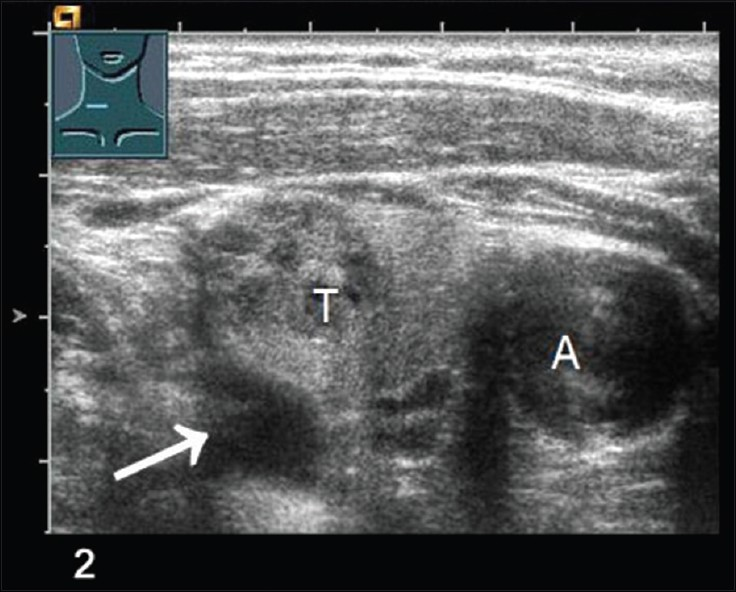
Figures 1–4 clearly show color-coded Doppler US (1), conventional B-mode US (2), the wash-in phase (3), and wash-out phase (4) of a suspected parathyroid adenoma (arrow) next to the thyroid (T) and carotid artery (A).
- Color-coded Doppler ultrasonography shows a parathyroid adenoma (arrow), Thyroid lobe (T), Carotid artery (A).
- Conventional B-mode US scan shows a parathyroid adenoma (arrow), Thyroid lobe (T), Carotid artery (A).
- Contrast-enhanced ultrasonography CEUS in wash-in phase shows a parathyroid adenoma (arrow), Thyroid lobe (T), Carotid artery (A).

- Contrast-enhanced ultrasonography CEUS in wash-out phase shows a parathyroid adenoma (arrow), Thyroid lobe (T), Carotid artery (A).
In addition, results of US and CEUS were compared to results of MIBI/SPECT investigations.
Planar scintigraphy was performed 5, 15, and 120 min after intravenous injection of 740 MBq of 99mTc-MIBI. Static images in anterior view with a 128 × 128 matrix were acquired of the cervical and thoracic area using a dual head gamma camera equipped with a low-energy high-resolution (LEHR) collimator (Symbia, Siemens, Erlangen, Germany). SPECT acquisition was performed at the “late” phase (90 min after intravenous injection) and all 128 views were acquired with an acquisition time of 30 s per view using the same system.
Positive preoperative localization was followed by an open minimally invasive parathyroidectomy (OMIP) or focused unilateral parathyroidectomy. In patients with inconclusive or negative results, no further imaging, but a BCE of the neck was performed. Rapid iOPTH was used to confirm complete removal of all hyper-functioning parathyroid tissue in patients who underwent OMIP or focused parathyroid surgery. Frozen sections were prepared and definite histopathological investigation done on all specimens that were removed during surgery.
In addition, all preoperative localization results were compared to intra-operative findings.
RESULTS
Preoperative localization studies were performed in 17 female and eight male patients suffering from pHPT. Clinical and laboratory data are summarized in Table 3.

In 17 patients (68%), preoperative MIBI/SPECT, US, and CEUS showed consistent results. Fifteen of these patients underwent a focused unilateral or MIP. In two patients, a BCE was done because preoperative localization results suggested a double adenoma with one enlarged parathyroid gland on each side in one patient, and BCE was necessary because US provided evidence of concomitant thyroid pathology in the other patient. In all 17 patients, frozen section confirmed the diagnosis of a parathyroid adenoma and in all patients, an adequate PTH drop was documented using iOPTH.
In eight patients (32%), results of US and MIBI/SEPCT were inconsistent. One of these patients suffered from mild pHPT with only slightly elevated calcium and PTH values (Ca, 2.7 mmol/l; PTH, 78 ng/l). In this 81-year-old asymptomatic female patient, SPECT was positive, whereas the planar MIBI-scan was negative. US suggested an enlarged bilateral multinodular goiter without evidence of a suspected parathyroid gland. In this patient, a close follow-up was recommended instead of surgery.
Results of preoperative localization procedures, including characteristics of the suspected parathyroid glands during US and CEUS and intra-operative findings are summarized in Table 3.
CEUS was done in all 25 patients but did not reveal additional information regarding suspected or discordant findings of conventional cervical sonography or MIBI/SPECT. In summary, echogenicity of the suspected parathyroid adenomas was inconsistent as 11 out of 25 glands were hypoechoic and 13 out of 25 patients were isoechoic compared to the thyroid gland. In 11 patients, vascularization was described as less or significantly less, whereas it was equal in 13 patients compared to the thyroid. In one patient, we were not able to compare echogenicity and vascularization of the presumed parathyroid adenoma with the thyroid gland, due to previous thyroidectomy, since the presence of thyroid disease or the absence of thyroid gland might interfere with the diagnostic accuracy of CEUS.
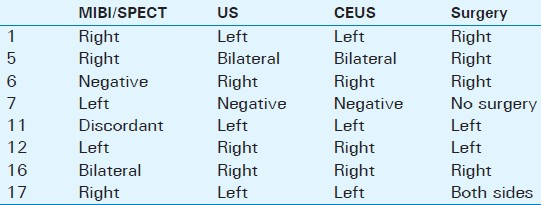
Results of the eight patients with inconsistent US and MIBI/SPECT results are shown in Table 4. In these patients, CEUS was at best able to confirm the US results.
DISCUSSION
In the era of focused and minimally invasive parathyroid surgery, pre-operative localization procedures are of utmost importance and the success of a focused approach is dependent on accurate preoperative imaging.[2581516] During the past decade, preoperative localization procedures, especially planar MIBI and additional SPECT and high-resolution US, have significantly improved.[16–18] Thus, MIP became the treatment of choice in patients with preoperatively localized sporadic pHPT. Several prospective trials showed success rates of focused parathyroid operations that were similar to success rates of the BCE.[3815] US and MIBI/SPECT show sensitivity rates of up to 90%.[1719–22] Taking these facts into account, the question arises, whether additional complex and cost expensive preoperative localization tools are needed.
CEUS is an important addition in the diagnostic workup routine of parenchmatous organs, such as, liver, spleen, and kidney.[23–25] Despite the use of considerably improved contrast agents, we were not able to provide evidence for a significant gain of information using CEUS in patients suffering from pHPT. Moreover, we were not able to prove the promising results of Mazzeo and colleagues.[26] In their study, CEUS was performed using a galactose-based microbubble contrast agent, which requires a high mechanical index (MI>0.7) that leads to a rapid destruction of the microbubbles, and therefore prevents real-time investigation of the suspected structures. Furthermore, the authors were able to compare preoperative localization results with intra-operative findings in a rather small group of patients: Only 10 out of 13 patients underwent surgery for pHPT and in only nine patients a parathyroid adenoma was detected intra-operatively. The rather heterogeneous results of color Doppler US and CEUS investigations, the use of an inappropriate, water-soluble contrast agent with a less intense signal enhancement with the less valuable characteristic of diffusing into the extracellular matrix, and the small number of patients included do not allow for definite conclusions from this pilot study.[26]
Despite a comparable cohort of patients, almost equal technical requirements (e.g. US probe, MI<0.17), and the use of the same, considerably improved, non-water-soluble contrast agent, our results are contradictory to the promising results reported by Agha et al., who were able to localize all suspected parathyroid glands in 30 patients suffering from pHPT. In this study, all patients underwent conventional US, color Doppler US, scintigraphy, and magnetic resonance imaging (MRI) together with CEUS. However, it remains unclear whether the CEUS performing ultrasonographer was blind to the accompanying localization results. Moreover, the authors do not provide information regarding the time schedule of the localization procedures performed and the number of patients with completely negative US, MIBI, and MRI results.[27]
CEUS has all the disadvantages of conventional US, including the high dependency on the individual skill of the investigator. It is implicitly necessary to identify a suspected lesion before CEUS can be applied because there is a given time frame of the wash-in and wash-out phases that does not allow for an extensive scanning of the thyroid region.
In addition, intermittent instead of permanent US scanning after application of the contrast agent is recommended due to US wave triggered burst of the microbubbles. CEUS is therefore not suitable to primarily localize an undetected parathyroid adenoma. Our results show that CEUS does not give helpful additional information in cases when US and MIBI/SPECT results are inconsistent or negative.
Knowledge of a retrosternal, intra-thoracic, or deep mediastinal position of the suspected gland is of utmost importance for planning the surgery, but neither US nor CEUS are able to detect these glands. However, MIBI/SPECT is able to reliably visualize parathyroid tumors in extra-cervical positions.
CEUS seems to be easy to apply and might be less expensive compared to scintigraphy or MRI investigations.[27] However, to perform CEUS, ultrasonic devices have to be equipped with specific US probes and software and investigators have to undertake a special training.[14]
Therefore, US and MIBI/SPECT are still the standard preoperative localization procedures in our institution, complying with requirements to definitely localize a suspected solitary parathyroid gland in patients suffering from pHPT. In patients with inconclusive or negative MIBI/SPECT and US results, a BCE of the neck should be performed by an experienced endocrine surgeon, whereas additional noninvasive and invasive localization procedures, such as, MRI, CT, Methionine-PET, or preoperative selective venous sampling, are only recommended before re-operation in the neck due to recurrent pHPT or following thyroid surgery.[2829]
A potentially promising application of CEUS in patients with preoperatively localized pHPT might be a specific application of antibodies on microbubbles (microbubble coating), that target parenchymatous organs or endocrine tissue. This might lead to a highly selective accumulation in a particular tissue and in case of preoperative parathyroid localization may help to definitely differentiate between parathyroid glands and surrounding tissue.
CONCLUSION
CEUS is a well-established diagnostic tool for investigating parenchymatous organs such as, liver, kidney, or spleen. In this limited cohort of patients, no additional information could be obtained using the costly CEUS compared to results of US and MIBI/SPECT. However, additional investigations are necessary to finally estimate potential advantages of an additional use of CEUS in parathyroid or thyroid surgery.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/64/103054
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Results of video-assisted parathyroidectomy: Single institution's six-year experience. World J Surg. 2004;28:1216-8.
- [Google Scholar]
- Minimally invasive thyroid and parathyroid surgery is not a question of length of incision. Langen becks Arch Surg. 2008;393:621-6.
- [Google Scholar]
- Does intraoperative quick parathyroid hormone assay improve the results of parathyroidectomy? World J Surg. 2002;26:926-30.
- [Google Scholar]
- Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg. 2002;235:665-70.
- [Google Scholar]
- The superiority of minimally invasive parathyroidectomy based on 1650 consecutive patients with primary hyperparathyroidism. Ann Surg. 2011;253:585-91.
- [Google Scholar]
- The impact of office neck ultrasonography on reducing unnecessary thyroid surgery in patients undergoing parathyroidectomy. Thyroid. 2005;15:1055-9.
- [Google Scholar]
- Ultrasonography for the endocrine surgeon: A valuable clinical tool that enhances diagnostic and therapeutic outcomes. Surgery. 2005;138:1193-200.
- [Google Scholar]
- Members of Contrast Media Safety Committee of European Society of Urogenital Radiology (ESUR).Safety of ultrasound contrast agents. EurRadiol. 2005;15:941-5.
- [Google Scholar]
- Etiology of cecal and hepatic lesions in mice after administration of gas-carrier contrast agents used in ultrasound imaging. Toxicol Appl Pharmacol. 2003;188:176-84.
- [Google Scholar]
- Ultrasound contrast agents: Properties, principles of action, tolerance, and artifacts. Eur Radiol. 2001;11:1316-28.
- [Google Scholar]
- Guidelines for the use of contrast agents in ultrasound. January 2004. Ultraschall Med. 2004;25:249-56.
- [Google Scholar]
- Conventional bilateral cervical exploration versus open minimally invasive parathyroidectomy under local anaesthesia for primary hyperparathyroidism. Br J Surg. 2005;92:190-7.
- [Google Scholar]
- Prospective evaluation of sestamibi scan, ultrasonography, and rapid PTH to predict the success of limited exploration for sporadic primary hyperparathyroidism. Surgery. 2004;136:872-80.
- [Google Scholar]
- Can localization studies be used to direct focused parathyroid operations? Surgery. 2001;129:720-9.
- [Google Scholar]
- Factors contributing to negative parathyroid localization: An analysis of 1000 patients. Surgery. 2008;144:74-9.
- [Google Scholar]
- Prospective evaluation of delayed technetium-99m sestamibi SPECT scintigraphy for preoperative localization of primary hyperparathyroidism. Surgery. 2002;131:149-57.
- [Google Scholar]
- Impact of gland morphology and concomitant thyroid nodules on preoperative localization of parathyroid adenomas. Laryngoscope. 2006;116:580-5.
- [Google Scholar]
- Preoperative evaluation of hyperparathyroidism: The role of dual-phase parathyroid scintigraphy and ultrasound imaging. Ann Nucl Med. 2008;22:123-31.
- [Google Scholar]
- Clinical value of parathyroid scintigraphy with technetium-99m methoxyisobutylisonitrile: Discrepancies in clinical data and a systematic metaanalysis of the literature. World J Surg. 2004;28:100-7.
- [Google Scholar]
- Current and potential renal applications of contrast-enhanced ultrasound. ClinRadiol. 2012;67:909-22.
- [Google Scholar]
- Contrast-enhanced color Doppler ultrasonography in suspected parathyroid lesions. Acta Radiol. 2000;41:412-6.
- [Google Scholar]
- Contrast-enhanced ultrasonography for localization of pathologic glands in patients with primary hyperparathyroidism. Surgery. 2012;151:580-6.
- [Google Scholar]
- High success rate of parathyroid reoperation may be achieved with improved localization diagnosis. World J Surg. 2008;32:774-81.
- [Google Scholar]
- Reoperation for primary hyperparathyroidism: Tips and tricks. Langenbecks Arch Surg. 2010;395:103-9.
- [Google Scholar]






