Translate this page into:
Diagnostic Imaging for Dental Implant Therapy
Address for correspondence: Dr. Aishwarya Nagarajan, Department of Periodontology, Meenakshi Ammal Dental College, Alapakkam Main Road, Chennai - 600 095, Tamil Nadu, India. E-mail: aish.magic@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Dental implant is a device made of alloplastic (foreign) material implanted into the jaw bone beneath the mucosal layer to support a fixed or removable dental prosthesis. Dental implants are gaining immense popularity and wide acceptance because they not only replace lost teeth but also provide permanent restorations that do not interfere with oral function or speech or compromise the self-esteem of a patient. Appropriate treatment planning for replacement of lost teeth is required and imaging plays a pivotal role to ensure a satisfactory outcome. The development of pre-surgical imaging techniques and surgical templates helps the dentist place the implants with relative ease. This article focuses on various types of imaging modalities that have a pivotal role in implant therapy.
Keywords
Cone beam computed tomography
dental implants
dosimetry
implant imaging
magnetic resonance imaging
treatment planning
INTRODUCTION

Imaging plays an important part in dental implant procedures. The imaging modalities vary from standard projections routinely available in the dental office to more complex radiographic techniques typically available only in radiology centers. Implant imaging provides accurate and reliable diagnostic information of the patient's anatomy at the proposed implant site. Standard projections include intra-oral (periapical, occlusal) and extra-oral (panoramic, lateral cephalometric) radiographs. More complex imaging techniques include conventional X-rays, computed tomography (CT), and cone beam computed tomography (CBCT). Multiple factors influence the selection of radiographic techniques for a particular case including cost, availability, radiation exposure, and patient's anatomy. The dentist aspires to find a balance between these factors with an aim to minimize risk of any complications to the patient.[1]
The objectives of imaging are to decide if implant treatment is appropriate for the patient, to identify the location of vital anatomical structures such as the inferior alveolar nerve and maxillary sinus, to ascertain bone quantity, height, buccolingual width, and angulation of alveolar process, to detect any possible pathological conditions, and also to decide the length and width of the implant to be placed.
Imaging modality is useful in three phases of treatment.[1]
Phase 1: Pre-prosthetic implant imaging
Imaging in this phase determines the quantity, quality, and angulation of bone; relationship of critical structures to prospective implant sites; and the presence or absence of disease at the proposed surgical sites.
Phase 2: Surgical and interventional implant imaging
Imaging in this phase evaluates the surgical sites during and immediately after surgery, assists in the optimal positioning and orientation of dental implants, and ascertains the healing and integration phase of implant surgery. It also ensures appropriate abutment positioning and prosthesis fabrication.
Phase 3: Post-prosthetic implant imaging
This phase commences just after placement of the prosthesis and continues as long as the implant remains in the jaw. Imaging in this phase evaluates the long-term change, if any, in the implant's fixed position and function, including the crestal bone levels around each implant, and evaluates the status and prognosis of the dental implant. It also helps to routinely assess the bone adjacent to the dental implant to note any changes in mineralization or bone volume.
The goals of imaging are:
-
To measure bone height and width (bone dimensions)
-
To assess bone quality
-
To determine the long axis of alveolar bone
-
To identify and localize internal anatomy
-
To establish jaw boundaries
-
To detect any underlying pathology.
PLANAR IMAGING MODALITIES
Periapical radiography
Periapical radiography is used to find the presence of pathosis and location of anatomic structures around the implant site, and evaluate implants postoperatively. It is used to determine vertical height of the edentulous region, architecture, and bone quality. For the edentulous and resorbed jawbone, however, this technique can be difficult as adequate support for positioning the instrument is not available. Attaching a film holder to the tube, while carefully positioning the jaw bone under investigation parallel to the film, may offer a solution. Figure 1 shows the postoperative periapical radiograph of an osseointegrated implant.
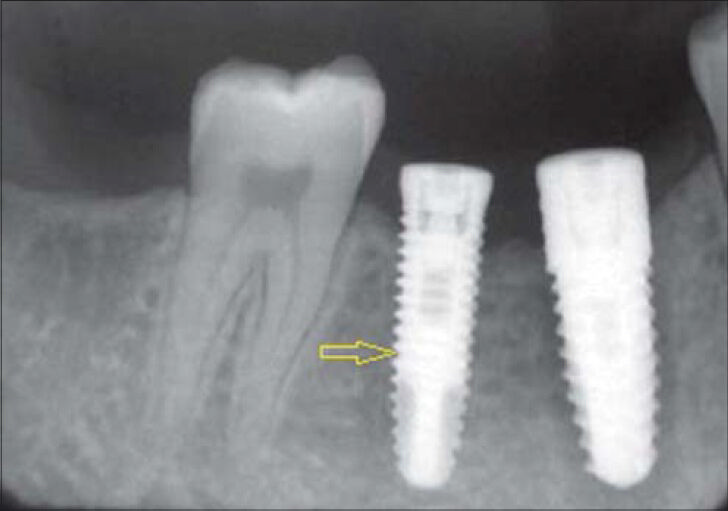
- 45-year-old male patient imaged for the evaluation of the implant. Periapical radiograph of the left mandibular posterior region shows the osseointegrated implant (arrows).
Intra-oral imaging using electronic or charge-coupled device imaging techniques
Charge-coupled device (CCD) detectors consist of a serial chain of signal components, such as phosphors, fiber optics or lenses, image intensifiers, and the CCD, which serve to convert the X-ray energy to light or electron-hole pairs and to record the spatially resolved image. With CCDs, pre-surgical implant assessment of a single site becomes precise. CCD provides accurate measurement of implant sites preoperatively and gives information about osseo-integration postoperatively.
CCD detectors are readily available and offer high-resolution images with minimal distortion.
However, CCDs have some disadvantages. Only a small area can be imaged and CCDs produce 2D images that are difficult to reproduce (due to non-uniformities in the phosphor, the optical couplings, the transmission of the fiber optics, and the response of the CCD pixels). Image elongation or foreshortening is also common (due to image intensifiers and optical coupling in the system).
Occlusal radiography
High-resolution planar images of the mandible or the maxilla are produced by occlusal radiography. Structures like maxillary sinus, nasal cavity, and nasopalatine canal can be assessed through occlusal radiography. Mandibular occlusal radiograph projection is less distorted than the maxillary occlusal radiograph.[1]
As periapical radiographs are unable to produce any cross-sectional information, occlusal radiographs are sometimes used to determine the facio-lingual dimensions of the mandibular alveolar ridge.
Occlusal imaging does not provide detailed information of the facial–lingual dimension of the alveolar ridge. It has limited reproducibility (replication of the imaging region), and superimposition of images (lack of distinctiveness of the image due to overlapping of the structures) is common.
Cephalometric radiography
Lateral cephalometric radiography helps in the analysis of the quality of the bony site (ratio of compact to cancellous bone), especially in the anterior region of the mandible. Though it gives limited information about the symphyseal area, the inclination and buccolingual dimensions of the anterior jawbone region can be obtained. These images do not provide useful information when planning placement of implants lateral to the mid-sagittal plane. Overly optimistic bone volume assessments are created due to the presence of genial tubercles.
The advantage of lateral cephalometric radiographs is that they outline the geometry of the alveolus in the anterior region and the relationship of the lingual plate to the patient's skeletal anatomy.
The disadvantages of this technique are that it is not useful for demonstrating the bone quality and only demonstrates a cross-sectional image of the alveolus where the central rays of the X-ray device are tangent to the alveolus. Other disadvantages include low power magnification and superimposition of images (lack of distinctiveness of the image due to overlapping of the structures).
Panoramic radiography
These are narrow beam rotational tomographs, which use two or more centers of rotation with a predefined focal trough, to produce an image of both the upper and lower jaws. Optimal patient positioning is crucial in this procedure because jaw positioning errors in the sagittal plane can occur easily, especially in the edentulous patient. It provides an approximation of bone height, vital structures, and any pathological conditions that may be present.[2]
Figure 2 shows the evaluation of sub-periosteal implant using panoramic radiograph.
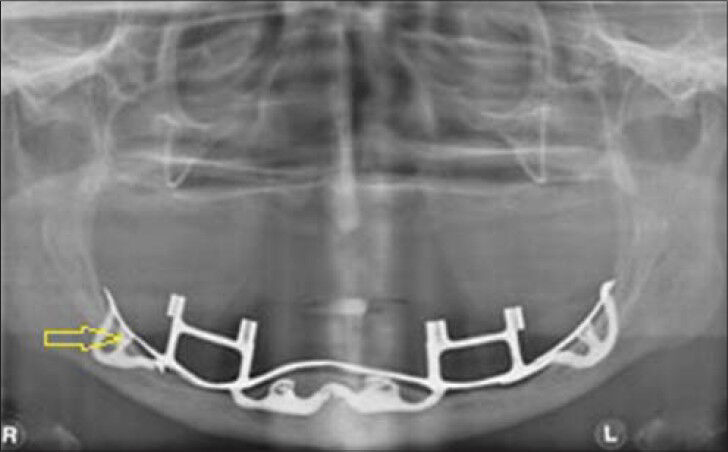
- 65-year-old female with completely edentulous maxillary and mandibular arches. Panoramic radiograph demonstrates a mandibular subperiosteal implant (arrows).
Advantages of panoramic radiography are that they provide information on opposing landmarks, vertical height of the bone, assess crestal alveolar bone and cortical boundaries, and evaluate gross anatomy of the jaws and related pathologic conditions.
Disadvantages of this modality are distortion of the visualized structures, low level of reproducibility, 1.1-1.7 times magnification of the structures, difficulty in assessing hard tissue morphology and density of the bone, little information about the buccolingual cross-sectional dimension, inadequate identification of critical structures, and no data of spatial relationships between the structures.
Zonography
Zonography is a modification of the panoramic X-ray machine and generates cross-sectional image of the jaws. The tomographic layer is around 5 mm. Zonography allows appreciation of spatial relationship between the critical structures and the implant site.
However, the disadvantages are presence of relatively thick tomographic layers, blurred adjacent structures superimposed on the image, and inability to identify the differences in bone densities or presence of disease pathology at the implant site.
QUASI 3D IMAGING MODALITIES
X-ray tomography
This is a special X-ray technique that enables visualization of a section of patient's anatomy above and below the section of interest. Tomography is derived from the Greek words “Tomo” (slice) and “Graph” (picture).
Conventional tomography
Conventional tomography differs from X-ray tomography in its ability to resolve details as small as a few microns in size, even when imaging objects is made of high-density materials. In the last two decades, conventional tomographic machines have been introduced in oral health care. Some extra-oral X-ray equipments may also offer possibilities for cross-sectional imaging. Sharp visualization of structures in the focal plane, while blurring all other structures is achieved by working with different tomographic movements in the linear, circular, spiral, elliptical, and hypocycloidal planes. Complex tomographic movements (e.g. spiral and hypocycloidal) are the most widely used.
Digital tomographic images offer increased image quality by contrast enhancement, reduction of blurring, and image manipulation. Further image processing may yield precise information on bone volume, (relative) bone density, and help to simulate implant surgery by visualizing the planned implant in relation to the anatomic structures.[3]
For radiographic visualization of the mandibular canal, cross-sectional imaging provides the best information. When comparing computed to conventional tomography (hypocycloidal and spiral) for measuring the distances to the mandibular canal CT does not seem to be more accurate. Spiral tomography performs better than hypocycloidal tomography as the borders of the canal are better identified with the former technique. The greatest inaccuracy is found when using panoramic images.[4]
Conventional tomography has the advantage in that it can determine the spatial relationship between the critical structures and the implant site and help in quantification of the geometry of the alveolus. The reformatted CT images provide axial, panoramic, and cross-sectional images that are all cross-referenced to one another allowing rapid correlation of different views.
Teeth, particularly those with metallic restorations adjacent to the area of interest, obscure the tomographic image. Limited resolution caused by use of an intensifying screen cassette makes the identification of anatomical structures and assessment of bone topography more difficult. Conventional tomography cannot assess the bone quality and does not identify bone and dental disease.
Computed tomography
CT was invented by Sir Godfrey Hounsfield and was introduced in 1972.[5] This modality gives rise to high-density resolution images, and allows soft tissues to be visualized. The reformatted CT image generates axial, panoramic, and cross-sectional images that allow rapid correlation of the different views.
CT scan provides tangential and cross-sectional tomographic images of the implant site. Figure 3 explains the various sections of a CT scan. Reformatted images are characterized by in-plane resolution of 1 pixel by scan spacing (0.5-1.5 mm) and a section thickness of 1 pixel (0.25 mm) resulting in a geometric resolution similar to that of planar imaging. The density of structures produced in the image is absolute and quantitative, and can be used to differentiate tissues in the region and characterize bone quality.
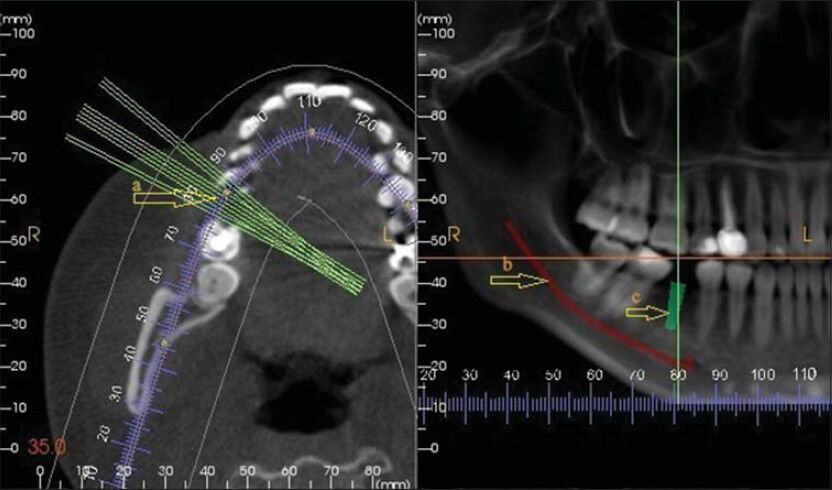
- 39-year-old male with mandibular edentulous posterior region. CT of the edentulous area of the mandibular posterior region for the evaluation of bone for implant placement. a) Various sections of CT (arrow); b) shows the inferior alveolar nerve (arrow); and c) shows the arbitrary implant placement (arrow).
Disadvantages include limited availability of CT scanners, high cost of machines, image artifacts caused by metal, technique errors, and the need for special training in image interpretation.
Interactive computed tomography
Interactive CT (ICT) allows the transfer of images to the clinician as a computer file. It helps the clinician measure the length and the width of the alveolus and also bone quality. An important aspect of ICT is that the clinician and radiologist can together perform “electronic surgery” (ES).
Cone-beam computerized tomography
CBCT scanners are designed specifically for diagnosis and treatment planning in implant therapy. Multiple pictures of the region of interest are generated in a single scan. This enables the dentist to perform minimally invasive surgery without raising a flap, thereby reducing surgery time, postoperative pain and swelling, and faster recovery time.[6] A master cast can be fabricated pre-surgically using the information that is stored in the surgical plate, and a provisional restoration can be placed immediately after surgery.
Radiographic markers can be inserted at the time of the scan and these identify the precise location of the proposed implants.[7] Stents provide radiographic landmarks that can be used to correlate proposed clinical location and angulation of implants with the available alveolar bone.
With the help of Digital Imaging and Communications in Medicine (DICOM) data, computer-generated surgical guides (stereolithographic models) can be fabricated from the CBCT data. The guide helps the surgeon place implants in their optimal and exact position. Figure 4 demonstrates the stereolithographic model that was fabricated using the data obtained from CBCT.

- 62-year-old female with completely edentulous maxillary arch. Image shows the stereolithographic model of the maxillary region.
A stereotactic surgical template is fabricated from a model that replicates the patient's alveolar structure. The template determines the position and orientation of the guide cylinders and this accurately identifies the position and orientation of the proposed implants. Figure 5 shows the implant site assessment that is carried out using CBCT.
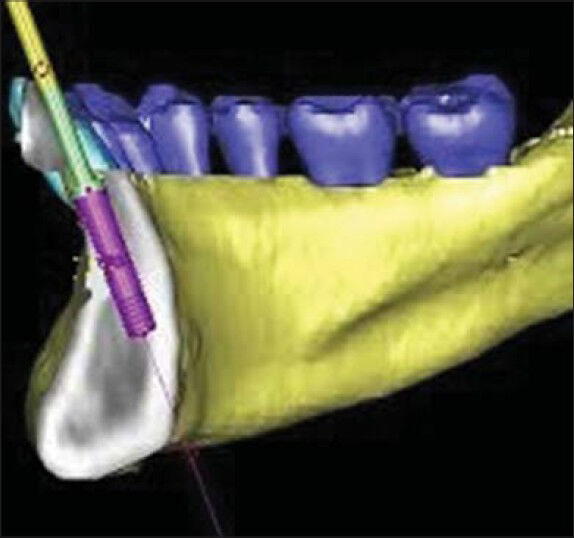
- 30-year-old female patient with edentulous mandibular anterior region. CBCT shows implant placement site in the mandibular anterior region.
Advantages of CBCT are that it generates a 3D dataset (digitally reconstructed image with 670 projections), has the potential for generating all 2D images (e.g. orthopantomogram, lateral cephalogram), and allows vertical scanning with the patient in a seated position. Figure 6 demonstrates the various sections of CBCT.
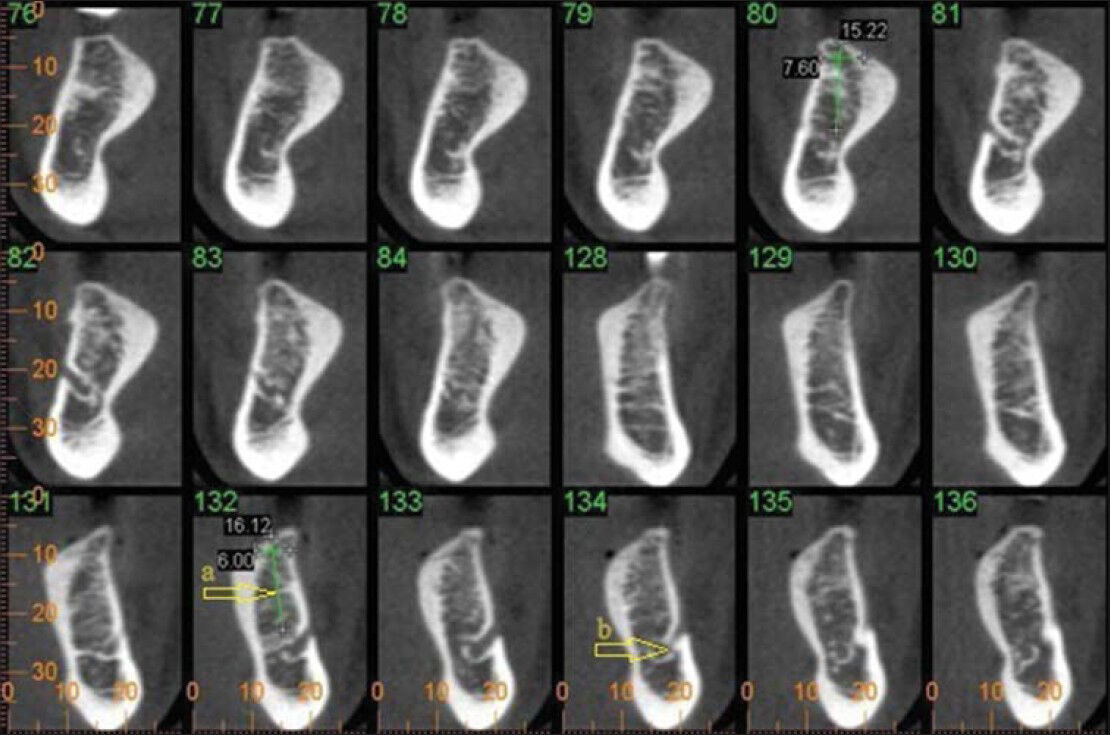
- 40-year-old male with mandibular posterior region. CBCT of mandibular posterior region for the evaluation of implant placement (a) shows the implant size (arrow) using the available bone and (b) points out the cross section of the inferior alveolar nerve (arrow).
CBCT generates high-resolution images of anatomical structures, bone trabeculae, periodontal ligament (PDL), and root formation. The other advantages include rapid scanning procedure, lower radiation dose, reduced disturbance from metal artifacts, lower cost, easy accessibility, easy handling, and DICOM compatibility.
CBCT has some disadvantages. It has a low contrast range, restricted field of view (FOV), reduced scanned volume caused by limited detector size, gives little information about the inner soft tissue, and increased noise from scatter radiation and artifacts.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) was first discovered by Lauterbur. The presence of ferromagnetic (high magnetic susceptibility) metals can distort the magnetic field and compromise the images. Non-ferromagnetic alloys do not produce image deformities, whereas non-precious ferromagnetic alloys (cobalt–chromium) produce large image deformations. Devge et al., found that MRI images are not affected by implants of the Branemark system.[8]
MRI differentiates the inferior alveolar canal and neurovascular bundle from adjacent trabecular bone, and visualizes the fat in the trabecular bone.[9] MRI avoids radiation hazards associated with CT.
MRI is contraindicated for patients with ferromagnetic metallic implants in their bodies. Unlike multi-plane reformatted CT images, cross-sectional MRI images are obtained using conventional reformatting due to the lack of software support for MRI data. Thus, MRI is not useful in characterizing bone mineralization.
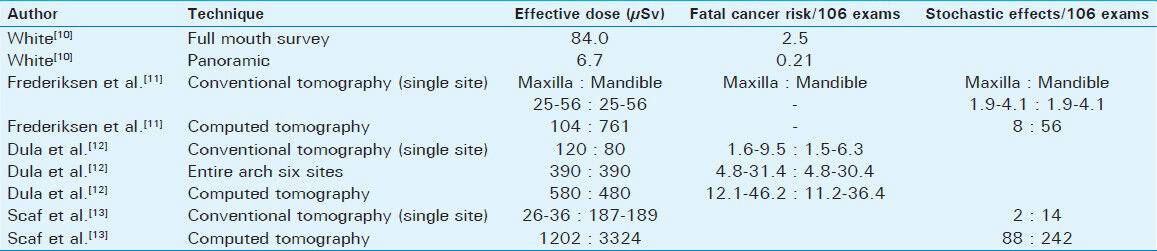
DOSIMETRY
Appropriate selection criteria must be applied to choose the correct imaging modality.[10] Dentist must consider potential risks versus perceived benefits of each imaging procedure [Table 1].[1] When the dentist prescribes a radiographic examination, the ALARA principle (as low as reasonably achievable) of radioactive materials or radiation-producing devices should be kept in mind. Radiographs should only be prescribed when the information required cannot be obtained by any lesser invasive modalities.
RECENT ADVANCES IN IMAGING
Using the platform of the SCANORA (Sordex Orion Corporation, Helsinki, Finland), a limited-volume CBCT system 3DX Accuitomo was developed. PSR9000N [Figure 7] is also a limited-volume CBCT system, which is an inherited technology from another dento-maxillary multimodal tomographic system, the AZ3000 (Asahi Roentgen, Japan).[14]

- New Tom CBCT system.
Cross-sectional images of a small, defined area in the jaws and dental arches are produced by these dental tomographic platforms. Minimization of the radiation dose is a remarkable advantage of limited-volume CBCT.
The main disadvantage of low-dose CBCT is the difficulty in the acquisition of reliable CT values, which leads to poor soft tissue resolution. But this helps to reduce metal and beam hardening artifacts, which are inherent in CT imaging. In limited-volume CBCT imaging, the size of FOV is small compared to the head and the intensity of transparent X-radiation fluctuates during the 360° scan. Metal artifacts in conventional fan-beam CT images are common. Metals producing artifacts are usually detectable. It is difficult to detect the appearance of halation artifacts in CBCT because their cause is outside the imaged area. Further studies are necessary to identify the characteristics of these presumed halation artifacts.
DISCUSSION
Medical images can be assessed for their technical quality and diagnostic value. The clinician has to carefully weigh the pros and cons of each modality and choose a particular technique accordingly.
Literature suggests that when evaluating the alveolar ridge, the radiologist should also determine the angle that the ridge makes with the vertical axis. This is important because the occlusal force vector that acts upon the fixture should be parallel to the vertical axis through the alveolar ridge. If excess angulation exists between the vertical axis through the fixture than that through the alveolar ridge, the resultant force vector may fall in an area which is unable to withstand the occlusal forces and breakdown of the surrounding bone may occur.
The various radiographic methods detailed here have their unique characteristics and each of these applied judiciously, where required, will help the diagnostician as well as the clinician to accurately plan, execute, and evaluate implant treatment.
Periapical radiographs produce a high-resolution planar image of a limited region of the jaws and do not provide any cross-sectional information of the jaws. Occlusal radiography produces high-resolution planar images of the body of the mandible or the maxilla. Cephalometric radiographs are a useful tool for the development of an implant treatment plan, especially for the completely edentulous patient, or for placement of implants near the midline for overdentures.
MRI is used in implant imaging as a secondary imaging technique where primary imaging techniques such as CT or ICT have failed. MRI visualizes the fat in the trabecular bone and differentiates the inferior alveolar canal and neurovascular bundle from the adjacent trabecular bone.
Since the introduction of CBCT scanners in the late 1990s, there has been great interest in these devices in the field of oral and maxillofacial surgery, orthodontics, and dentistry. Swennen and Schutyser stated that with CBCT, the image value of a voxel of an organ depends on the position in the image volume.[15] Several studies have described the value of computer-guided implant bed preparation for dental implantology. Gert Wittwer et al., evaluated a novel approach in the placement of interforaminal mandibular dental implants with computer-assisted navigation and without conventional elevation and reflection of mucoperiosteal flaps or mucosal punching at the surgical site.[16] Patel et al., stated that perhaps the most clinically useful aspect of CBCT imaging is the highly sophisticated software that allows the huge volume of data collected to be broken down and processed or reconstructed into a format that closely resembles that produced by other imaging modalities.[17] Vannier stated that when new developments in the synthesis and optimization of CBCT reconstruction algorithms allow the full exploitation of the potential of area detectors in CBCT, it will provide important benefits for craniofacial imaging.[18] It is expected that improvements in cone-beam reconstruction algorithms and post processing will solve or reduce this problem.
Flapless transmucosal implant placement is also an ideal method to treat cases of medically compromised patients. One major limitation of this new technique is the cost of CT images and the navigation technology. However, the benefits outweigh its cost.
CONCLUSION
With the excellent imaging modalities that exist today, one can enhance the success of implant placement. Selection of an appropriate imaging modality should be made based on the type and number of implants, location of the implant, and surrounding anatomy. As in the case of all imaging techniques, appropriate selection criteria must be applied before selecting one which is most suitable for each patient.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/2/4/143440
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Radiographic results. In: Branemark PI, Zarb GA, Albrektsson T, eds. Tissue-Integrated Prostheses: Osseointegration in Clinical Dentistry. Vol 3. Chicago: Quintessence; 1985. p. :187-98.
- [Google Scholar]
- Density of bone: Effect on treatment plans, surgical approach, healing, and progressive bone loading. Int J Oral Implant. 1990;6:23-31.
- [Google Scholar]
- Reliability of hypocycloidal tomography for the evaluation of the distance from the alveolar crest to the mandibular canal. Dentomaxillofac Radiol. 1991;20:200-4.
- [Google Scholar]
- Imaging modalities for preoperative assessment in dental implant therapy: An overview. Hong Kong Dent J. 2010;7:23-30.
- [Google Scholar]
- A comparative evaluation of cone beam computed tomography (CBCT) and multi-slice ct (MSCT). Part II: On 3D model accuracy. Eur J Radiol. 2010;75:270-4.
- [Google Scholar]
- A new volumetric CT machine for dental imaging based on the cone-beam technique: Preliminary results. Eur Radiol. 1998;8:1558-64.
- [Google Scholar]
- Magnetic resonance imaging in patients with dental implants: A clinical report. Int J Oral Maxillofac Implants. 1997;12:354-9.
- [Google Scholar]
- Pre-surgical dental implant assessment by magnetic resonance imaging. J Oral Implantol. 1996;22:147-53.
- [Google Scholar]
- Parameters of radiologic care: An official report of the American academy of oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:498-511.
- [Google Scholar]
- Diagnostic imaging in dental implantology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:540-54.
- [Google Scholar]
- Selection criteria for dental implant site imaging: A position paper of the American academy of oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:630-7.
- [Google Scholar]
- Dosimetry and Cost of imaging osseointegrated implants with film-based and computed tomography. Oral Surg Oral Med Oral pathol Oral Radiol Endod. 1997;83:41-8.
- [Google Scholar]
- Predictable implant placement with a diagnostic/surgical template and advanced radiographic imaging. J Prosthet Dent. 2003;89:611-5.
- [Google Scholar]
- Three dimensional cephalometry: Spiral multi-slice vs cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2006;130:410-6.
- [Google Scholar]
- Computer-guided flapless transmucosal implant placement in the mandible: A new combination of two innovative techniques. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:718-23.
- [Google Scholar]
- The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J. 2007;40:818-30.
- [Google Scholar]
- Craniofacial computed tomography scanning: Technology, applications and future trends. Orthod Craniofac Res. 2003;6(Suppl 1):23-30. Discussion 179-82
- [Google Scholar]






