Translate this page into:
Crohn's disease: Multimodality Imaging of Surgical Indications, Operative Procedures, and Complications
Address for correspondence: Dr. Balasubramanya Kolar, Department of Imaging Sciences, 411 Quinby Road, Rochester, NY-14623, USA. E-mail: balasubramanya_kolar@urmc.rochester.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Surgical management is considered for specific indications in Crohn's disease and a wide variety of surgeries is performed. The purpose of this pictorial essay is to depict manifestations of Crohn's disease that indicates surgery, various surgical procedures that are performed, and the complications arising from these surgical procedures. Surgical indications including obstruction due to strictures or adhesions, fistulae and abscesses, and surgeries for these conditions, such as, ileocecectomy, stricturoplasty, small bowel resection, fecal diversion, segmental colectomy, and lysis of adhesions and their complications will be discussed and their imaging will also be illustrated.
Keywords
Crohn's disease
CT
MRI
INTRODUCTION

Crohn's disease is a chronic granulomatous inflammatory bowel disease that is usually managed medically. Surgery is indicated for complications that do not respond to medical management. Within 13 years of the onset of the disease, an estimated 74% of the cases require surgery. Also, in the subsequent 10-year follow-up period, the rate of relapse is about 30-50%.[12]
Indications for surgery
The first line of treatment for patients with Crohn's disease is medication. When the disease does not respond or when complications arise and there is a need to relieve symptoms, surgery is required [Table 1].
Obstruction
The common indication for surgery includes small bowel obstruction caused by strictures. Twenty-five percent of patients with Crohn's disease undergo surgery for intestinal obstruction. Chronic fibrosis and scarring that do not respond to conservative management necessitates surgery.[2]
Fistulae/Abscesses
Crohn's disease is a transmural inflammatory process. The formation of fistulae or abscesses is relatively common being seen in about 25% of patients.[2] A fistula is an abnormal communication from an abscess to intestines or alternatively fistulae can also connect two adjacent loops of intestine or may connect the intestine to the bladder, vagina, skin, or other organ.
Enterovesical fistulae
These account for 10% of fistulae and are common in the younger age group.[3] Enterovesical fistulae can be detected by injection of contrast through the fistula (fistulogram), MRI, barium studies, or in some cases by CT.
Perianal fistulae
Perianal fistulae are commonly associated with Crohn's disease and are seen in about 43% of patients.[4] These fistulae are classified as inter, supra, trans, or extrasphincteric (Park's classification).[5] However, some fistulae associated with Crohn's disease may be superficial with no relation to the sphincter. Fistulous communications and abscesses are indications for surgical procedures.
Bowel perforation
Bowel perforation is rare (about 1-3%) and is associated with toxic colitis or megacolon. This is an emergent indication for surgery.[2]
Gastrointestinal hemorrhage
This may occur due to the chronic inflammation and the site of bleeding may be localized with angiography or endoscopy.[2] Once the site is localized, resection of the involved segment may be performed.
Surgical procedures performed
Various procedures are performed depending on the underlying condition and location of the lesion. More common procedures include resection of the involved segment and anastomosing different segments of bowel [Table 2].
Strictureplasty
A characteristic finding in Crohn's disease is “skip” lesions with alternating small areas of diseased bowel separated by segments of normal bowel.[6] The areas of active disease may narrow, forming strictures that can cause bowel obstruction. Strictureplasty is usually performed to treat these small involved segments. The strictured area is widened in this procedure without removal of any portion of the small intestine. A lengthwise incision along the narrowed area is made which is then sewed up crosswise.[7]
Resection of intestine and anastomosis
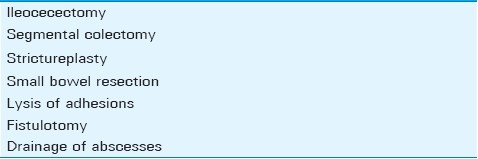
Involvement of a longer segment of intestine or presence of multiple strictures that preclude a simple strictureplasty may necessitate removal/resection of the affected segment of the intestine.[8] The two ends of healthy intestine are then joined together in a procedure called anastomosis. [Figures 1–5]. Perforation is a rarer complication that may also require resection of the involved segment along with washout of the peritoneal cavity [Figure 6].
- (a-d) Line diagrams show ileocolonic anastomosis between ileum and transverse colon.
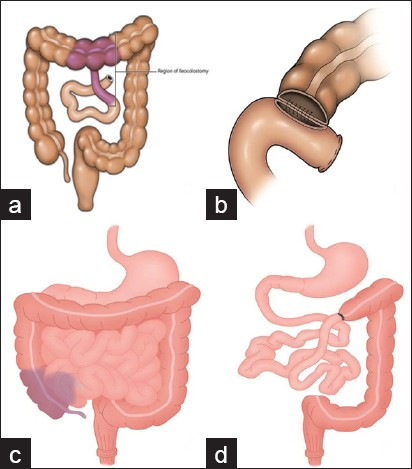
- (a,b) Axial and (d) coronal CT images and (c) barium enema image depict ileocolonic anastomosis.
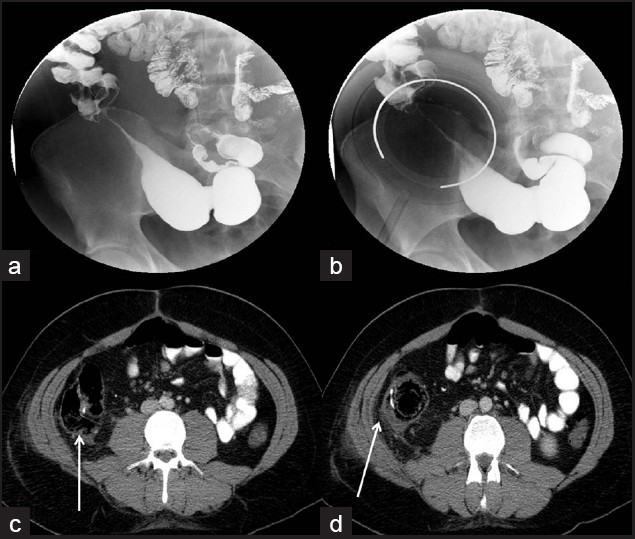
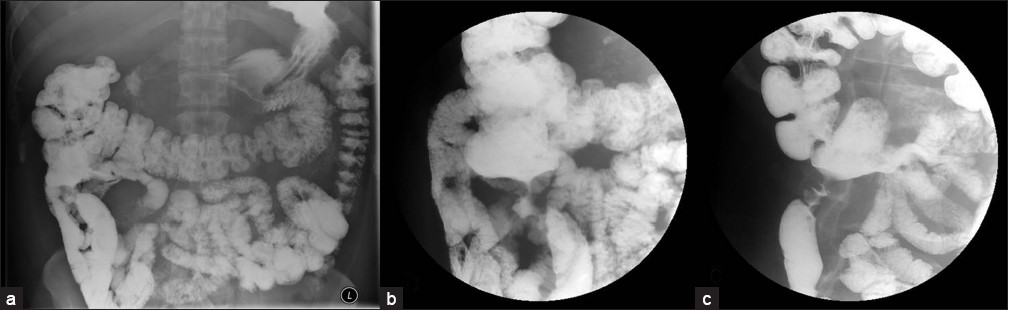
- (a,b) Small bowel follow through shows stricture of ileum in this 16-year-old male patient with Crohn's disease which was surgically managed by ileocecectomy and ileocolonic anastomosis. (c,d) Axial CT images show the anastomosis (arrows) in right lower quadrant.
- (a,b) Long segment stricture of distal ileum in this 21-year-old male patient with Crohn's disease noted on the axial CT images. This was managed by ileocecectomy and ileocolonic anastomosis noted (c) on this barium enema done prior to reversal of ileostomy.

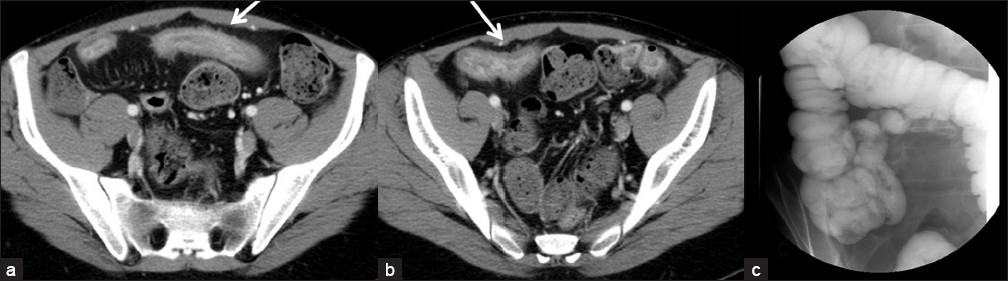
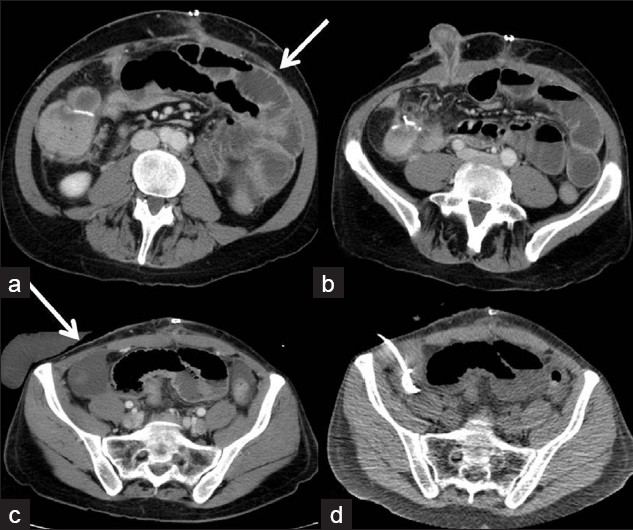
- (a-c) Resection of small bowel with jejunojejunal anastomosis (seen on axial CT images; arrows shows the jejunojejunal anastomosis).
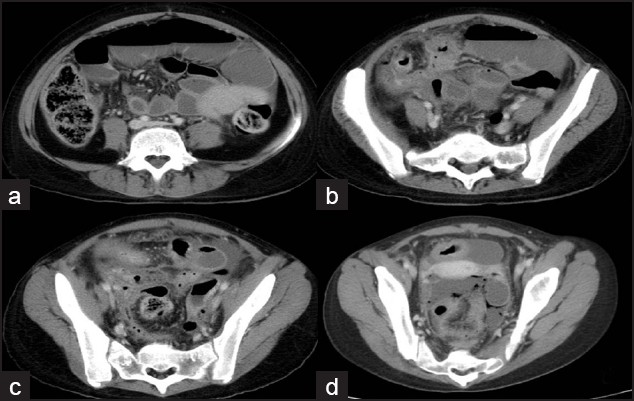
- (a-d) Axial CT images shows dilated small bowel loops along with intraperitoneal/ pelvic free fluid and air; managed by ileocecectomy and ileocolonic anastomosis with washout of abdominal cavity.
Colectomy/Proctocolectomy
Involvement of significant or large segments of the colon may necessitate removal of the colon (colectomy). If the rectum is free of disease, an anastomosis between the ileum and rectum can be performed [Figures 7 and 8].
- Line diagram depicts ileorectal anastomosis.
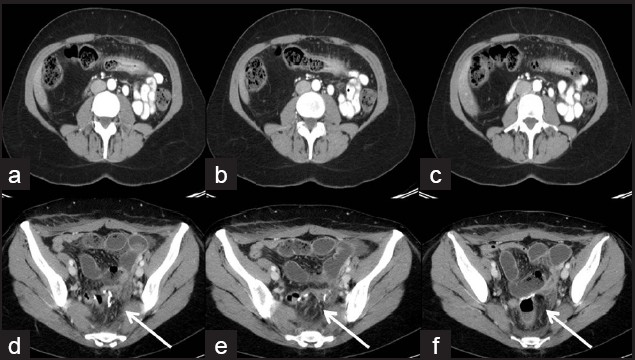
- (a-c) Axial CT images demonstrate thickening of transverse colon in this patient with Crohn's disease; (d-f) Managed by total colectomy with ileorectal anastomosis.
If the rectum is, however, involved, the patients may need a proctocolectomy – a procedure involving the removal of both the colon and rectum. An ileostomy is usually performed in conjunction and involves bringing the end of the small intestine (ileum) through a stoma in the anterior abdominal wall that is usually created in the right lower quadrant.
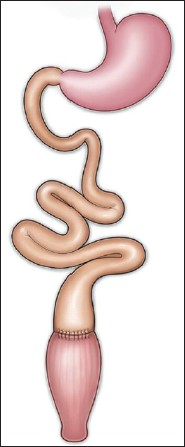
Ileo anal pouch is an anastomosis between the ileum and anus after proctocolectomy. This is usually not indicated for Crohn's disease as the pouch is formed from terminal ileum which increases the possibility of recurrence[9] [Figures 9 and 10].
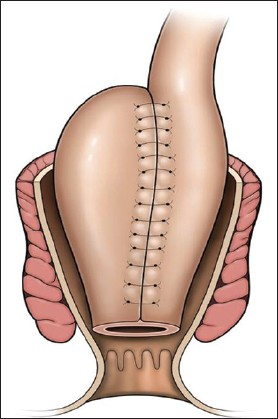
- Line diagram depicts an ileoanal pouch.
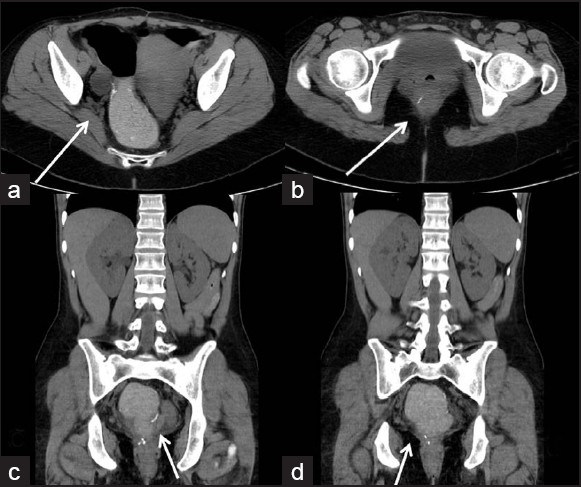
- (a-d) Axial and coronal CT images showing ileoanal pouch after proctocolectomy.
Drainage of abscesses and fistulotomy
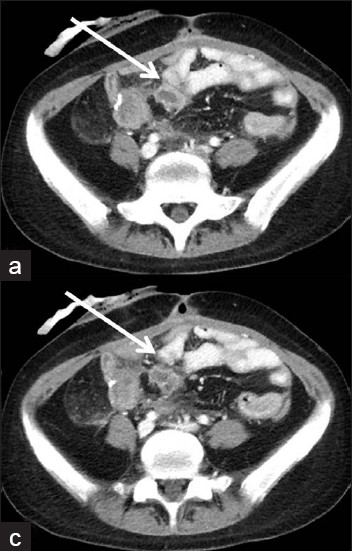
Crohn's disease is also a fistulising disease with fistulae/abnormal communications forming between structures and viscera adjacent to the bowel such as between bowel and skin, bowel and bladder [Figures 11 and 12], or more commonly perianal fistulae [Figure 13]. Resection of the involved bowel and anastomosis is usually performed for fistulae.
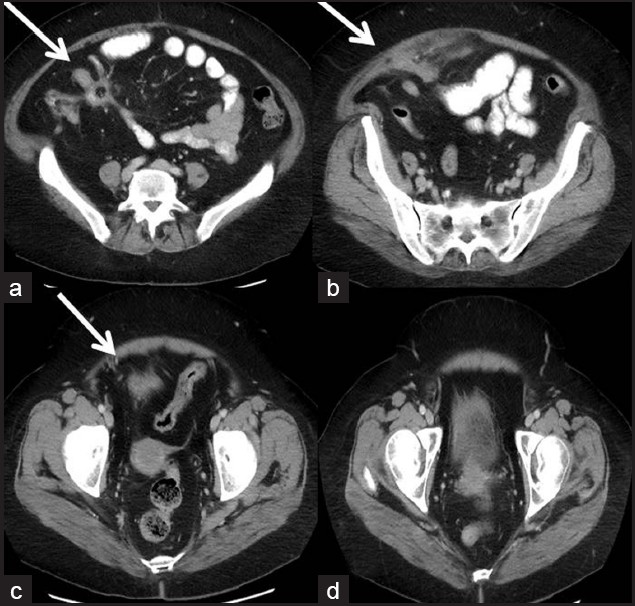
- (a-d) Axial CT images demonstrate thickened ileum with a fistulous track extending into subcutaneous tissue and upto bladder.

- Thirty-two-year old female patient with Crohn's disease complicated by proctoolitis which was managed by total proctoolectomy and ileoanal pouch developed fistula between rectum and vagina. T2-weighted (a) sagittal and (b) axial MR images show the fistulous track (arrows). This was managed by fistulotomy and a gracilis interposition flap seen on (c) axial CT image (arrow).
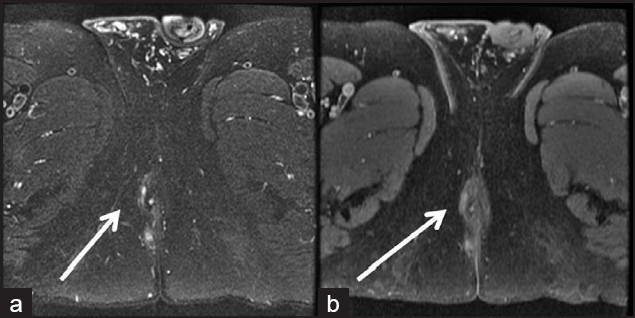
- Thirty-four-year-old male patient with Crohn's disease and perianal fistula seen on (a) MR T2-weighted fat suppressed images as hyperintense areas on the right side with enhancement noted on (b) postcontrast T1-weighted images. Managed by fistulotomy and seton placement.
Perianal fistulae
Perianal fistulae may be managed by placement of seton or fistulotomy. Seton placement involves placement of a suture or drain into the cutaneous orifice of a perianal fistula, traversing the fistula tract into the rectum and exiting through the rectum across the anus, where the two ends of the suture are loosely tied [Figure 14]. Simple trans-sphincteric, intersphincteric, and superficial fistulae can be treated with fistulotomy [Figure 15].[4]
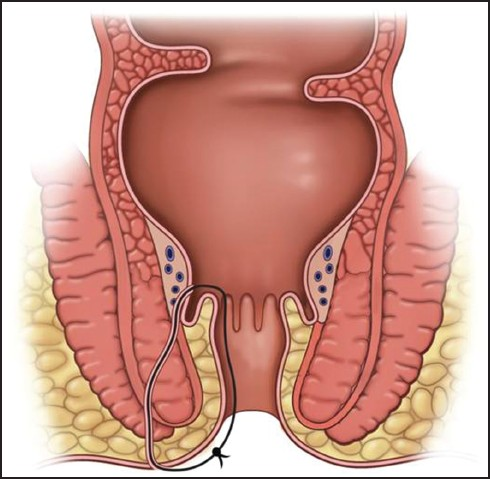
- Line diagram depicts placement of seton.
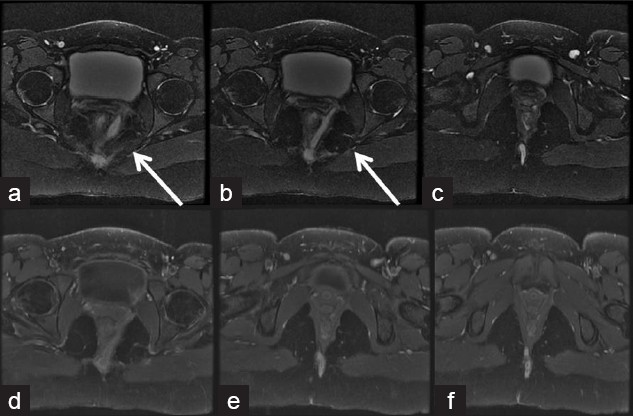
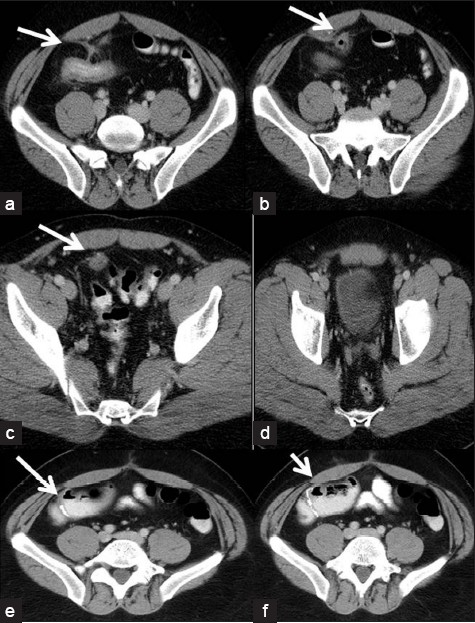
- Twenty-three-year-old female with perianal fistula and perirectal collection seen on (a-c) T2 and (d-f) postcontrast MRI; managed by drainage and seton placement.
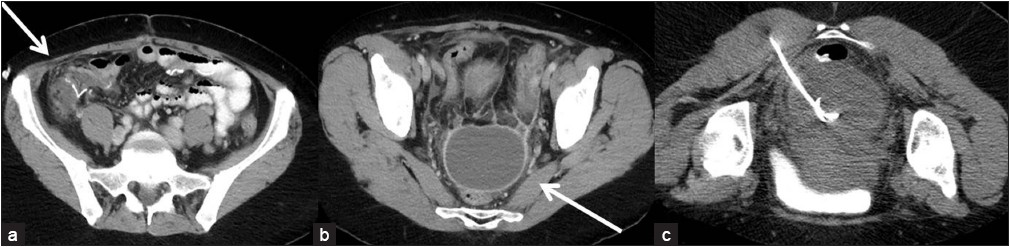
Abscesses can be drained either percutaneously or surgically. Percutaneous drainage involves placement of drainage catheter in appropriate location under imaging guidance such as ultrasound or computed tomography [Figures 16–19].
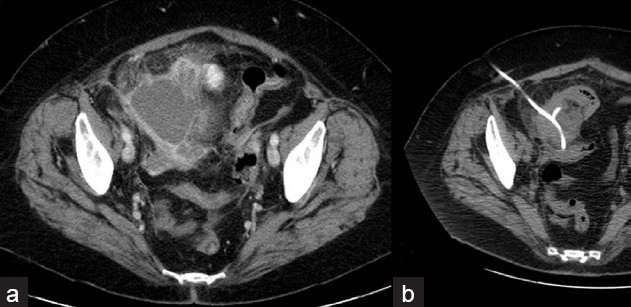
- Sixty-two-year-old lady with Crohn's disease who developed a pelvic abscess, (a) seen on axial postcontrast CT image (b) which was percutaneously drained.
- (a-d) Axial CT images show thickened ileum with a collection/sinus tracking to bladder. Managed by ileocecectomy with drainage of abscess and ileocolonic anastomosis seen on (e-f) axial CT images.
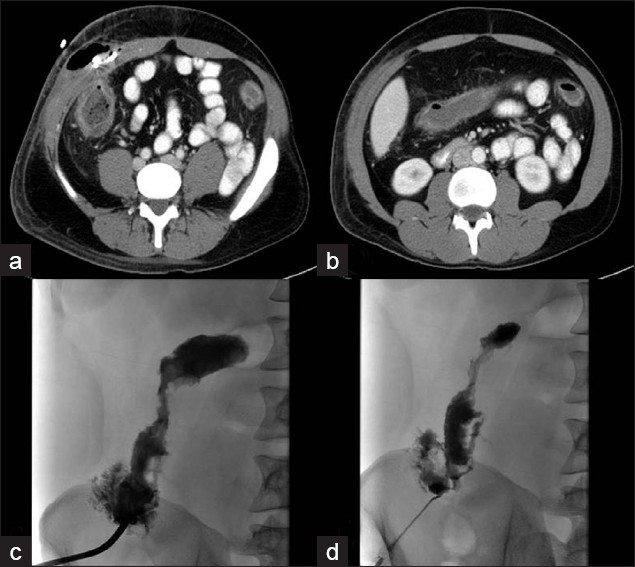
- (a,b) Axial CT images demonstrating the abdominal wall abscess and intraabdominal collection; (c,d) injection of contrast during percutaneous drainage demonstrates connection with colon.

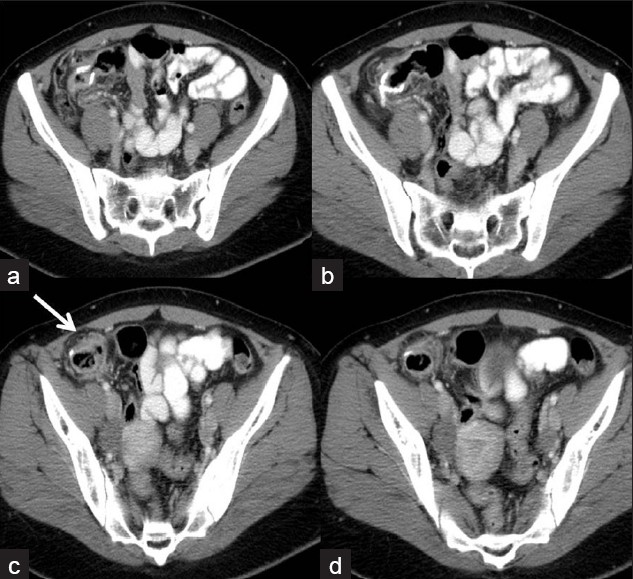
- Twenty-one-year-old female patient with Crohn's disease presenting with right inguinal abscess seen on (a,b) axial MR images as hypointense collection on T1 images which is hyperintense on T2 images. Incision and drainage of abscess done with antibiotics administered. Presented 9 months later with perirectal fistula seen on (c-f) these axial CT images posteriorly on the right side and managed by seton and abscess drainage. The inguinal abscess has completely resolved on these images.
Complications of surgical procedures
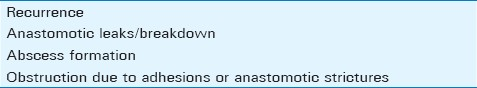
The nature of the disease that is a transmural granulomatous inflammatory process and medications such as immunosuppressants used in its treatment render the patients more prone for complications postsurgical procedures [Table 3].
Symptomatic recurrence is usually seen in approximately 30% of patients at 3 years with the number increasing considerably in 10 years. The region of the anastomosis is the most common site of recurrence. Surgery for recurrence is estimated at 70% in 20 years.[110] In the immediate postoperative period, thickening of the loops may be reactive [Figure 20]. Obstruction of the bowel due to disease recurrence or the presence of extensive adhesions requires surgical correction [Figure 21 and 22].
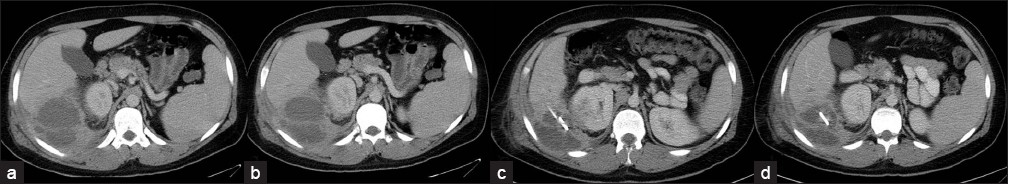
- Mild thickening around recent ileocolonic anastomosis seen on (a-d) these axial CT images which is likely postoperative/reactive
- (a-c) Small bowel series images show narrowing of the ileocolonic anastomosis.
- (a,b) Ileocolonic anastomosis with ileostomy presents with dilated small bowel loops suggestive of obstruction and infected collections adjacent to the anastomosis. (c) Drainage of collection (d) and lysis of adhesions was done.
Infectious complications in the postoperative period in Crohn's disease include sepsis, anastomotic leaks, fistulae, abscesses, and peritonitis. The complications have been attributed to the underlying disease process and treatment with corticosteroids.[11] Most of these major complications require repeat surgery for management [Figures 23–25].
- (a,b) Axial CT images show small fluid collection around site of anastomosis suggesting breakdown.
- (a) Three-weeks postileocolic resection with small collection adjacent to anastomosis and (b) new pelvic collection (c) which was drained percutaneously.
- Sixteen-year-old male patient with history of Crohn's disease, ileocecectomy and ileocolonic anastomosis developed a perihepatic abscess seen on (a,b) axial CT images managed by (c,d) percutaneous drainage.
MR enterography (MRE) is a useful modality and can be a tool for monitoring recurrent disease especially given the radiation risks involved with repeat CT exams in pediatric patients. MRE compares favorably with CT in evaluation of complications of Crohn's disease such as fistula and sinus formation, abscesses, lymphadenopathy, and abnormal fold patterns. It is very useful for assessment of disease activity in the form of bowel wall enhancement, wall thickening, and edema [Figures 26 and 27].[12] MRE may not be sensitive for early disease such as mucosal abnormalities including ulcers that may need a small bowel barium series or endoscopy; however, it is very useful as noted for evaluation of complications such as perianal fistula and recurrence of disease, including assessment of disease activity.
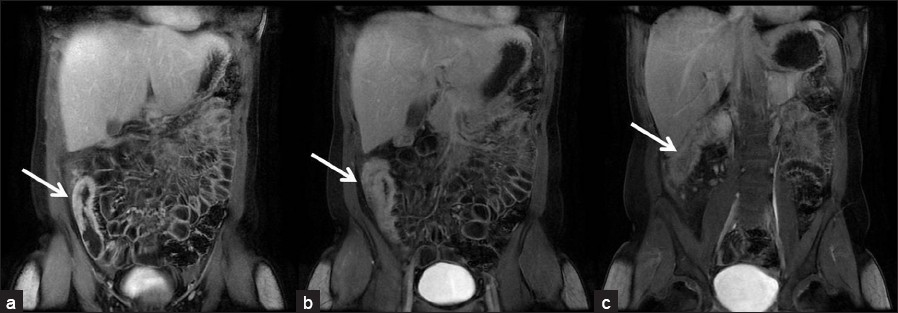
- (a-c) Seventeen-year-old female patient with Crohn's disease. Coronal post-gadolinium T1 images show thick-walled cecum and ascending colon with enhancement indicating active inflammatory disease.
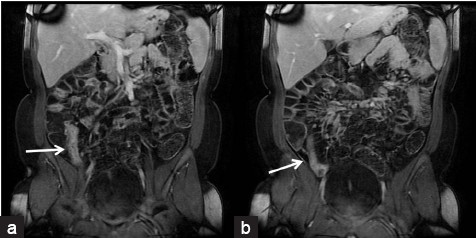
- (a,b) Fifteen-year-old male patient with Crohn's disease. Coronal post-gadolinium T1 images show thick-walled and enhancing terminal ileum indicating active inflammatory disease.
CONCLUSION
Knowledge of surgical indications and their management in Crohn's disease is imperative for a radiologist as it will enable him to recognise imaging appearances of various surgical procedures performed for these indications and identify complications associated with these surgical procedures.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/37/82966
REFERENCES
- Risk factors for surgery and recurrence in 907 patients with primary ileocaecal Crohn's disease. Br J Surg. 2000;87:1697-701.
- [Google Scholar]
- Timing of surgery in Crohn's disease: A key issue in the management. World J Gastroenterol. 2008;14:5532-9.
- [Google Scholar]
- Fistulas of the Genitourinary Tract: A Radiologic Review. Radiographics. 2004;24:1331-52.
- [Google Scholar]
- Diagnosis and treatment of perianal fistulas in Crohn disease. Ann Intern Med. 2001;135:906-18.
- [Google Scholar]
- Gastointestinal tract. In: Semelka Richard, ed. Abdominal- pelvic MRI (Second edition). Hoboken, New Jersey: John Wiley and sons; 2006. p. :677-813.
- [Google Scholar]
- Surgical therapy of recurrent Crohn's disease. In: Holzheimer RG, Mannick JA, eds. Surgical Treatment: Evidence-Based and Problem-Oriented. Munich: Zuckschwerdt; 2001.
- [Google Scholar]
- Surgical management of Crohn's disease. In: Holzheimer RG, Mannick JA, eds. Surgical Treatment: Evidence-Based and Problem-Oriented. Munich: Zuckschwerdt; 2001.
- [Google Scholar]
- Pictorial essay.Radiology of ileal pouch-anal anastomosis surgery. AJR Am J Roentgenol. 2003;180:999-1002.
- [Google Scholar]
- Management and Prevention of Postoperative Crohn's Disease. Inflamm Bowel Dis. 2009;15:1583-90.
- [Google Scholar]
- Corticosteroids and immunomodulators: Postoperative infectious complication risk in inflammatory bowel disease patients. Gastroenterology. 2003;125:320-7.
- [Google Scholar]
- MR enterographic manifestations of small bowel crohn disease. Radiographics. 2010;30:367-84.
- [Google Scholar]






