Translate this page into:
Congenital Agenesis of the Left Lung: A Rare Case
Address for correspondence: Dr. Vefik Arıca, Medical Faculty of the Mustafa Kemal University, Department of Pediatric Clinic, Serinyol, Antakya, Hatay, Turkey. E-mail: vefikarica@hotmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Pulmonary agenesis is a rare congenital anomaly, the etiology of which is not clearly known. Other systemic comorbidities such as cardiovascular, gastrointestinal, musculoskeletal, and urogenital system anomalies can be observed in more than half of the patients. It is usually diagnosed during childhood. Diagnosis in adulthood is very rare. We present a case of pulmonary agenesis diagnosed in an adult.
Keywords
Adulthood
congenital anomaly
pulmonary agenesis
INTRODUCTION

Pulmonary agenesis was first observed in 1673 by Pozze in a female cadaver autopsy. This condition is generally diagnosed in childhood. However, patients without any comorbid anomalies or patients with a mild form of this disease can reach adulthood.[1] It occurs approximately in 1 out of 100,000 births.[2] No significant etiological factors have been found in patients, and thus genetic, teratogenic, and mechanical factors have been thought to be responsible. Since it is rarely observed in adulthood, we present a rare case of of pulmonary agenesis in an adult.
CASE REPORT
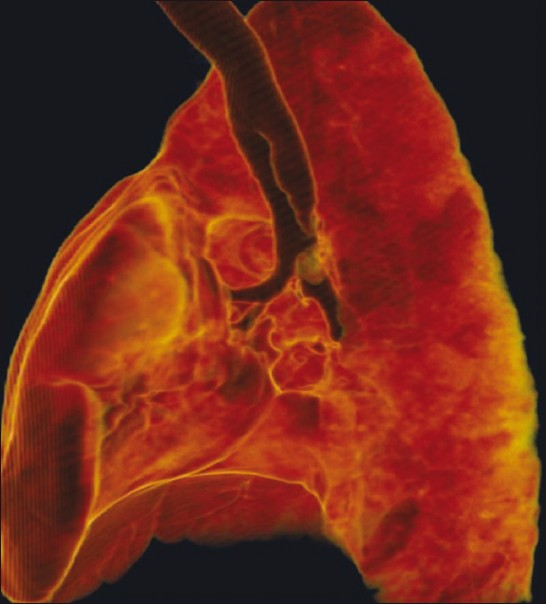
A 17-year-old female patient presented to our clinic with a complaint of shortness of breath. She had a history of frequent infections throughout her childhood. On physical examination, her respiratory sound was found to be reduced in the left hemithorax. Full blood test and routine biochemical test values were within normal limits. P/A chest radiography revealed a deviation to the left in mediastinal structures, trachea, and heart; a narrowing between the ribs in the left hemithorax; a widening between the ribs in the right hemithorax; and elevation of the right hemidiaphragm. Additionally, mild scoliosis was observed [Figure 1]. Spirometry findings was consistent with restrictive disease: FVC: 3.01L (Pred % 67.2), FEV1 2.59L (Pred % 67), and FEV1/FVC: 84.9 (Pred % 102.0). Computed thorax tomography revealed the absence of the left lung parenchyma, deviation of mediastinal structures to the left, a compensatory enlargement of right lung into left hemithorax, and rudimentary bronchus in the left [Figure 2]. Further tests were performed on suspicion of left pulmonary aplasia. The patient underwent thorax CT angiography, abdominal CT, and pulmonary perfusion scintigraphy. In CT angiography, the left pulmonary artery could not be observed [Figure 3]. Rudimentary left vein and bronchus were observed. Furthermore, no parenchymal tissue could be observed in the left lung area [Figure 4]. Perfusion scintigraphy revealed no activity involvement in the left lung.

- Aplasic image of the left lung.
- Rudimentary left main bronchus.

- The image of nonexistent left pulmonary artery and rudimentary left pulmonary vein.

- Left hemithorax; no parenchyma was observed.
DISCUSSION
Pulmonary agenesis means undeveloped pulmonary vessels, bronchi, and parenchyma. It can be unilateral or bilateral. In unilateral aplasia, the remaining lung contains twice as much alveoli as normal, but has normal bronchi.[3] Although aplasia does not have the same structures, it has a rudimentary bronchus. In our case, too, the left main bronchus was determined as rudimentary. As agenesis and aplasia are difficult to distinguish from each other clinically and pathologically, they are often used in the same sense. On the other hand, pulmonary hypoplasia is characterized by immature lung tissue or by lung tissue decreased at varying degrees.[14] Pulmonary aplasia (agenesis) is thought to result from the negative effects that occur on the 4th week of fetal life. Although its etiology is not fully understood, Vitamin A or folic acid deficiency or the use of salicylates may be responsible for it.[4] Its incidence in males and females and the occurrence of the anomaly in the right or left lung are about the same.[5] Hypoplasia and aplasia are often observed together with other malformations (diaphragma defects, kidney anomalies, extrapulmonary sequestration, muscle, or skeleton system defects). Nearly one-third of the patients have congenital heart diseases. Although the most common one is the atrial septal defect, ventricular septal defect, patent ductus arteriosus, or aorta coarctation can also be observed.[6] In our case, too, no pathological findings were found except scoliosis. Aplasic patients are usually asymptomatic. Clinical findings change with the presence of comorbid anomalies and their severity. Recurrent infections can increase the breathing distress. Although the patients with unilateral lung aplasia (agenesis) are believed to die usually in the neonatal period, there are patients who live upto the adulthood, some of whom live without any symptoms.[1] Our patient had been asymptomatic for years. Pulmonary aplasia (agenesis) can cause a predisposition to infections. In aplasia, secretions not cleared from the rudimentary bronchus and/or comorbid bronchiectasis may partially be responsible for the risk of infection.[15] In our case, bronchus was rudimentary and an antibiotic treatment was started to clear the symptoms of a respiratory tract infection. In some cases, a significant decrease in vital capacity and exercise intolerance can be seen. Chronic respiratory failure and eventually respiratory infections can develop in adults.[7] The restrictive pattern detected in our case was thought to be secondary to the aplasic lung disorder. In the diagnosis of this condition, methods such as contrast-enhanced CT, bronchography, bronchoscopy, pulmonary angiography, and magnetic resonance imaging are also employed.[89] In our case, the diagnosis was made with noninvasive methods such as thorax CT-angiography and ventilation/perfusion scintigraphy. In chest radiography, mediastinum is observed to deviate to the adverse side. Narrowing between the ribs and elevated hemidiaphragm on this side is also observed.[1] In our case, CT revealed rudimentary bronchus, but no bronchiectasis was observed. Right pulmonary artery was quite long, left pulmonary artery did not exist, and the bronchus was rudimentary. No parenchymal tissue was detected in the left lung area. Heart and the main vascular structures were observed to move into left mediastinum. Bronchoscopy was not required. Total atelectasia, diaphragmatic hernia, diaphragmatic eventration, pneumonia, pleural effusion, pulmonary hypoplasia, or pneumonectomy should be considered in the differential diagnosis.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2011/1/1/47/85175
REFERENCES
- Pulmonary Abnormalities of Developmental Origin. In: Synopsis of Diseases of the Chest (2nd ed). Phildelphia: W. B. Saunders Company; 1994. p. :25686.
- [Google Scholar]
- Unilateral pulmonary agenesis without mediastinal displacement. South Med J. 1997;90:3357.
- [Google Scholar]
- Right-sided pulmonary aplasia: Longitudinal lung function studies in two cases and comparison to results from term healthy neonates. Pediatr Pulmonol. 1998;26:13844.
- [Google Scholar]
- Radiology of the diaphram, pleura, thoracic cage and upper air passages. In: Meschan I, Farrer Meschan RM, eds. Roentgen signs in diagnostic imaging Vol 4. (2nd ed). Philadelphia: WB Saunders Co; 1987. p. :120220.
- [Google Scholar]
- Prenatal diagnosis of isolated unilateral pulmonary agenesis in the second trimester. Ultrasound Obstet Gynecol. 2002;19:2067.
- [Google Scholar]
- Case report: Agenesis of the right lung diagnosed by threedimensional reconstruction of helical chest CT. Br J Radiol. 1996;69:10524.
- [Google Scholar]
- MR evaluation of right pulmonary agenesis and vascular airway compression in pediatric patients. AJR Am J Roentgenol. 1997;168:558.
- [Google Scholar]






