Translate this page into:
Computed tomography and magnetic resonance imaging features of abdominal and pelvic leiomyomatosis peritonealis disseminata: A retrospective observational study

*Corresponding author: Ling Yang, Department of Radiology, The First Affiliated Hospital of Soochow University, Suzhou, China. yanglingsdfyy@163.com
-
Received: ,
Accepted: ,
How to cite this article: He X, Ma X, Jiang N, Weng C, Yang L. Computed tomography and magnetic resonance imaging features of abdominal and pelvic leiomyomatosis peritonealis disseminata: A retrospective observational study. J Clin Imaging Sci. 2025;15:6. doi: 10.25259/JCIS_144_2024
Abstract
Objectives:
Leiomyomatosis peritonealis disseminata (LPD) is a rare and specific type of leiomyomatosis that is often misdiagnosed as malignant tumor with peritoneal metastasis, and accurate diagnosis is critical to treatment planning. The purpose of this study is to investigate the radiological features of LPD, analyze, and summarize its differential diagnosis and clinical features to improve the understanding of this rare disease.
Material and Methods:
A retrospective analysis was conducted on clinical and radiological features from 10 patients with pathologically confirmed LPD between 2012 and 2024. The computed tomography (CT) and magnetic resonance imaging (MRI) findings were examined, focusing on parameters such as location, morphology, size, quantity, enhancement patterns, and their relationship with adjacent organs. In addition, the radiological features and the key points of differential diagnosis were summarized.
Results:
All the 10 LPD patients presented with multifocal lesions in the abdomen and pelvis, and 7 of them had a history of hysteromyoma surgery. The number of lesions was all ≥2, most of them were round or quasi-circular, with clear boundaries and smooth edges, did not invade the neighboring parenchymal organs, with a length of about 1.5~16.8 cm. The lesions were located in the pelvic cavity in 6 cases, the abdominal wall in 6 cases, the intestinal wall in 3 cases, the rectouterine pouch in 1 case, the omentum in 5 cases, the abdominal cavity in 1 case, and the mesentery in 1 case. There were 7 cases with minimal pelvic fluid and 1 case with liver spread. CT showed circular solid nodules with clear boundaries. The density of small lesions was homogeneous. Cystic changes were observed in some large lesions. On MRI, T1-weighted imaging showed hypo to isointense, T2-weighted imaging (T2WI) mostly showed hypointense, and T2WI in some large lesions showed slightly high signal intensity, diffusion-weighted imaging signal intensity was not higher than that of myometrium, apparent diffusion coefficient showed isointense, and solid components of the lesions were significantly more homogeneous enhanced after enhancement, and the enhancement degree was similar to that of normal myometrium.
Conclusion:
Although the imaging findings of LPD are similar to malignant tumors with peritoneal implantation and metastasis, they have certain characteristics, which are helpful for differential diagnosis combined with the clinical history of patients.
Keywords
Leiomyomatosis peritonealis disseminata
Differential diagnosis
Peritoneal tumor
INTRODUCTION
Leiomyomatosis peritonealis dissemination (LPD) is a rare and specific type of leiomyomatosis that was first reported in 1952[1] and officially named by Taubert et al. in 1965.[2] This disease is most common in premenopausal women and is characterized by the presence of multiple masses or nodules within the abdomen, pelvis, and periperitoneal space. It is frequently misdiagnosed as a malignant tumor with peritoneal implantation and metastasis before surgical intervention. This study retrospectively analyzed and summarized the imaging findings along with clinical data from 10 cases of LPD, while also reviewing pertinent literature to enhance understanding of this disease, provide valuable references for clinical diagnosis and treatment, and mitigate instances of misdiagnosis and mistreatment.
MATERIAL AND METHODS
Patient selection
This retrospective study was approved by the Ethics Review Board of The First Affiliated Hospital of Soochow University (No. 2024538). A retrospective analysis was conducted on 10 female patients diagnosed with LPD through postoperative pathology, who were admitted to the First Affiliated Hospital of Soochow University between December 2012 and June 2024. They were all female, and the ages of the patients ranged from 21 to 56 years, with a median age of 46 years. Clinical presentations included abdominal pain in 2 cases, irregular vaginal bleeding accompanied by odor in 1 case, while other seven cases exhibited no significant clinical symptoms, and the lesions were found by routine physical examination after operation. Notably, 7 patients had a history of hysteromyoma surgery, among these, five underwent laparoscopic myomectomy, with lesions identified 4–12 years post last myoma operation. Carbohydrate antigen 125 (CA 125) levels were elevated in 5 cases (50.60 U/mL, 139.7 U/mL, 106.4 U/mL, 70.10 U/mL, and 349.6 U/mL; normal range: 0–35 U/mL), while carbohydrate antigen 199 (CA 199) was elevated in 2 cases (40.09 U/mL and 55.85 U/mL; normal range: 0-37 U/mL). Of these patients, seven underwent enhanced total abdominal computed tomography (CT) scans at our hospital and four received pelvic magnetic resonance imaging (MRI) examinations.
CT and MRI technique
CT: The patients underwent CT on Philips iCT 256 or Siemens SOMATOM Definition dual-source CT. The tube voltage was 120 kV and the tube current was used by automatic mA technology. After normal scan, non-ionic contrast agent isohexyl alcohol was injected through the cubical vein with a dose of 1–1.5 mg/kg and a flow rate of 3 mL/s. Images of arterial and venous phases were collected 25 s and 90 s after injection.
MRI: The patients underwent MRI on GE Signa Premier 3.0T or Philips Ingenia magnetic resonance scanners with the phased alignment circle of the torso. The scanning sequences included T1-weighted imaging (T1WI), T2-weighted imaging (T2WI), and diffusion-weighted imaging (DWI) with a thickness of 5 mm. Gadopentetate Dimeglumine (GdDTPA) (0.1 mmol/kg) was injected into the elbow vein with a flow rate of 2.0~2.5 mL/s using a high-pressure syringe. After the injection, 15–20 mL normal saline was injected rapidly.
Image analysis
The radiological features were independently analyzed by two experienced radiologists (both with over 10 years of diagnosis experience, receptively) who subspecialty trained in abdominal imaging, without access to any patient information or pathological results. If any discrepancies arose, a consensus was reached through consultation. The radiological features assessed included the lesion location, number, morphology (quasi-circular/irregular), size, boundary, density/signal, enhancement mode, enhancement degree, etc., and to evaluate whether there was calcification and cystic change in the lesions, invasion of neighboring organs, and lymph node metastasis. At least three largest lesions were selected for each patient, and region of interest (ROI) was placed on the largest cross section, avoiding necrosis and calcification. Three ROIs were selected for each section to calculate the average value. The measured parameters included (1) the CT attenuation values on non-enhanced phase, arterial phase, and venous phase; (2) ΔCT attenuation value on arterial phase and venous phase (ΔCT attenuation value = CT attenuation value on arterial/venous phase-CT attenuation value on non-enhanced phase); (3) apparent diffusion coefficient (ADC) values of LPD lesions and normal myometriums.
Statistical analysis
All the statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) software (version 26.0, SPSS, IBM). Quantitative data with a Gaussian distribution are presented as mean ± standard deviation, and quantitative data with non-normal distributions are presented as median with interquartile range. The independent-sample t-test or Mann–Whitney U test was used to compare the quantitative parameters. A two-sided P <0.05 was considered statistically significant.
RESULTS
Number and distribution of lesions: All the 10 patients presented with multiple lesions. The maximum cross-sectional diameter of the lesions ranged from approximately 1.5 cm to 16.8 cm, with a mean of 9.3 cm and a median of 7.9 cm. Lesions were identified in the pelvic cavity (6 cases), abdominal cavity (1 case), abdominal wall (6 cases), intestinal wall (3 cases), rectouterine pouch (1 case), omentum (5 cases), and mesentery (1 case). Each lesion exhibited smooth edges and well-defined boundaries relative to adjacent organs. In instances where the lesions were larger, they pressed and pushed surrounding tissues without invading parenchymal organs, the perilesional fat space remained clear, and no significant enlarged lymph nodes were observed. Seven patients were accompanied by a small amount of pelvic effusion, and one patient demonstrated hepatic dissemination [Figure 1]. The clinical data and radiological features of the 10 patients were summarized in Table 1.
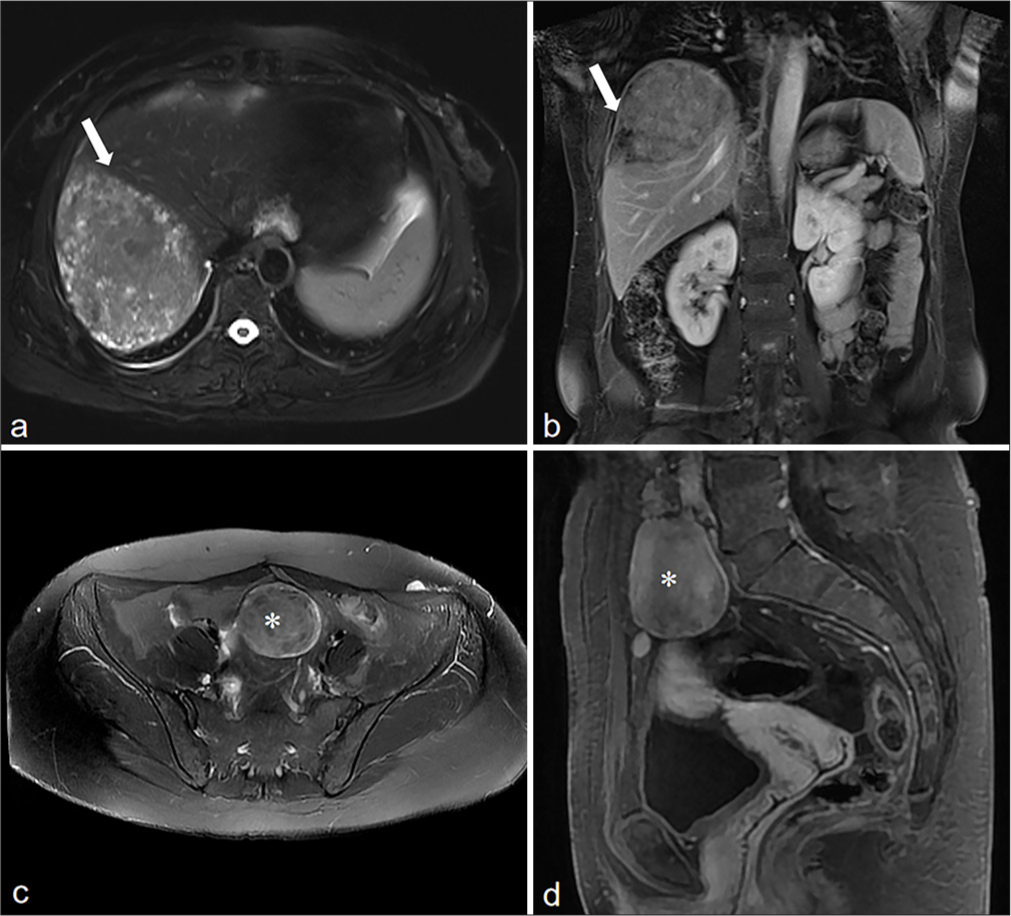
- A 54-year-old woman with LPD, who had a history of laparoscopic myoma resection more than 10 years ago. (a and b) MRI T2WI images showed a slightly hyperintensity mass in the liver with smooth edges (white arrow), and showed uneven enhancement. (c and d) Soft tissue masses (*) were also seen in the abdomen and pelvis, with smooth edge, whose signal and enhancement mode were similar to the liver lesion (white arrow which is only present in a and b). (LPD: Leiomyomatosis peritonealis disseminata, MRI: Magnetic resonance imaging, T2WI: T2-weighted imaging).
| Patient | Age | History of hysteromyoma | Recurrence interval (year) | Symptoms | Location of lesions | Number of lesions | Maximum lesion size (mm) | Density/Signal intensity | Enhancement patterns |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 56 | - | - | - | Anterior and posterior wall of uterus, rectouterine pouch, omentum | 4 | 51.7×46.9×61.8 | T1WI isointensity, T2WI hypointense | Slightly- moderately heterogeneous enhancement |
| 2 | 48 | - | - | Abdominal pain | Uterus, mesentery, intestinal wall, pelvic cavity | >20 | 106×113×132 | CT homogeneous density/T1WI isointensity, T2WI slightly hyperintense | Obviously homogeneous enhancement |
| 3 | 44 | LM | 11 | - | Pelvic cavity, intestinal wall, abdominal wall, omentum | 4 | 63×52×63 | T1WI slightly hypointense, T2WI isointensity | Obviously homogeneous enhancement |
| 4 | 46 | TVM, TAM | 8 | - | Uterus, omentum, abdominal wall, pelvic cavity | >10 | 15×19×22 | CT homogeneous density | Obviously homogeneous enhancement |
| 5 | 39 | LM, TAH | 9 | - | Pelvic cavity, intestinal wall | 3 | 71×55×76 | CT homogeneous density | Slightly heterogeneous enhancement |
| 6 | 21 | LM | 4 | - | Pelvic cavity, omentum, left abdominal wall | 13 | 40×28×79 | CT homogeneous density | Slightly- moderately heterogeneous enhancement |
| 7 | 47 | TAH | 12 | - | Anterior abdominal wall, pelvic cavity | 3 | 70×80 | CT heterogeneous density | Obviously heterogeneous enhancement |
| 8 | 54 | LM | 10 | Abdominal pain | Left abdominal wall, omentum, pelvic cavity, liver | 8 | 57.9×41.3×48.5 | T1WI isointensity, T2WI slightly hyperintense | Obviously homogeneous enhancement |
| 9 | 50 | LM | 8 | Irregular vaginal bleeding with odor | Uterus, abdominal wall | >10 | 168×106×149 | CT heterogeneous density | Slightly- moderately heterogeneous enhancement |
| 10 | 40 | - | - | - | Uterus, abdominal cavity | 3 | 130×88×162 | CT heterogeneous density | Moderately heterogeneous enhancement |
LM: Laparoscopic myomectomy, TVM: Transvaginal myomectomy, TAM: Transabdominal myomectomy, TAH: Total abdominal hysterectomy, CT: Computed tomography, T1WI: T1-weighted imaging, T2WI: T2-weighted imaging, LPD: Leiomyomatosis peritonealis disseminate
CT findings: All 7 patients who underwent CT examination presented with round solid nodules or masses characterized by well-defined margins. The smaller lesions exhibited isodensity on the non-enhanced phase and demonstrated homogeneous enhancement on both the arterial and venous phases. Cystic lesions were identified in 5 cases. As illustrated in Table 2, the non-enhanced CT attenuation value of the solid component of these lesions was measured at 44.21 ± 4.57 Hounsfield Unit (HU), while that of the arterial phase was 66.65 ± 13.91 HU. Notably, the ΔCT attenuation value of normal myometrium on the arterial phase was found to be 67.40 ± 11.83 HU, which is comparable to that of LPD lesions (66.65 ± 13.91 HU), with no statistically significant difference observed (P = 0.74). Solid components exhibited mild enhancement in 4 cases and moderate enhancement in 3 cases, exhibiting a degree of enhancement similar to that of normal myometriums [Figure 2]. The CT attenuation value for the solid portion on venous phase was 91.44 ± 19.36 HU, no significant enhancement was noted within cystic areas, and there was no statistical difference in ΔCT attenuation values between myometrium and lesions on venous phase (P = 0.65).
| ADC (×10-3 mm2/s) | CT attenuation value (HU) | ΔCT attenuation value (HU) | ||||
|---|---|---|---|---|---|---|
| Non-enhanced phase | Arterial phase | Venous phase | Arterial phase | Venous phase | ||
| Myometrium | 1.69±1.67 | 47.93±9.18 | 67.40±11.83 | 101.33±20.07 | 19.47±17.00 | 53.40±25.97 |
| LPD | 1.49±0.30 | 44.21±4.57 | 66.65±13.91 | 91.44±19.36 | 22.44±13.66 | 47.23±20.18 |
| P-value | 0.31 | 0.44 | 0.92 | 0.41 | 0.74 | 0.65 |
| t-value | 1.09 | 0.84 | 0.1 | 0.86 | −0.34 | 0.47 |
ADC: Apparent diffusion coefficient, CT: Computed tomography, HU: Hounsfield unit, LPD: Leiomyomatosis peritonealis disseminata
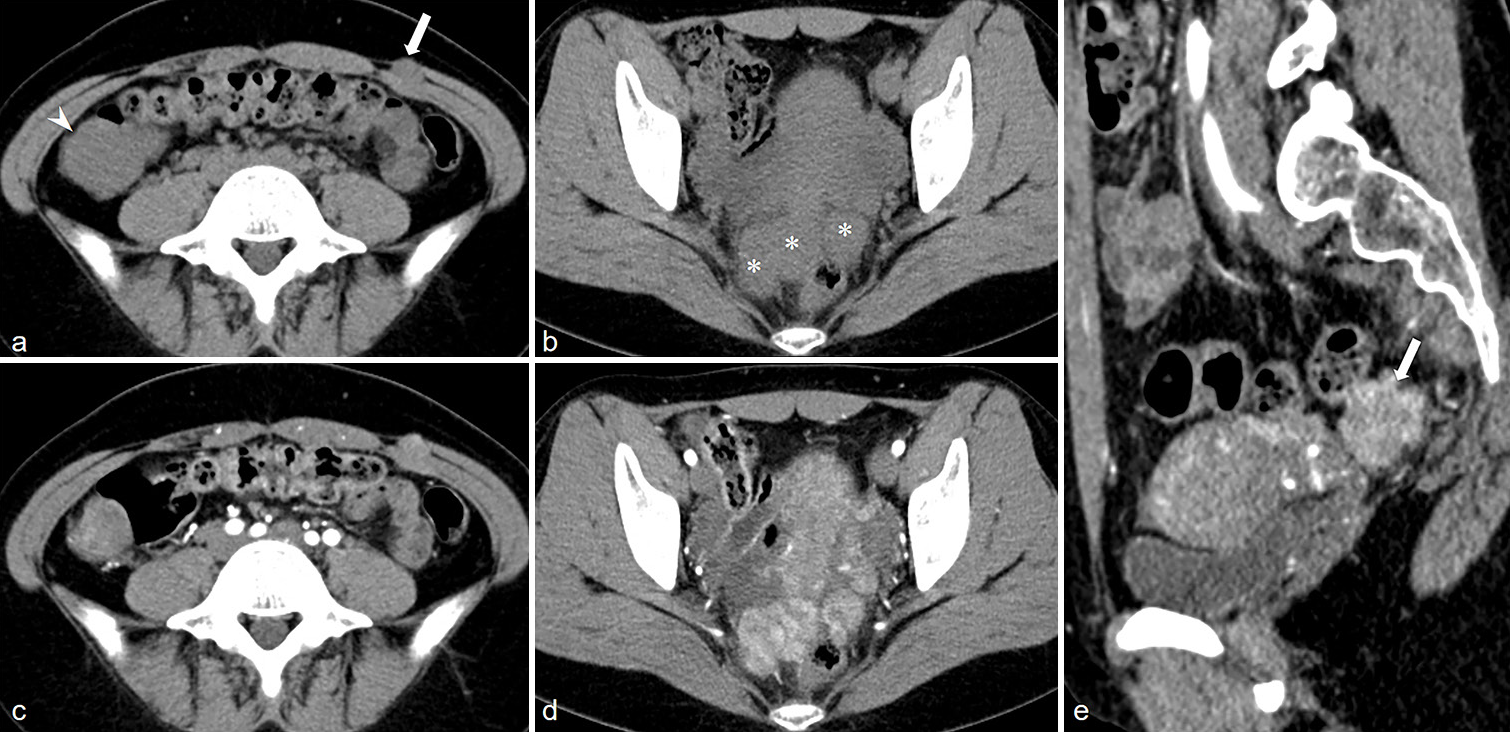
- A 21-year-old woman with LPD. (a) Axial non-enhanced CT image showed soft tissue nodules in the left abdominal wall (white arrow), right abdominal cavity (white arrowhead) . (b) Axial non-enhanced CT image showed multiple soft tissue nodules in the rectouterine pouch (*) with uniform density. (c and d) Axial CT images on arterial phase showed slightly heterogeneous enhancement in the lesions, and the enhancement patterns of all lesions were similar. (e) Sagittal CT images on arterial phase, and the enhancement of the lesion was similar to that of the myometrium (white arrow). (LPD, Leiomyomatosis peritonealisis disseminata; CT, Computed tomography.)
MRI findings revealed that all lesions from 4 patients exhibited isointensity or hyperintensity on T1-weighted imaging (T1WI) and hypointensity on T2-weighted imaging (T2WI). Two patients demonstrated slight hyperintensity on T2WI. The diffusion weighted imaging (DWI) signals were not elevated compared to those of the normal myometrium. Notably, the solid components of the lesions demonstrated significantly more homogeneous enhancement post-contrast administration, with enhancement levels comparable to those of the normal myometrium. The results indicated that the apparent diffusion coefficient (ADC) value for normal myometrium was 1.69 ± 1.67×10−3 mm2/s, whereas for LPD lesions, it was 1.49 ± 0.30×10−3 mm2/s, and no statistically significant difference was observed between them (P = 0.31). Typical cases are shown in Figure 3.
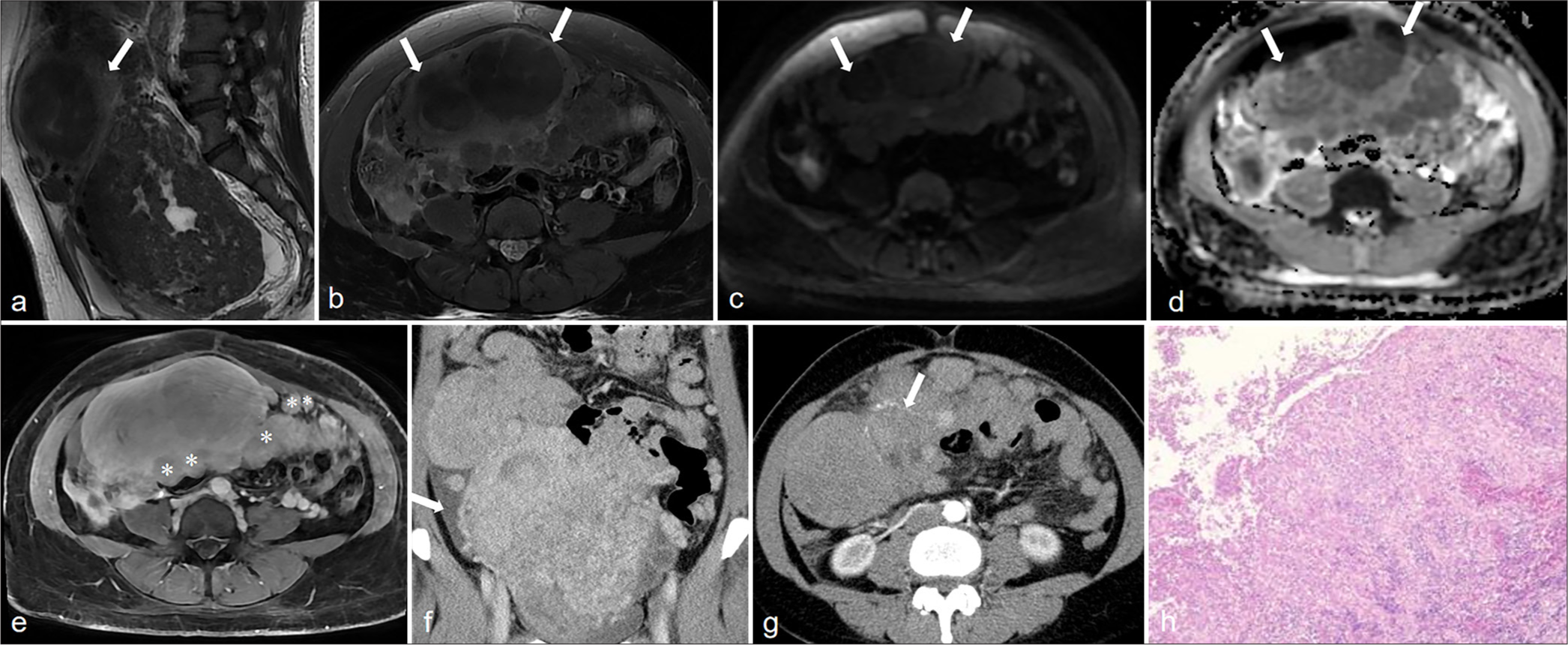
- A 48-year-old woman with LPD. (a) Axial T1WI image showed a hypointense soft tissue mass in the abdominal cavity (white arrow). (b) The lesion edge showed high signal intensity on Axial T2WI image (white arrows). (c) The DWI showed isointense (white arrows). (d) The ADC showed hypointense (white arrows). (e) There were also many nodular abnormal signals in the abdominal cavity (*), some of which were closely related to the peritoneum, and obvious homogeneous enhancement was observed; (f) On the CT venous phase, the huge mass in the abdomen cavity showed uneven and obvious enhancement, and a small amount of fluid (white arrow) could be seen in the abdominal cavity. (g) The lesions on the CT arterial phase showed patchy enhancement with vascular shadows (white arrow). (h) The microscope showed that the tumor was composed of spindle cells (Hematoxylin and eosin, ×40 magnification). (LPD: Leiomyomatosis peritonealis disseminate, MRI: Magnetic resonance imaging, T1WI: T1-weighted imaging, T2WI: T2-weighted imaging, DWI: Diffusion weighted imaging, ADC: Apparent diffusion coefficient).
Pre-operative imaging diagnosis included uterine fibroids with malignant metastasis (1 case), ovarian origin malignant tumor with metastasis (5 cases), follicular membrane fibroma (1 case), endometriosis with abdominal wall implantation (1 case), broad ligament fibroids or stromal tumors (1 case), and vascular lesions (1 case).
DISCUSSION
LPD is a rare and specific type of leiomyomatosis, with its precise pathogenesis remaining elusive. It may be associated with hormonal fluctuations, the utilization of oral contraceptives, genetic predispositions,[3] and iatrogenic transmission.[4] In recent years, with the wide application of minimally invasive techniques, the incidence of LPD in patients after laparoscopic myomectomy has increased.[5] Reviewing the previously reported LPD cases, most of the patients had a history of laparoscopic myomectomy, and 50% of the patients in our group had also undergone this operation.
Previous studies have reported that LPD is prevalent among women with elevated estrogen levels, and the development of proliferative leiomyoma nodules may be attributed to the abnormal effects of estrogen and progesterone, as well as metaplasia of subperitoneal mesenchymal stem cells, leading to the formation of smooth muscle cells, fibroblasts, myofibroblasts, and decidual cells.[6] Some studies also believe that LPD is related to X chromosome inactivation and chromosome karyotype abnormality.[7] The clinical manifestations were mostly non-specific, and most patients were treated for abdominal pain, abdominal distension, abdominal mass, and other symptoms. Microscopic nodules are composed of fusiform smooth muscle cells, occasionally containing fibroblasts and myofibroblasts, without atypia or mitosis, and their morphological arrangement is similar to typical uterine leiomyomas in a swirling shape.[8,9] Most of the tumor indicators in laboratory examination show no abnormality or slight increase. If these indicators are elevated, it is easy to consider abdominal metastases, leading to misdiagnosis.[8] Previously reported cases CA199 and CA125 were mostly normal or slightly elevated.[10-12] However, one patient in our group had a high CA125 of 349.6 U/mL (0–35 U/mL), but this patient had a history of breast cancer, and the post-operative pathology showed abundant fibroid cells and active mitotic images, which may be the cause of the increase in tumor indicators. Pre-operative qualitative diagnosis of LPD has always been a difficult problem, and its imaging features can provide an important reference for clinical treatment and surgical planning.
By reviewing the relevant literature of LPD and combining with our experience, we summarize its radiological features as follows: (1) it mostly occurs simultaneously in the uterus and periperitoneal organs, showing multi-focal distribution, and the number of lesions is generally relatively large. This characteristic distinguishes it from leiomyosarcoma, in which the lesions are typically few in number but large in size, and possess the ability to infiltrate adjacent tissues.[13] (2) The lesions of LPD exhibit well-defined margins, a regular morphology, and homogeneous signal/density and typically demonstrate homogeneous enhancement, with both the pattern and degree of enhancement closely resembling those of normal myometrium. There was no statistically significant difference in ΔCT attenuation values between normal myometrium and lesions of LPD in our group. Furthermore, owing to their homology, the imaging characteristics of the lesions exhibited notable similarities.[3] Nevertheless, the presence of necrosis, cystic transformations, or the implantation of endometrial elements within certain larger lesions may result in heterogeneous enhancement,[14] similar to the enhancement patterns of primary or metastatic peritoneal carcinoma.[15] Ye and Chen[16] reported a case of LPD patient with low-grade malignant transformation, whose lesion showed heterogeneous enhancement, which was similar to the enhancement pattern of a patient with elevated tumor indicators in our group. The post-operative pathological examination also indicated that the LPD lesions of this patient had abundant cells under the microscope and mild atypia. However, the risk factors for malignant transformation of LPD are still unclear. At this time, the peritoneal metastasis caused by malignant tumor has unclear boundary, irregular shape, diffuse thickening of peritoneum, and indirect malignant signs such as enlarged lymph nodes and massive abdominal and pelvic effusion can help to distinguish it to a certain extent. (3) LPD does not invade adjacent parenchymal organs, and the surrounding structure is clear. Most lesions of LPD located in the pelvis involved ovaries, and pre-operative diagnosis was difficult. In our group, 5 cases were misdiagnosed as malignant tumors of ovarian origin with metastasis before surgery. However, based on the pathogenesis of LPD, the signals of the patient’s ovarian parenchyma and follicle are clear and inviolable,[3] which can be used as the key points for identification. (4) Most lesions were isointense or mildly hypointense on T1WI and showed hypointense on T2WI, which is due to the fact that the lesions contain more fiber components.[17] Different from peritoneal carcinoma and leiomyosarcoma, T2WI of the latter two usually shows slightly high signal intensity,[8] indicating the hypercellular or hypervascular nature of the lesions.[18] A retrospective analysis of the cases in our group showed that the imaging features were similar to those reported in previous literature. CT findings of multiple abdominal and pelvic lesions were mostly solid nodules or masses, with cystic changes in some of them, and the enhancement pattern was similar to that of the myometrium. T2WI signal intensity is not high, and diffusion is not significantly limited. The mesenteric adipose space and its structure were clear, there was no obvious swelling of surrounding lymph nodes, no thickening of peritoneum, no omental cake sign, and the boundary between the mesenteric organs was clear. 7 cases had a little pelvic effusion.
The incidence of LPD is low, and few cases have been reported so far. Moreover, the location of lesions occurred mostly in abdomen and pelvis, but rarely in other parts. One patient from our group developed benign liver dissemination. The patient underwent an MRI examination and found a hepatic mass, leading to a pre-operative diagnosis of metastatic tumor. However, post-operative pathology confirmed the presence of leiomyoma dissemination. A retrospective analysis of the patient’s imaging indicated that the MRI signals and enhancement patterns of the liver lesions closely resembled those of uterine fibroids. In addition, multiple nodules of varying sizes were observed within the abdominal and pelvic cavities, aligning with characteristic imaging findings typical of LPD. After referring to relevant literature, we found that LPD lesions found in the liver are very rare. In January 2024, Nduwimana et al.[19] reported a case of LPD patient with liver spread. Notably, the imaging characteristics of the hepatic mass bore resemblance to multiple uterine leiomyomas and were accompanied by several small peritoneal nodules consistent with our case report.
Previous literature has noted instances where LPD coexists with endometriosis[20,21] or gastrointestinal stromal tumors (GISTs),[22] although no such cases were identified within our group. Endometriosis can also be manifested as multiple nodules with clear boundaries, and there appears to be no significant difference in clinicopathological features between LPD patients with or without endometriosis.[23] When LPD lesions occur in the stomach, distinguishing them from peritoneal dissemination due to GIST can be challenging due to overlapping imaging characteristics between GIST and LPD. Consequently, pre-operative diagnosis remains complex and depends on pathological evaluation and immunohistochemistry.
In general, LPD mainly needs to be distinguished from the following diseases: (1) Peritoneal metastases: gastric cancer and ovarian cancer metastasize to the peritoneum via hematogenous routes, lymphatic pathways, local infiltration, or implantation. This results in multiple nodules within the omentum and mesentery that exhibit indistinct margins, irregular shapes, heterogeneous signal intensities, and asynchronous enhancement relative to the myometrium. Malignant signs such as massive abdominal and pelvic effusion and peripheral lymph node enlargement may also be present. Conversely, LPD lesions typically display smooth and well-defined edges, rarely fused into a mass, and the surrounding adipose tissue remains clear of any “omental cake” sign. (2) Primary peritoneal leiomyosarcoma: It is a prevalent soft tissue sarcoma found in the retroperitoneum, usually located in the upper abdomen, near the root of the mesentery or the vicinity of the retroperitoneum, and manifests as a large lobulated mass often associated with necrosis and cystic degeneration. Histologically, sarcomatous cells are poorly differentiated with a high mitotic index—a stark contrast to LPD.[8] MRI features include marginal irregularity, slightly low signal intensity on T1WI, high signal intensity on T2WI and DWI, uneven enhancement of solid components post-contrast administration, alongside malignant features such as invasion into adjacent structures or distant metastasis.[24] Typically, LPD presents with low signal intensity similar to smooth muscle on T2WI, and malignant signs such as adjacent vascular invasion and abdominal fluid accumulation are rare. (3) GISTs: presented as circular nodules or masses, prone to cystic necrosis, they generally show mildly hypointense on T1WI while exhibiting mixed high signal intensity on T2WI, and significantly enhanced post-contrast. Peritoneal implants resulting from gastrointestinal malignancies generally do not involve muscle layer, while both muscle layer and peritoneal lesions can often be observed simultaneously in LPD patients.[3]
There are a number of typical imaging features of LPD, and it is important for the reporting radiologist to have a broad understanding of them. But it is worth noting that histopathological assessment remains the critical standard for determining LPD diagnosis. We summarized the image features of LPD to offer diagnostic references and differential thoughts for radiologists, especially primary physicians, and decrease the rate of preoperative misdiagnosis.
CONCLUSION
LPD is a rare benign multifocal lesion located in the abdomen and pelvis, with certain characteristic CT and MRI findings, and most patients have a prior history of hysteromyoma surgery. Integrating imaging findings with clinical history is helpful to enhance the accuracy of preoperative diagnosis.
Ethical approval
The research/study was approved by the Institutional Review Board at the Ethics Review Board of The First Affiliated Hospital of Soochow University, number 2024538, dated October 22, 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
1. Jiangsu Province Capability Improvement Project through Science, Technology and Education (Jiangsu Provincial Medical Key Discipline Cultivation Unit, JSDW202242) 2. Suzhou Key Laboratory of Medical Imaging (SZS2024032).
References
- Multiple peritoneal leiomyomas associated with a granulosa-cell tumor of the ovary. Am J Obstet Gynecol. 1952;64:204-8.
- [CrossRef] [PubMed] [Google Scholar]
- Leiomyomatosis peritonealis disseminata; an unusual complication of genital leiomyomata. Obstet Gynecol. 1965;25:561-74.
- [Google Scholar]
- Magnetic resonance imaging findings of leiomyomatosis peritonealis disseminata: A case description and literature analysis. Quant Imaging Med Surg. 2023;13:4015-9.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated peritoneal leiomyoma: A diagnostic dilemma. BMJ Case Rep. 2024;17:e259093.
- [CrossRef] [PubMed] [Google Scholar]
- Parasitic myoma after laparoscopic morcellation: A systematic review of the literature. BJOG. 2016;123:69-75.
- [CrossRef] [PubMed] [Google Scholar]
- Leiomyomatosis peritonealis disseminata of unusual course with malignant transformation: Case report. Acta Obstet Gynecol Scand. 2015;94:220-3.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated peritoneal leiomyomatosis after laparoscopic supracervical hysterectomy with characteristic molecular cytogenetic findings of uterine leiomyoma. Genes Chromosomes Cancer. 2010;49:1152-60.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated peritoneal leiomyomatosis: A case report and review of the literature. J Int Med Res. 2021;49:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Successful pregnancy after complete resection of leiomyomatosis peritonealis disseminate without recurrence: A case report with next-generation sequencing analysis and literature review. World J Surg Oncol. 2020;18:85.
- [CrossRef] [PubMed] [Google Scholar]
- Laparoscopic management of disseminated peritoneal leiomyomatosis. J Minim Invasive Gynecol. 2023;30:443-4.
- [CrossRef] [PubMed] [Google Scholar]
- Ulipristal acetate for disseminated peritoneal leiomyomatosis. Obstet Gynecol. 2019;133:434-6.
- [CrossRef] [PubMed] [Google Scholar]
- Leiomyomatosis peritonealis disseminata: Three case reports. Medicine (Baltimore). 2020;99:e22633.
- [CrossRef] [PubMed] [Google Scholar]
- A case of disseminated peritoneal leiomyomatosis after two laparoscopic procedures due to uterine fibroids. Wideochir Inne Tech Maloinwazyjne. 2017;12:110-4.
- [CrossRef] [PubMed] [Google Scholar]
- Combination therapy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for recurrent leiomyomatosis peritonealis disseminata with endometriosis: A case report. Heliyon. 2023;9:e19794.
- [CrossRef] [PubMed] [Google Scholar]
- A diagnostic dilemma of recurrent disseminated peritoneal leiomyomatosis with hypertrophied omental vessels: Imaging and embolization of omental branches with positive outcome. Case Rep Obstet Gynecol. 2017;2017:8427240.
- [CrossRef] [PubMed] [Google Scholar]
- Leiomyomatosis peritonealis disseminata with low-grade malignant change: A case report. Medicine (Baltimore). 2022;101:e30528.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging manifestations and diagnosis of disseminated peritoneal leiomyomatosis. J Clin Radiol. 2022;41:1065-70.
- [Google Scholar]
- Preoperative differentiation of uterine leiomyomas and leiomyosarcomas: Current possibilities and future directions. Cancers (Basel). 2022;14:1966.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated peritoneal leiomyomatosis presenting as liver mass. Clin Gastroenterol Hepatol. 2024;22:A13-4.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated peritoneal leiomyomatosis with endometriosis. J Minim Invasive Gynecol. 2012;19:380-2.
- [CrossRef] [PubMed] [Google Scholar]
- Leyomiomatosis peritonealis disseminata associated with ovarian endometriosis in a patient submitted to hysteroscopic myomectomy [published correction appears in Fertil Steril. . 2019;112:401.
- [CrossRef] [PubMed] [Google Scholar]
- Gastrointestinal stromal tumor coexisting with disseminated peritoneal leiomyomatosis. Surg Case Rep. 2019;5:130.
- [CrossRef] [PubMed] [Google Scholar]
- Leiomyomatosis peritonealis disseminata coexisting with endometriosis within the same lesions: A case report with review of the literature. Int J Clin Exp Pathol. 2013;6:2949-54.
- [Google Scholar]
- Recurrent leiomyomatosis peritonealis disseminata. Int J Gynecol Cancer. 2023;33:827-32.
- [CrossRef] [PubMed] [Google Scholar]







