Translate this page into:
Comparison of periprocedural and procedure room times between moderate sedation and monitored anesthesia care in interventional radiology

*Corresponding author: Vlasios S. Sotirchos, Interventional Radiology Service, Memorial Sloan Kettering Cancer Center, New York, United States. sotirchv@mskcc.org
-
Received: ,
Accepted: ,
How to cite this article: Sotirchos VS, Alexander ES, Zhao K, Zhan C, Yarmohammadi H, Ziv E, et al. Comparison of periprocedural and procedure room times between moderate sedation and monitored anesthesia care in interventional radiology. J Clin Imaging Sci. 2024;14:11. doi: 10.25259/JCIS_9_2024
Abstract
Objectives:
In recent years, there has been increased utilization of monitored anesthesia care (MAC) in interventional radiology (IR) departments. The purpose of this study was to compare pre-procedure bed, procedure room, and post-procedure bed times for IR procedures performed with either nurse-administered moderate sedation (MOSED) or MAC.
Material and Methods:
An institutional review board-approved single institution retrospective review of IR procedures between January 2010 and September 2022 was performed. Procedures performed with general anesthesia or local anesthetic only, missing time stamps, or where <50 cases were performed for both MAC and MOSED were excluded from the study. Pre-procedure bed, procedure room, post-procedure bed, and total IR encounter times were compared between MAC and MOSED using the t-test. The effect size was estimated using Cohen’s d statistic.
Results:
97,480 cases spanning 69 procedure codes were examined. Mean time in pre-procedure bed was 27 min longer for MAC procedures (69 vs. 42 min, P < 0.001, d = 0.95). Mean procedure room time was 11 min shorter for MAC (60 vs. 71 min, P < 0.001, d = 0.48), and mean time in post-procedure bed was 10 min longer for MAC (102 vs. 92 min, P < 0.001, d = 0.22). Total IR encounter times were on average 27 min longer for MAC cases (231 vs. 204 min, P < 0.001, d = 0.41).
Conclusion:
MAC improves the utilization of IR procedure rooms, but at the cost of increased patient time in the pre- and post-procedure areas.
Keywords
Moderate sedation
Interventional radiology workflow
Monitored anesthesia care
Procedure room utilization
Post-procedure recovery
INTRODUCTION
Most interventional radiology (IR) procedures are performed under moderate sedation (MOSED).[1-3] An IR registered nurse, typically with prior intensive care unit or emergency department experience, provides sedation under the supervision of the IR physician performing the procedure. Medications administered to achieve MOSED during the procedure are usually midazolam and fentanyl, for anxiolysis and analgesia, respectively.
In recent years, there has been increased utilization of monitored anesthesia care (MAC) in IR departments. This is a result of IR physicians performing increasingly complex procedures on patients who are progressively sicker and have multiple coexisting health conditions, necessitating the attainment of deeper levels of sedation during these interventions.[4,5] For patients undergoing procedures under MAC, a physician anesthesiologist performs a pre-procedure assessment and is subsequently present in the procedure room or oversees a certified registered nurse anesthetist during the procedure.
The impact of MAC on IR procedure workflow, room times, and patient throughput in IR departments remains unknown. The purpose of this study was to compare pre-procedure bed, procedure room, post-procedure bed, and total IR encounter times for procedures performed with either MOSED or MAC.
MATERIAL AND METHODS
Study setting, design, and data collection
An Institutional Research Board-approved retrospective review of IR procedures at a single academic institution between January 2010 and September 2022 was performed. Procedures and scheduling times for cases performed with MOSED and MAC were extracted from the Epic OpTime module (Verona, WI).
Procedures performed with general anesthesia or local anesthetic only, missing time stamps, or those infrequently performed (<50 cases for both MAC and MOSED) were excluded from the study. Procedures performed at regional outpatient centers within the institution were also excluded from the study. Pre-procedure time (time in pre-procedure bed), procedure room time (time in IR procedure room), post-procedure time (time in recovery/post-anesthesia care unit - bed), and total IR encounter time (pre-procedure bed + procedure room + post-procedure bed times) were recorded [Figure 1].
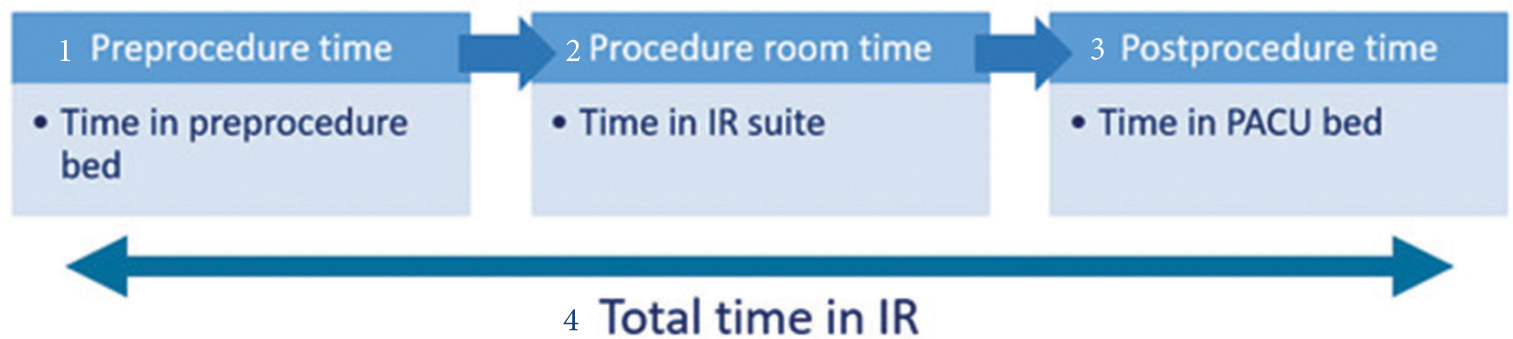
- Diagram showing the times compared overall and for each procedure code; (1) pre-procedure bed time, (2) procedure room time, (3) post-procedure bed time, and (4) total time in interventional radiology (total encounter time). (IR: Interventional radiology. PACU: Post anesthesia care unit).
Statistical analysis
Mean times for each procedure code and for all procedures were compared between MAC and MOSED cases using the t-test (significance P < 0.05). Given the large sample size which can overestimate significance, the effect size was estimated using Cohen’s d statistic (mean difference/pooled standard deviation); large effects were defined as d > 0.8, moderate 0.5–0.8, and small <0.5. R software version 4.0.2 was used for all statistical analysis (R Core Team, 2020, R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Study cohort
A total of 200,319 procedures were performed during the study period. After applying the exclusion criteria, 97,480 cases spanning 69 procedure codes were examined. The most frequently performed procedures were chest port placement (16%), lung biopsy (12%), liver biopsy (6%), abdomen biopsy (5%), and chest port removal (4%).
Time in pre-procedure bed
Mean time in pre-procedure bed was significantly higher for MAC across all examined procedure codes [Figure 2]. Overall, the difference was 27 min with a large effect size (69 vs. 42 min, P < 0.001, d = 0.95). The mean times in pre-procedure bed for the most commonly performed procedures were as follows: Chest port placement (68 vs. 41 min), lung biopsy (76 vs. 45 min), liver biopsy (70 vs. 43 min), abdomen biopsy (69 vs. 41 min), and chest port removal (63 vs. 39 min), all P < 0.001 [Figure 3].

- Comparison of mean times for moderate sedation (MOSED) and monitored anesthesia care (MAC) at each stage for all interventional radiology (IR) procedures. d = Cohen’s statistic, effect size in parentheses at each stage of the interventional radiology encounter. All time differences between MOSED and MAC were statistically significant (P < 0.001).

- Differences of mean times between moderate sedation (MOSED) and monitored anesthesia care (MAC) at each stage of the interventional radiology (IR) encounter, for the five most frequently performed procedures. The mean total time in IR was shorter for procedures performed with MOSED. All time differences between MOSED and MAC were statistically significant (P < 0.001).
Procedure room time
Overall, procedures performed with MAC were associated with a small decrease in mean procedure room time compared to MOSED (−11 min, 60 vs. 71, P < 0.001, d = 0.48). Procedure room time was decreased with MAC across all examined procedure codes.
Time in post-procedure bed
Overall, there was a small increase in mean time in post-procedure bed (10 min, 102 vs. 92 min, P < 0.001, d = 0.22) for MAC compared to MOSED. Only 7/69 procedure codes were associated with increased mean MOSED times in post-procedure bed (bone biopsy, spine biopsy, abscess catheter check, hepatic transarterial embolization, magnetic resonance-guided soft-tissue biopsy, limited imaging in IR suite without intervention, and transjugular liver biopsy). All other procedure codes were associated with decreased post-procedure bed time with MOSED.
Total IR encounter time
Overall, the mean total IR encounter time (pre-procedure bed + procedure room + post-procedure bed times) was 27 min longer for MAC cases than MOSED cases (231 vs. 204 min, P < 0.001, d = 0.42). The largest time differences were observed for biliary catheter to stent conversions (282 vs. 241 min), nephroureterostomy tube placements (266 vs. 230 min), and inferior vena cava filter removals (214 vs. 179 min), all P < 0.001 [Figure 4].

- Procedures with the largest differences in mean total interventional radiology encounter times (shaded in grey) between moderate sedation (MOSED) and monitored anesthesia care (MAC). All time differences between MOSED and MAC were statistically significant (P < 0.001) (IVC: Inferior vena cava).
DISCUSSION
This study was performed at a tertiary academic center specializing in cancer care. Depending on the patient’s condition/comorbidities/preference, the planned procedure, and procedure room availability, outpatient and inpatient cases are scheduled in a MOSED or anesthesia-staffed procedure room. During the study period, the number of IR procedure rooms and IR-dedicated anesthesia teams varied; however, the most common setup over the examined time frame was 7 procedure rooms, with 4 staffed by anesthesiology. Today, the number of procedure rooms is 12, with 9 staffed by anesthesiology and 3 by IR nurses administering MOSED. This excludes the institution’s three regional outpatient centers, which each have one IR procedure room with a dedicated anesthesia team for the performance of routine IR procedures. As the workflow at the regional outpatient centers providing ambulatory care is significantly different compared to the hospital setting, the procedures performed at these centers were excluded from the study.
Although all time differences in this study were statistically significant, the largest effect size was a pronounced difference between MAC and MOSED for pre-procedure bed times, with significantly increased times for MAC. A contributing factor could be the additional pre-procedure evaluation and informed consent required by a physician anesthesiologist. Moreover, patients with severe comorbidities and inpatients were preferentially scheduled with MAC, leading to longer times for appropriate patient workup before transfer to the procedure room.
Once in the procedure room, MAC procedure room time was shorter than MOSED by an average of 11 min overall. With the presence of an anesthesia provider in the procedure room, IR physicians can focus on the technical aspects of the procedure as opposed to MOSED procedures where they are also responsible for sedation administration by the IR nurse. More medication options are available with MAC to achieve deeper patient sedation (e.g., propofol, dexmedetomidine, and ketamine) and minimize patient movement and discomfort, likely contributing to decreased procedure times. The effects of these medications and deeper procedural sedation may be responsible for the longer recovery/post-procedure bed times observed with MAC, by an average of 10 min.
Over the past two decades, there has been a trend of increased utilization of MAC in IR[4,5] and other specialties.[6] This study shows that there are time-saving benefits in retaining nurse-administered MOSED in IR. In our experience, there are additional advantages to maintaining MOSED in IR. With MOSED, there is more flexibility in scheduling urgent procedures off hours, since IR is not dependent on another service (Anesthesiology) which may have to staff other urgent interventions (e.g., surgical and endoscopic) in the hospital. In addition, an IR department offering MOSED is more likely to retain more experienced and skilled nurses, as the administration of MOSED requires added qualifications and credentials. Finally, there are cost-saving benefits with MOSED (Current Procedural Terminology [CPT] codes 99151–99153 and 99155–99157) compared to MAC for IR procedures (CPT codes 01916–01933), with the latter requiring an additional physician consult and the presence of an anesthesia provider in the procedure room.[7]
The results of this study may be helpful for IR departments seeking to increase procedure volume. If there is a fixed number of procedure rooms without the capability for expansion, utilization of MAC may lead to increased procedure room turnover; however, a need for more pre- and post-procedure area beds may arise. Given the different advantage profiles of MOSED and MAC, larger IR departments can designate procedure rooms for MOSED and for anesthesia, to maximize the benefits of the IR service.
There are several limitations in this study, which was performed at a single academic institution specializing in cancer care; therefore, the results may not be applicable to other institutions. The patient population in this study had a high prevalence of chronic pain and opioid tolerance, which may have led to instances of suboptimal sedation with MOSED and increased procedure room times. Selection bias was likely present, since patients with comorbidities and inpatients were preferentially scheduled with MAC. Patient satisfaction was not examined in this study, however there are studies showing improved patient satisfaction with MAC for non-surgical procedures.[8]
CONCLUSION
MAC improves the utilization of IR procedure rooms, but at the cost of increased patient time in the pre- and post-procedure areas.
Ethical approval
The research/study was approved by the Institutional Review Board at MSKCC, number 16-402, dated 5/3/2016.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Memorial Sloan Kettering Cancer Center is supported by the NIH/NCI Cancer Center Support Grant P30 CA008748.
References
- Sedation and analgesia in interventional radiology: Where do we stand, where are we heading and why does it matter? Diagn Interv Imaging. 2019;100:753-62.
- [CrossRef] [PubMed] [Google Scholar]
- ACR-SIR practice parameter for minimal and/or moderate sedation/analgesia. Available from: https://www.acr.org/-/media/ACR/files/practice-parameters/sed-analgesia [Last accessed on 2024 Jan 20]
- [Google Scholar]
- Moderate sedation: What radiologists need to know. AJR Am J Roentgenol. 2013;201:941-6.
- [CrossRef] [PubMed] [Google Scholar]
- The future of anesthesia for interventional radiology. Curr Opin Anaesthesiol. 2018;31:469-72.
- [CrossRef] [PubMed] [Google Scholar]
- Common procedures and strategies for anaesthesia in interventional radiology. Curr Opin Anaesthesiol. 2015;28:458-63.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review of factors associated with utilization of monitored anesthesia care for gastrointestinal endoscopy. Gastroenterol Hepatol (N Y). 2016;12:361-70.
- [Google Scholar]
- Impact of moderate sedation versus monitored anesthesia care on outcomes and cost of endobronchial ultrasound transbronchial needle aspiration. Pulm Med. 2019;2019:4347852.
- [CrossRef] [PubMed] [Google Scholar]
- Patient satisfaction with deep versus light/moderate sedation for non-surgical procedures: A systematic review and meta-analysis. Medicine (Baltimore). 2021;100:e27176.
- [CrossRef] [PubMed] [Google Scholar]






