Translate this page into:
Bronchial Artery Aneurysm with Associated Bronchial Artery to Pulmonary Artery Fistula: Treatment by Embolization
Address for correspondence: Dr. Nader Kamangar, Department of Internal Medicine, Division of Pulmonary Medicine and Critical Care, UCLA Medical Center, David Geffen School of Medicine, Sylmar, CA 91342, USA. E-mail: kamangar@ucla.edu
-
Received: ,
Accepted: ,
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Bronchial artery aneurysm (BAA) is a rare vascular phenomenon. This review highlights a case of a BAA that was complicated by the presence of a bronchial artery to pulmonary artery (BA-PA) fistula, consequently presenting a unique challenge to management. BAAs have a strongly reported risk of rupture resulting in life-threatening hemoptysis. Embolization has thus become routine for the management such severe cases. The management of incidentally found anomalies is less obvious, but prophylactic embolization is a generally accepted practice. In this report, we review some of the risks and benefits associated with BAA embolization with specific consideration of the challenges in cases of co-existing BA-PA fistula.
Keywords
Bronchial artery aneurysm
bronchial artery to pulmonary artery fistula
pulmonary arteriovenous malformation

Introduction
Bronchial artery aneurysm (BAA) is seen in less than 1% of cases of selective bronchial arteriography. It is a potentially life-threatening condition, often requiring immediate therapy following diagnosis. Most patients are asymptomatic, however, massive hemoptysis and mediastinal hematomas are potentially devastating complications following their rupture. Although no direct etiology has been established, most cases of BAA are associated chronic inflammatory, infectious and vascular lung diseases. Bronchial artery to pulmonary artery (BA-PA) fistula is an exceedingly uncommon vascular anomaly which can be congenital or acquired.[12]
We herein report of a case of patient who presented with progressive dyspnea, found to have a BAA with associated BA-PA fistula. The patient was successfully treated with embolization using cyanoacrylate. She was noted to have improvement of symptoms on follow-up.
Case Report
A 63 year-old female with hypothyroidism and no history of hereditary hemorrhagic telangiectasia (HHT) or pulmonary disease presented with gradually progressive dyspnea on exertion over a course of 3 years, with subacute worsening over a period of 2 weeks significantly affecting ability to perform her activities of daily living. She had no chest pain, back pain, recent illnesses, cough, or B symptoms. She had no history of smoking. Additional history was unremarkable. Physical examination was only notable for oxygen saturation of 95% at rest with mild, 7%–8%, desaturation after minimal exertion. Initial pulmonary function testing and echocardiogram with agitated saline were unremarkable.
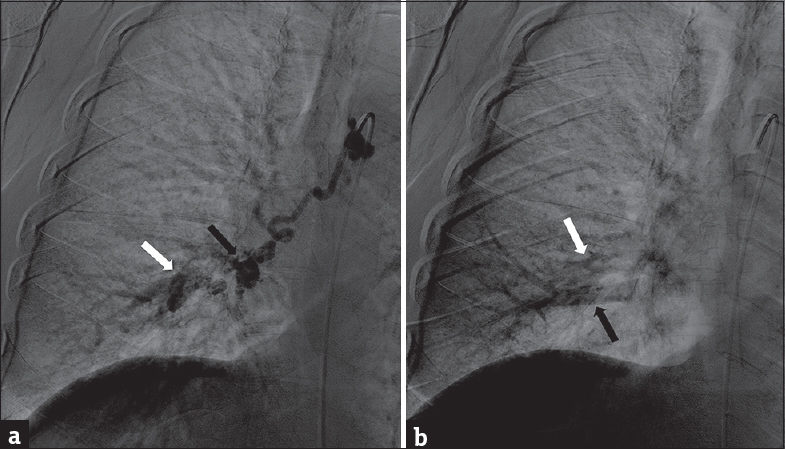
A computed tomography (CT) pulmonary angiogram was significant for a single 1.2 cm right infrahilar nonspecific density that was suspicious for an arterial source [Figure 1a]. Therefore, a CT arteriogram was performed that revealed an intrapulmonary BAA [Figure 1b]. Bronchial artery angiography was then performed, further demonstrating the presence of a BAA with BA-PA fistula [Figure 2a and b].

- A 63-year-old woman without significant medical history who presented with subacute onset of dyspnea on exertion. (a) Computed tomography pulmonary angiogram highlights the pulmonary arteries; there is a note of a nonspecific infrahilar mass (white arrow). (b) Repeat computed tomography arteriogram allows tracing of bronchial artery (black arrows). Previously noted infrahilar mass is highlighted suggesting bronchial artery aneurysm.
- A 63-year-old woman without significant medical history who presented with subacute onset of dyspnea on exertion. (a) Bronchial artery angiogram with contrast injected directly into the bronchial artery under video fluoroscopy shows contrast filling of the bronchial artery aneurysm (black arrow) and simultaneous filling of the pulmonary artery (white arrow). On video fluoroscopy, contrast was noted to flow outward toward the lung periphery. (b) Bronchial artery angiogram after slight time delay shows contrast fading from pulmonary artery (white arrow) and flowing inward toward the hila through pulmonary vein (black arrow). This was, therefore, consistent with bronchial artery to pulmonary artery fistula rather than bronchial artery to pulmonary artery fistula.
The patient underwent successful embolization of with cyanoacrylate [Figure 3]. On 3-month follow-up evaluation, the patient noted that symptoms had ceased progressing and that she was no longer experiencing significant shortness of breath. During her 1-year postembolization follow-up, the patient remained stable with improvement of her dyspnea, and CT angiogram confirming durable bronchial artery occlusion without notable expansion of the BAA [Figure 4].
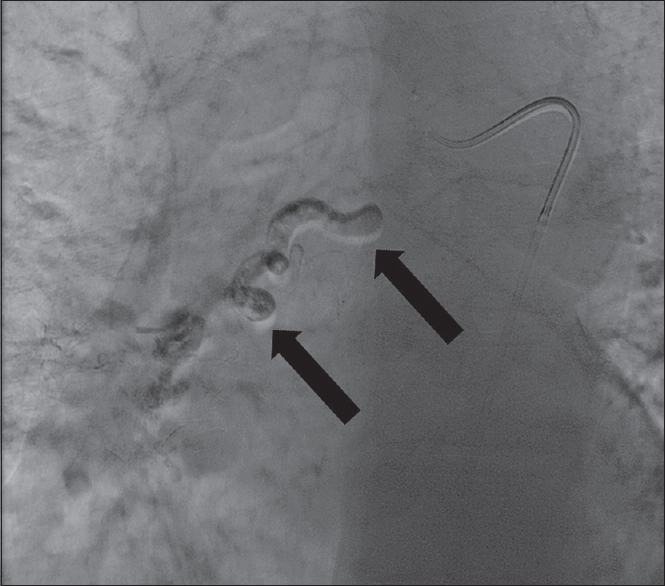
- A 63-year-old woman without significant medical history who presented with subacute onset of dyspnea on exertion. Successful postembolization bronchial artery angiogram shows cyanoacrylate glue outlining and occluding the distal bronchial artery (black arrow).
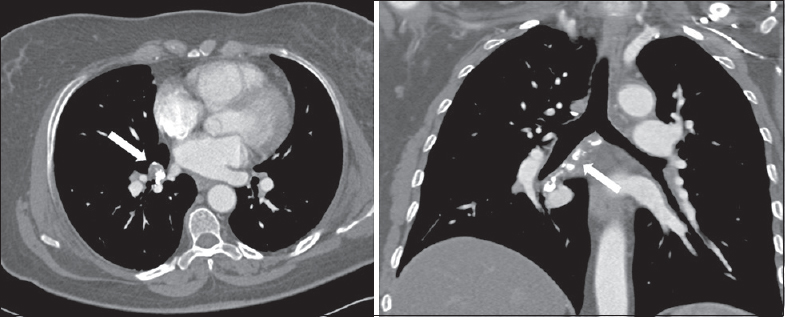
- A 63-year-old woman without significant medical history who presented with subacute onset of dyspnea on exertion. One-year status-postembolization follow-up, computed tomography angiogram confirming durable bronchial artery occlusion (white arrows) without notable expansion of bronchial artery aneurysm.
Discussion
BAA is a rare phenomenon, and concomitant BA-PA fistula is even more uncommon. In one review of 13 cases of BAA, sizes of BAA ranged from 5 to 30 mm,[3] however, the size was not felt to be predictive of risk of rupture. Many BAAs remain asymptomatic until rupture. Because of the inherent instability and risk of rupture, current recommendations are that BAAs should be treated on identification.[4] Embolization is the treatment of choice, however, it is not without inherent risks.
Although suggestive of possible BAA, the initial CT pulmonary angiogram was suboptimal for BAA characterization. In addition, there was no evidence to suggest a pulmonary vascular fistula. However, on the CT arteriogram, the BAA was more clearly identified, but the fistula was not. Additionally, certain images may have misleadingly suggested bronchial artery to pulmonary vein (BA-PV) fistula [Figure 1b]. In systemic-to-pulmonary vascular malformations, anomalous flow causes abnormal filling patterns on angiography which may result in misdiagnoses.[1] Thus, selective bronchial artery angiogram is preferable when such pathology is suspected. In this case, identification of a BA-PA fistula via selective angiography was important considering that the risks of embolization of isolated BAA versus BA-PA and/or BA-PV fistula may theoretically be different.
It is unclear if the risk of rupture of BAA with BA to pulmonary circulation fistula differs from BAA alone, as their description remains limited to case reports. When identified, such systemic-to-pulmonary arteriovenous malformations (AVM) can be congenital or acquired.[5] If acquired, they are most often associated with underlying pulmonary diseases such as bronchiectasis, tuberculosis, or other inflammatory disease.[1] Some have suggested that hypoxia itself can be a catalyst in angiogenesis of anomalous collaterals.[6] If BAA formation is indeed secondary to high-pressure gradients, and if rupture is the result of necessary release of tension, it would seem plausible that fistula formation could also have relieved tension and reduced risk of rupture. In this case, it remained unclear if BAA with fistula was the cause of her shortness of breath or a symptom of her underlying disease.
Had this been a BA-PV fistula, embolization would have presented the theoretical risk of inadvertent propagation of emboli to the systemic circulation. Inadvertent migration of embolized material is reported in up to 3% of bronchial artery embolization (BAE) cases, and air emboli in approximately 2% of cases.[78] Bronchial artery embolization by itself presents the risk of inadvertent spinal artery embolization, with some original studies reporting a incidence of up to 6.5 percent. Ultimately, when weighed against the risks and consequences of rupture, and compounded by that lack of alternative explanations for the patient's shortness of breath, the decision was made to proceed with embolization.
Finally, there are an increasing number of options and techniques for embolization.[9] The choice of the embolic agent should be dependent on durability of occlusion, size of occluded vessel, and ease of delivery.[10] It has been suggested that coils be avoided as they frequently require proximal placement which may preclude future embolization.[11] In cases of BAE for management of hemoptysis, recurrence rates range from 10% to 55% after as long as 46 months.[10] Therefore, follow-up imaging may often be indicated to verify durable occlusion.
Conclusions
While embolization of BAA is widely accepted as the treatment of choice, BAA complicated by fistulation to the pulmonary circulation resulting in a systemic-to-pulmonary AVM represents an uncommon challenge to management. CT angiogram alone may be insufficient for identification of a fistulous tract therefore, selective bronchial artery angiogram is recommended. Finally, a multidisciplinary discussion is instrumental in selecting the optimal therpeutic modality, followed by a thorough review of its risks, alternatives, and benefits with the patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2017/7/1/2/199052.
References
- Congenital and acquired pulmonary artery anomalies in the adult: Radiologic overview. Radiographics. 2006;26:349-71.
- [Google Scholar]
- A case of bronchial artery aneurysm demonstrating a mass shadow on chest x-ray film. Nihon Kyobu Shikkan Gakkai Zasshi. 1991;29:1591-5.
- [Google Scholar]
- Mediastinal fibrosis complicating healed primary histoplasmosis and tuberculosis. Medicine (Baltimore). 1972;51:227-46.
- [Google Scholar]
- Giant mediastinal bronchial artery aneurysm mimicking benign esophageal tumor: A case report and review of 26 cases from literature. J Vasc Surg. 2003;38:1125-9.
- [Google Scholar]
- Cavernous hemangioma of the bronchial wall: A systemic-pulmonary vessel fistula. J Thorac Cardiovasc Surg. 2009;137:1272-3.
- [Google Scholar]
- Systemic-to-pulmonary collaterals in pathological states: A review. Radiology. 1982;144:55-9.
- [Google Scholar]
- Bronchial and nonbronchial systemic artery embolization for life-threatening hemoptysis: A comprehensive review. Radiographics. 2002;22:1395-409.
- [Google Scholar]
- Bronchial artery embolization for hemoptysis. Semin Intervent Radiol. 2011;28:48-62.
- [Google Scholar]
- Bronchial artery embolization for hemoptysis. Semin Intervent Radiol. 2008;25:310-8.
- [Google Scholar]






