Translate this page into:
Bilateral Multiple Level Lateral Meningocoele
Address for correspondence: Dr. B. E. Panil Kumar, Department of Radio-Diagnosis, Narayana Medical College Hospital, Chinthareddypalem, Nellore, Andhra Pradesh, India. E-mail: panilkumarbe@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Lateral meningocoele is a very rare disorder characterized by extensions of the dura and arachnoid through an enlarged neural foramen. We report a case of a 23-year-old female with deformity of spine who presented with low back pain and no neurological deficits. A whole spine magnetic resonance imaging showed multiple well-defined cystic masses involving dorsal, lumbar, and sacral spinal levels bilaterally, with dural ectasia and neural foraminal widening suggestive of bilateral multiple level lateral meningocoele. The patient is being managed conservatively and is on regular follow-up.
Keywords
Lateral meningocele
multiple menigocoele
spinal dysraphism
INTRODUCTION

Lateral meningocele is a rare presentation of spinal dysraphism characterized by extensions of the dura and arachnoid through an enlarged neural foramen.[1–10] In the present report, we discuss a case of a 23-year-old female who had bilateral multiple level lateral meningocoele with no neurological deficits and without any associated craniofacial anomalies, neurofibromatosis, or Marfan's syndrome.
CASE REPORT
A 23-year-old female patient presented with 6-month history of low back pain and associated spine deformity. On neurological examination higher mental functions, cranial nerves, motor, and sensory systems were normal. There were no focal neurological deficits. Bowel and bladder functions were normal. Her spinal column appeared kyphotic. Patient stature is normal without any skin lesions. No features of either Marfan's syndrome or Neurofibromatosis Type I were noted. Routine laboratory investigations including hemoglobin (10.6 g%) and routine urine microscopy were within normal limits. A whole spine magnetic resonance imaging (MRI) showed well-defined multiple cystic masses involving dorsal, lumbar, and sacral spinal levels. These multiple cystic lesions are hypointense on T1-weighted images and hyperintense on T2-weighted images, which is similar to cerebrospinal fluid (CSF) signals. In addition, there was dural ectasia and neural foraminal widening [Figures 1 and 2]. There was low-lying position of the cord but roots were unremarkable. The findings were suggestive of multiple level lateral meningocoele. The patient was managed with analgesics and regular physiotherapy and is under regular follow-up and observation.
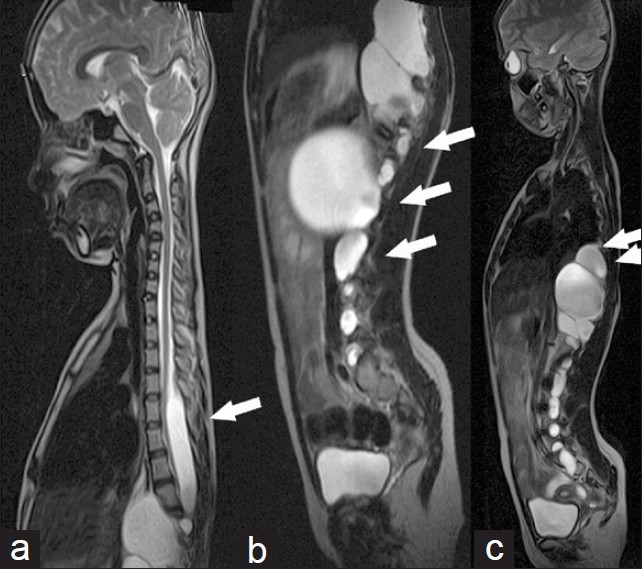
- Serial sagittal magnetic resonance imaging T2W images of dorso-lumbo-sacral spine. (a) Right parasagittal section. (b) Sagittal section and (c) Left parasagittal section show multiple level and extensive lateral meningocoele with neural foraminal widening (arrow) and dural ectasia (arrow).
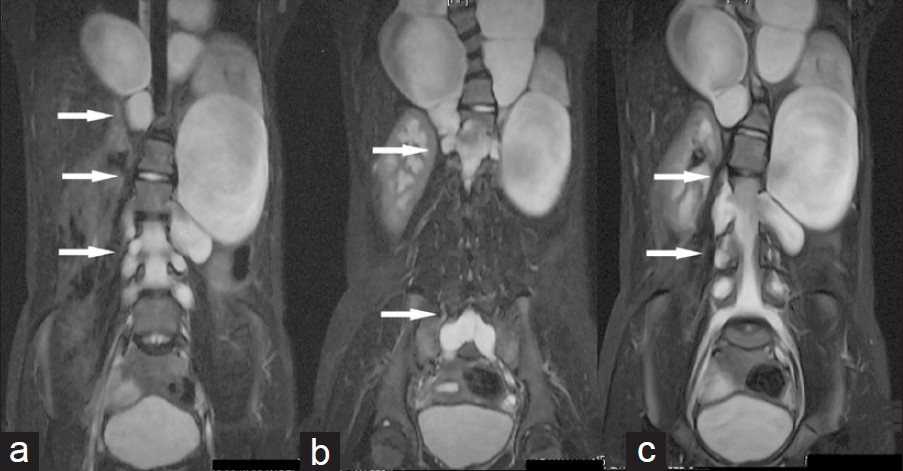
- Serial coronal magnetic resonance imaging STIR images (a, b, c) of dorso-lumbo-sacral spine show multiple level and extensive lateral meningocoele with neural foraminal widening (arrow), dural ectasia (arrow) and scoliosis deformity.
DISCUSSION
Lateral or anterior spinal meningocoeles are relatively rare congenital anomalies where protrusion of dura mater and arachnoid extending laterally through an enlarged intervertebral foramen into the paraspinal, intrathoracic, or retroperitoneal region.[11] Lateral meningocoeles may be unilateral or bilateral (as in the present case) or may be solitary or multiple. Typically, lateral and anterior meningocoeles are occult lesions that are not visible externally. An anterior defect can form in the vertebral column as a result of faulty embryogenesis. Such faulty development can also result in coexisting abnormalities in the skin, subcutaneous tissues, spine, and internal organs. Another important factor that can influence the development of anterior and lateral spinal meningoceles is the balance between both the hydrostatic pressure and the pulsations of the CSF, and the resistance of the arachnoid and dura mater to deformation by such pressure, especially at the intervertebral foramina. If there is a developmental bony defect, the dura and arachnoid may bulge out through it.
Lateral meningocele syndrome or Lehman syndrome, is characterized by multiple lateral meningoceles in the absence of Neurofibromatosis or Marfan's syndrome,[4] commonly present during the fourth and the fifth decades of life (in contrast to this, our patient was 23-years old)[1] and overall, female patients are more often affected than male patients. Lateral meningoceles commonly occur in thoracic and lumbar regions followed by the cervical area,[5–8] and rarely in the sacral region.[139] Because of this unique finding, Gripp[4] suggested the term “lateral meningocoele syndrome”. More and more patients with lateral meningocoele syndrome are being reported.[1] It is suggested that lateral menigocoele syndrome is an autosomal dominant disorder affecting primarily the connective tissue[4] with many associated skeletal findings kypho-scoliotic deformities, joint hypermobility, pectus deformities, craniofacial abnormalities, and vertebral defects such as hemivertebrae, scoliosis, absence of neural arches on the affected side, widening of the spinal canal, and intervertebral foramina. In our patient kypho-scoliosis is noted. The clinical manifestations of meningocoele closely relate with its size and its relationship with surrounding structures. The patient may be asymptomatic or can present with back pain or paraparesis.[12] In contrast, in the setting of a small meningocoele, no symptoms can be recorded, and the lesion may be incidentally diagnosed on a routine chest radiograph. It is widely accepted that excision of the lesion is indicated in the presence of progressive neurologic deficit, respiratory distress, or rapid progress in the size of the meningocoele.[1213]
On conventional radiographs, meningocoele appear as sharply defined round, smooth, or lobulated paraspinal masses. On computed tomography (CT) scan, these lesions appear as well-defined, homogeneous, low-attenuation paravertebral masses.[14] MRI findings are often diagnostic and better delineate the details of multiple lesions including paravertebral expansion and dural ectasias with scalloping of the pedicles, laminae, vertebral bodies, and an enlarged spinal canal.[110] Surgical excision is recommended for symptomatic lesions, particularly when there are neurological deficits or bowel and bladder involvement.[18] However, as our patient was not symptomatic for any of the lesions, she is being monitored during regular follow-ups.
CONCLUSION
Bilateral multiple level menigocoele without association with Neurofibromatosis or Marfan's syndrome is a rare entity. MRI best depicts the lesions. Surgeons and radiologists should be aware of this rare clinical entity. As the patient is asymptomatic, she is currently being managed conservatively.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/1/1/106613
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Lateral sacral meningocele presenting as a gluteal mass: A case report. J Med Case Rep. 2010;4:1-6.
- [Google Scholar]
- Multiple asymptomatic lateral thoracic meningocele. Eur J Cardiothorac Surg. 2008;33:113.
- [Google Scholar]
- Lateral meningocele syndrome: Three new patients and review of the literature. Am J Med Genet. 1997;70:229-39.
- [Google Scholar]
- Multiple anterolateral cervical meningoceles associated with neurofibromatosis. Neurosurg Rev. 1999;22:124-6.
- [Google Scholar]
- Lateral sacral meningomyelocele as a gluteal swelling: An unusual presentation. J Indian Med Assoc. 2005;103:556.
- [Google Scholar]
- Epithelioid hemangioendothelioma and multiple thoraco-lumbar lateral meningoceles: Two rare pathological entities in a patient with NF-1. Neuroradiology. 2005;47:165-9.
- [Google Scholar]
- Isolated true anterior thoracic meningocele. AJNR Am J Neuroradiol. 2004;25:1828-30.
- [Google Scholar]
- Intrathoracic giant meningocele developing hydrothorax: A case report. J Spinal Disord Tech. 2002;15:529-32.
- [Google Scholar]
- A neurofibromatosis type 1 patient with severe kyphoscoliosis and intrathoracic meningocele. J Clin Neurosci. 2003;10:268-72.
- [Google Scholar]
- Diseases of the mediastinum. In: Putman CE, Ravin CE, eds. Textbook of diagnostic imaging (2nd ed). Philadelphia, Pa: Saunders; 1994. p. :428-44.
- [Google Scholar]






