Translate this page into:
Agenesis of the Gallbladder with the Presence of a Small Dysmorphic Cyst: Role of Magnetic Resonance Cholangiopancreatography
Address for correspondence: Dr. Antonio Pierro, Radiology Department, Foundation for Research and Treatment, John Paul II, Largo A. Gemelli, 1 - 86100 Campobasso, Italy. E-mail: apierrojonico@libero.it
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
We report a case of agenesis of the gallbladder with the presence of a small dysmorphic cyst, along the bed of the gallbladder and cystic duct. The patient presented to us with a suspected diagnosis of atrophic and sclerotic gallbladder that was not seen on ultrasound examination, indicating the need for cholecystectomy. The patient's medical history report mentioned agenesis of the left kidney. The existence of a congenital abnormality led us to suspect the inability to visualize the gallbladder was probably due to a possible agenesis of the gallbladder. The patient was investigated with magnetic resonance cholangiopancreatography (MRCP), that confirmed the suspected diagnosis and avoided unnecessary surgery. The hypothesis of anomalous development or agenesis of the gallbladder should always be suspected when the gallbladder is not visible on ultrasound imaging, especially in patients with other congenital anomalies. We believe that in all these patients, MRCP must always be performed to help make decisions on the treatment protocol.
Keywords
Congenital abnormality
gallbladder agenesis
gallbladder scleroatrophic
MRCP
renal agenesis
INTRODUCTION

Developmental abnormalities of the gallbladder are relatively rare. Although more often asymptomatic, agenesis of the gallbladder can present with symptoms, such as dyspepsia, abdominal pain, nausea and vomiting, intolerance to fatty foods, and so on. It has been reported to be associated with gastrointestinal, cardiovascular, genitourinary, and skeletal malformations.
We report a case of a patient, with agenesis of the left kidney, who was a candidate for cholecystectomy for suspected sclerotic and atrophic gallbladder. Study with magnetic resonance cholangiopancreatography (MRCP) showed agenesis of the gallbladder with the presence of a small dysmorphic cyst, along the bed of the gallbladder and cystic duct, thus avoiding unnecessary surgery.
CASE REPORT
A 53-year-old woman presented to us with a history of dyspeptic syndrome and right upper quadrant abdominal pain. On ultrasound examination, performed in another institution, the gallbladder could not be seen. This raised a suspicion of gallbladder scleroatrophy with possible presence of microlithiasis. The laboratory tests carried out were all normal. The patient was advised to undergo cholecystectomy.
The clinical history of the patient showed the presence of a congenital anomaly - agenesis of the left kidney. In order to exclude the presence of any associated agenesis of the gallbladder, the patient was subjected to MRCP. This investigation showed agenesis of the gallbladder with the presence of a small dysmorphic cyst (longitudinal axis of 15 mm), along the bed of the gallbladder and cystic duct [Figures 1 and 2].
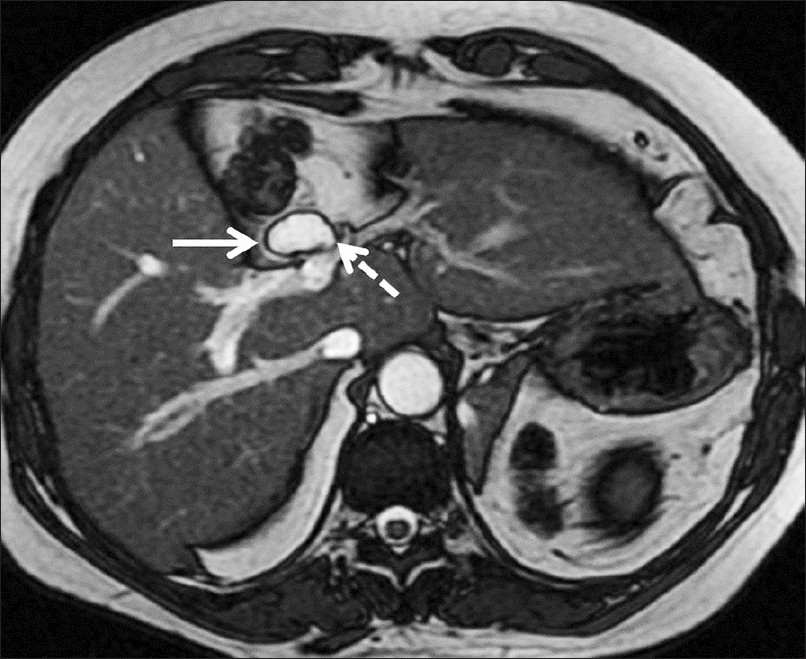
- Axial fast imaging employing steady-state acquisition image, shows a small cystic lesion (white arrow) along the course of the bed of the gallbladder, in proximity to the bile duct (dashed arrow).
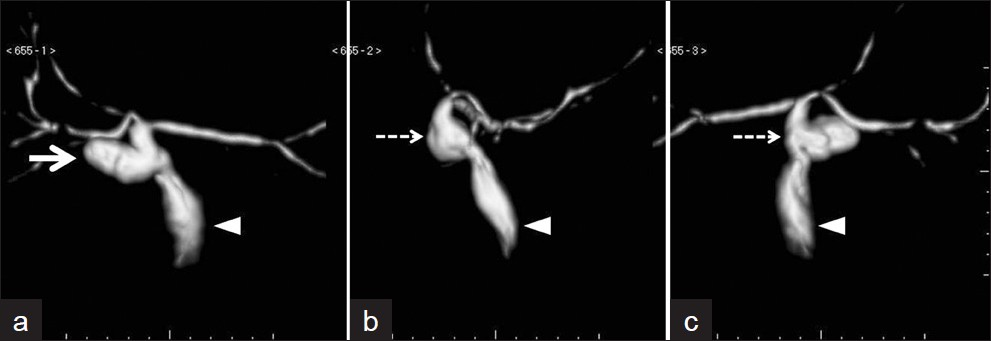
- Volume rendering technique images: (a) Front view; (b) lateral view; and (c) rear view show a small dysmorphic cystic dilatation (white arrow), which shows extensive communication with the bile duct (dashed arrow). The common bile duct is dilated (arrowhead), assuming the function of bile storage.
The virtual endoscopy images obtained with magnetic resonance imaging [Figure 3] show the extensive communication between the cystic dilatation of dysmorphic cystic duct and the common bile duct. The common bile duct shows a slight increase in size and there were no formations of gallstones in the bile ducts. Therefore, the patient was not subjected to surgery but started on medical therapy alone.
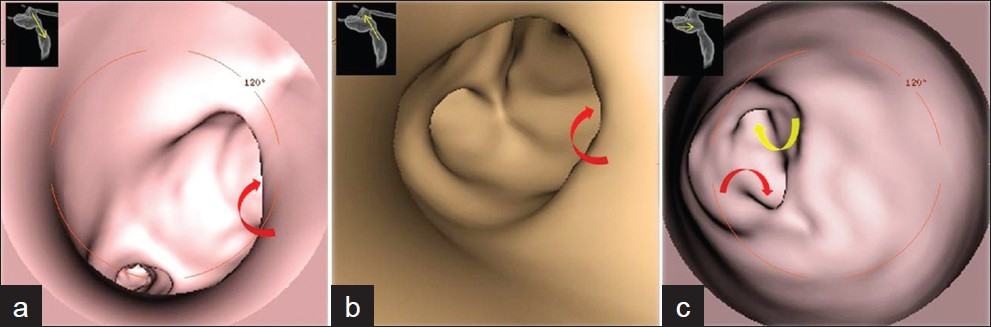
- Images of virtual endoscopy of the biliary tract. (a) Cranial endoscopic view, from the common hepatic duct into the common bile duct. We can appreciate the wide communication between the bile duct and cystic dilatation (red curved arrow). (b) Caudal view from the common bile duct into the common hepatic duct. Input cystic dilatation (curved arrow red). (c) View from the bottom of the cystic dilatation, into the common bile duct; you can well appreciate the openings, respectively, of the common hepatic duct (curved arrow yellow) and the common bile duct (arrow red curve).
We considered this cystic dilatation of the bile duct as the probable cystic ectasia of the dysmorphic cystic duct, because the point of origin from the common bile duct and the vector of growth along the bed of the gallbladder and cystic duct makes this hypothesis more likely. The absence of a collar and the elevated position, make it unlikely to be a diverticulum of the common bile duct (Todani Type II choledochal cyst).
DISCUSSION
In the 4th week of intrauterine life appears the hepatic diverticulum, an endodermal outpouching formed at the junction of the foregut and midgut. As the hepatic diverticulum grows, its connection with the gut narrows to form the extrahepatic bile duct. The hepatic diverticulum divides into 2 parts: A larger cranial part (pars hepatica), the primordium of the liver, and a smaller ventral part (pars cystica), the primordium of the gallbladder and of the cystic duct.
From the pars cystica, develop a vacuole and a shalk which respectively represent the gallbladder and the cystic duct. In a first stage, the gallbladder is a hollow organ, even if the proliferation of its epithelium determines a phase in which its cavity is temporarily canceled; subsequently, through the vacuolation of its epithelium, it again becomes a hollow organ.[12]
All the anomalies that alter the natural course of embryologic development can result in agenesis of the gallbladder alone or along with the absence of the cystic duct.
Gallbladder agenesis (GA) is a rare congenital anomaly characterized by the absence of the gallbladder in conjunction with a normal bile duct system.[3] It can be observed in both children and adults, with a median age of 46 years at the time of diagnosis.
It is almost always an incidental finding of the abdominal surgery or a finding at autopsy. It has a lower incidence in surgical cholecystectomy series (0.007%–0.027%) than that in autopsy reports (0.04%–0.13%). The prevalence range is 0.007%–0.13%.[4]
GA is usually accompanied by lack of the cystic duct, but it can be associated with patent and hypoplastic cystic duct according to different aberrations of the embryologic development. The lack of development of the pars cystica results in agenesis of both gallbladder and cystic duct without any associated atresia of the external hepatic bile duct, while the lack of vacuolation of the epithelium leads to an atretic gallbladder with patent cystic duct.[2] Until 2006, only 3 cases of gallbladder agenesis with a patent or hypoplastic cystic duct were reported.[3]
GA is often associated with other congenital abnormalities (12.8%–30%). It has been reported to be associated with gastrointestinal, cardiovascular, genitourinary, and skeletal malformations, such as duodenal atresia, malrotation of the gut, pancreas divisum, imperforate anus, hypoplasia of the right hepatic lobe, duplication cysts of the hepatic flexure, ventricular septal defect, renal agenesis, undescended testes, and syndactyly.[5] In particular, some authors report genitourinary anomalies as most frequently associated with GA.[6]
The etiology of GA is unknown, but generally it is accepted to be a congenital malformation.
The occurrence of the pathology is most often sporadic; however, there are reports of families where several members are affected by this condition, and this suggests the possible existence of hereditary forms.[2]
GA has also been reported in association with congenital syndromes, trisomy 18 and with congenital malformations caused by thalidomide.[4]
GA is usually asymptomatic (35%–60%).[3] Common symptoms include: right upper quadrant abdominal pain (90%), nausea and vomiting (66%), fatty food intolerance (37%), dyspepsia (30%), and jaundice (35%).[23] Moreover, bile duct stones are found in 25%–60% of symptomatic patients.[2] Most of these symptoms of GA may be explained as being associated with stasis in the bile duct (often dilated and taking on the function of bile storage), which can produce the clinical features of cholecystitis, cholangitis, and choledocholithiasis.[3]
Despite the high resolution of diagnostic imaging techniques, it has proved to be very difficult to make a correct preoperative diagnosis of GA in symptomatic patients. In fact, lots of “laparoscopic” diagnoses are reported in the literature.[37] If the diagnosis of GA is made during operation, the surgeon must prove GA by examining the most common sites for ectopic gallbladder (intrahepatic, retrohepatic, on the left side, within the leaves of the lesser omentum, within the falciform ligament, retroduodenal, retropancreatic, retroperitoneal).[5] Therefore, these patients are exposed to complications from prolonged exploration and it is suggested to abort the procedure rather than complete further exploration, if a gallbladder is not found on laparoscopy, since open exploration for possible ectopic gallbladder increases the risk of complications.[8]
Thus, preoperative diagnosis of GA is mandatory. Various authors have found ultrasound (US) scan to be misleading in interpreting a contracted and fibrotic gallbladder; therefore, most symptomatic patients are scheduled for surgery with a diagnosis of chronic cholecystitis with a contracted fibrosed gallbladder and a normal biliary tract.[9] Effectively a small, contracted (shrunken, scarred, sclerotic, or atrophied) gallbladder associated with stones and chronic cholecystitis will be difficult to visualize and US scan is highly operator-dependent.[23]
Significant progress in radiology and widespread availability of non-invasive imaging techniques, such as computed tomography, MRCP, and endoscopic ultrasound (EUS) provide an excellent alternative to open exploration and intra-operative cholangiography.[9] In particular, MRCP is considered the test of choice if there is suspicion, and it is also helpful in demonstrating an ectopic gallbladder along with other possible anomalies of the biliary tract system.[8] Nevertheless, as it does not require contrast administration to visualize the bile, it is not compromised by biliary stasis.[5]
There are no specific guidelines on how to manage patients with GA.[8] An algorithm published by Malde[10] suggests further radiologic investigation (MRCP, TC, ECRP, based on local availability) in symptomatic patients, when results from an US scan is doubtful because of gallbladder not being identified or reported as shrunken and suggestive of chronic cholecystitis.
Anyway, if the diagnosis is made during surgery, the operative strategy is finalized to exclude an aberrant gallbladder, and the diagnosis should be reconfirmed postoperatively by careful US scan.[2]
The majority of the patients reported in the literature became asymptomatic after the surgical procedures, even after nontherapeutic surgery. This is probably due to the lysis of the periportal and right hypochondrial adhesions[2] even though it remains unclear whether these patients would have had symptom resolution in the absence of exploration.[8] If symptoms continue postoperatively, a possible conservative treatment with oral smooth muscle relaxants and analgesics is effective.[3]
Otherwise, if the diagnosis is made preoperatively, there are generally 2 possible clinical situations: Patients with choledocholithiasis who should undergo ERCP (endoscopic retrograde cholangiopancreatography) and stone extraction or choledocholithotomy, or completely asymptomatic patients for whom no treatment or definitive procedure is required, as isolated GA has an excellent prognosis.[2]
CONCLUSION
In conclusion, GA is a significant diagnostic challenge, extremely difficult to diagnose before surgery with only US examination. Radiologists and clinicians should keep this entity in mind whenever the gallbladder is improperly visualized in routine imaging methods, in patients with or without biliary-type pain and also in patients with other known abnormalities/agenesis (genitourinary, gastrointestinal, cardiovascular, and others). MRCP technique cannot replace US scan in the management of acute gallbladder imaging, but it can represent a complementary study to inconclusive US studies, allowing a preoperative diagnosis of GA and avoiding unnecessary surgical exploration.
Source of Support: Nil
Conflict of Interest: None declared.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/17/95431
REFERENCES
- Multimodality imaging of pancreatic and biliary congenital anomalies. Radiographics. 2006;26:715-31.
- [Google Scholar]
- Agenesis of the gallbladder: Difficulties in management. J Gastroenterol Hepatol. 2005;20:671-5.
- [Google Scholar]
- Agenesis of the gallbladder with hypoplastic cystic duct diagnosed at laparoscopy. Surg Laparosc Endosc Percutan Tech. 2006;16:251-4.
- [Google Scholar]
- Abnormalities of the gallbladder, clinical effects. Surg Radiol Anat. 2008;30:285-90.
- [Google Scholar]
- Gallbladder agenesis and cystic duct absence in an adult patient diagnosed by magnetic resonance cholangiography: Report of a Case and review of the literature. Case Report Med. 2009;2009:674768.
- [Google Scholar]
- Malformations associated with congenital absence of the gall bladder. J Med Genet. 1983;20:445-9.
- [Google Scholar]
- Gallbladder and cystic duct absence.An infrequent malformation in laparoscopic surgery. Surg Endosc. 1997;11:483-4.
- [Google Scholar]
- Gallbladder agenesis diagnosed intra-operatively: A case report. J Med Case Reports. 2010;4:285.
- [Google Scholar]






