Translate this page into:
Adenoid Cystic Carcinoma of the Upper Trachea: A Rare Neoplasm
Address for correspondence: Dr. Binoy Kumar Choudhury, Department of Radiodiagnosis, Dr. Bhubaneswar Boroooah Cancer Institute, Gopinath Nagar, Guwahati - 781 016, Assam, India. E-mail: bkchoudhury@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Primary malignant tracheal tumors are not common and adenoid cystic carcinoma (ACC) of trachea is rare. We report an extremely rare case of ACC of proximal trachea, which was diagnosed in a 42-year-old male who presents with 6-month history of dyspnea. Lateral skiagram of neck, computed tomography, and magnetic resonance imaging revealed a broad-based polypoidal soft tissue mass arising from posterior wall of the proximal trachea. Biopsy confirmed the diagnosis of ACC. The patient was treated by surgical resection followed by radiotherapy and is on regular follow-up. Follow-up at 18 months post-treatment showed no local recurrence or distant metastases. The literature on tracheal ACC is reviewed. Image findings are briefly discussed.
Keywords
Adenoid cystic carcinoma
primary malignant tumor
trachea
INTRODUCTION

Primary tumors of the trachea are rare, occurring in less than 2 out of 1,000,000 persons per year representing less than 0.1% of cancer death.[1] Adenoid cystic carcinoma (ACC) is the second most common primary malignant tracheal neoplasm after squamous cell carcinoma.[23] ACC commonly arises at the distal portion of the trachea and its laryngeal involvement is extremely rare. Multidetector helical computed tomography (MDCT) and magnetic resonance imaging (MRI) may help in early diagnosis of this tumor. Early diagnosis and treatment is very essential for better prognosis. We present a rare case of ACC involving the proximal trachea and subglottis.
CASE REPORT
A 42-year-old male patient presents with a 6-month history of dyspnea. General physical examination did not reveal any significant abnormality. He had no history of smoking. The hematological and biochemical profile were essentially normal. Chest radiograph was within normal limits. Plain lateral radiograph of the neck revealed a broad-based polypoidal mass arising from the posterior wall of the proximal trachea [Figure 1]. Bronchoscopy confirmed the neoplasm. Histopatholgical examination of the mass confirmed it to be an ACC [Figure 2]. Patient suddenly developed severe respiratory distress and change of voice for which emergency tracheostomy was performed. CT and MRI were advised for treatment planning. MDCT [Figures 3 and 4] revealed a broad-based polypoidal soft tissue mass arising from the posterior wall of the proximal end of the trachea just below the cricoid cartilage and extending to involve the subglottis resulting in near total luminal obstruction. The tracheal mass eroded the tracheal cartilage and was abutting the right lobe of the thyroid. MRI [Figures 5 and 6] confirmed almost similar findings like CT. Metastatic work up which included CT thorax, abdominal ultrasound, and bone scan were normal. Surgical resection of the tumor was planned. Because of laryngeal extension, total laryngectomy and end-tracheostomy was performed in addition to resection of the tracheal segment. Histopathological examination of the surgical specimen confirmed the diagnosis of ACC. The patient also received external beam radiation therapy following surgery. The patient was on regular follow-up after the treatment. Follow-up of the patient after 18 months post-treatment did not reveal local recurrence or distant metastases.
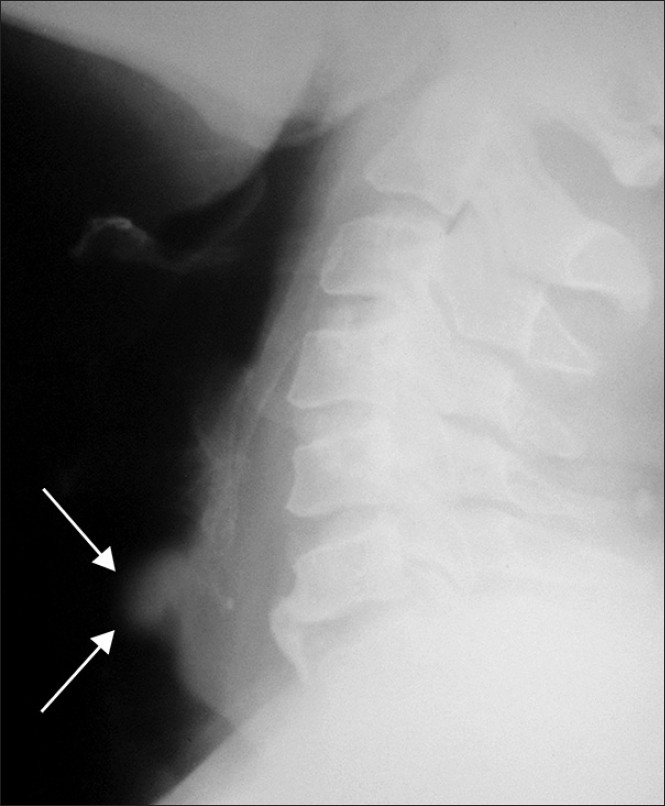
- 42-year-old man diagnosed with adenoid cystic carcinoma. Lateral radiograph of neck shows a broad-based polypoidal mass arising from the posterior wall of proximal end of trachea causing luminal narrowing (arrows).
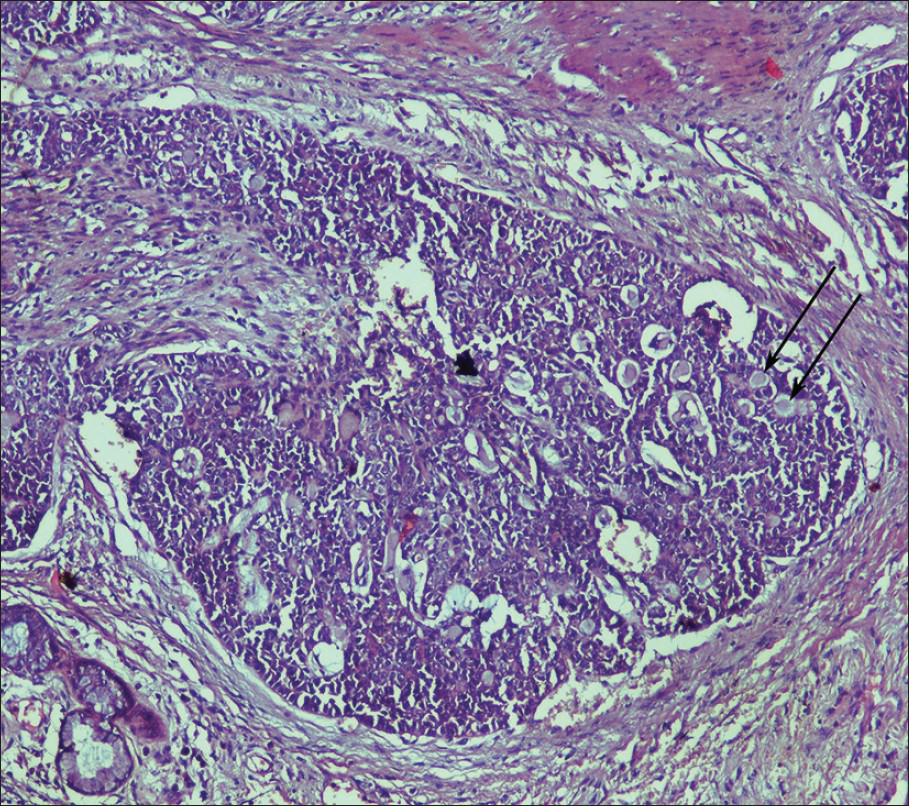
- 42-year-old man diagnosed with adenoid cystic carcinoma. High magnification (hematoxylin and eosin, ×100) photomicrograph of stained biopsy specimen shows neoplastic, moderately uniform round cells with hyperchromatic nuclei arranged in typical cribriform pattern of growth (arrows).
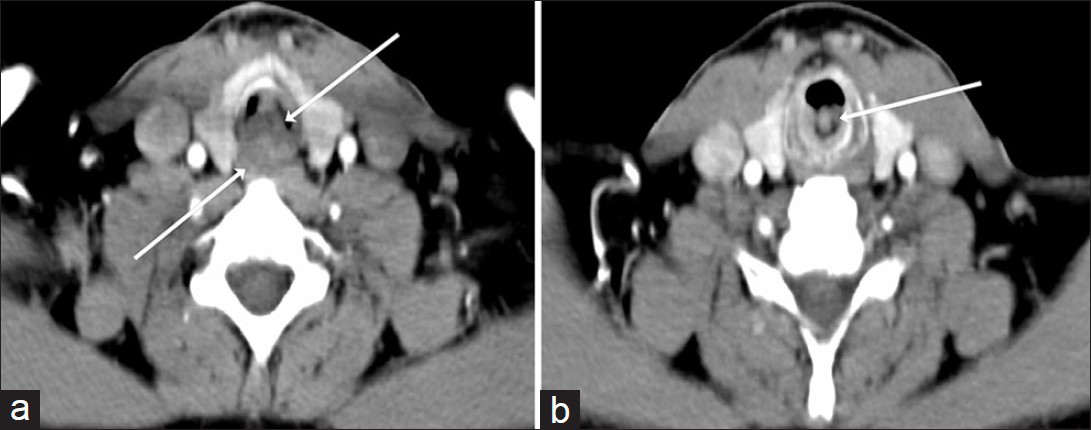
- 42-year-old man diagnosed with adenoid cystic carcinoma. (a) Contrast-enhanced axial computed tomography (CT) scan of neck shows a broad-based soft tissue mass (arrows) arising from posterior wall of upper end of trachea with both intraluminal and extraluminal components. Less than 180 degree circumference of trachea is involved. (b) CT scan obtained at the level of cricoid cartilage shows extension of tumor to subglottis (arrow).

- A 42-year-old man diagnosed with adenoid cystic carcinoma. Serial sagittal reformatted CT images (a-c) of neck show longitudinal extent of tumor (arrows) located at upper end of trachea extending to subglottis with both intraluminal and extraluminal components. Tracheostomy tube is seen inferior to the mass (arrowhead).
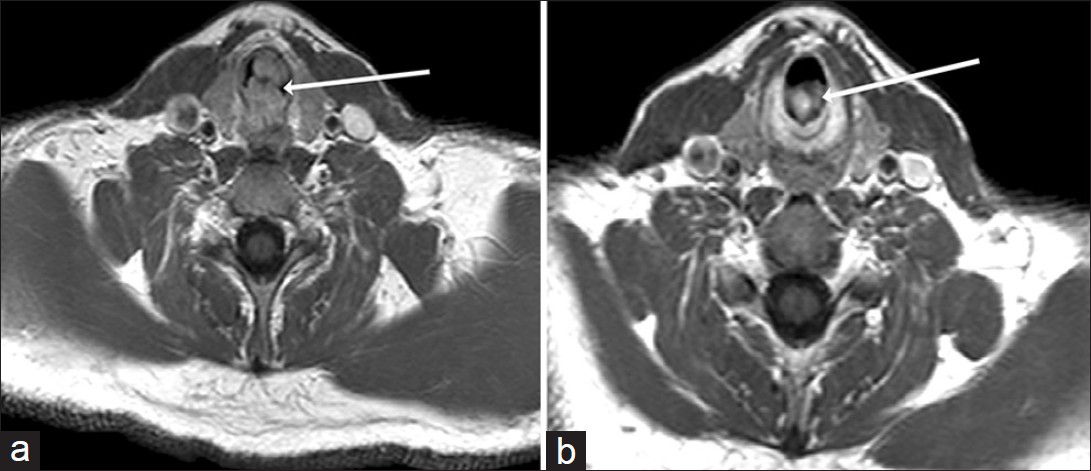
- 42-year-old man diagnosed with adenoid cystic carcinoma. (a) Axial magnetic resonance post-contrast T1-weighted image of neck shows broad-based soft tissue mass (arrow) arising from posterior wall of upper end of trachea causing near total luminal narrowing and having both intraluminal and extraluminal components. (b) Magnetic resonance image obtained at the level of cricoid cartilage shows extension of tumor to subglottis.
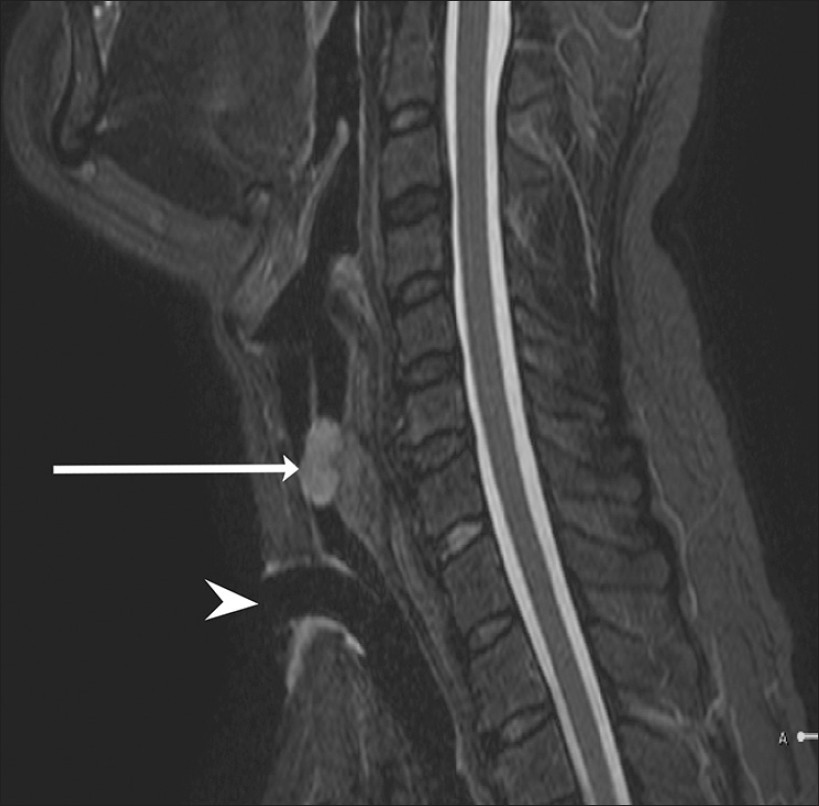
- 42-year-old man diagnosed with adenoid cystic carcinoma. Sagittal magnetic resonance Short Tau Inversion Recovery image of neck shows longitudinal extent of tumor (arrow) located at the level of upper end of trachea extending to subglottis causing almost complete luminal narrowing. Tracheostomy tube is seen below the level of tumor (arrowhead).
DISCUSSION
Primary malignant tracheal tumors are very uncommon. Squamous cell carcinoma is the most common primary tumor followed by ACC. These two tumors represent approximately 86% of primary malignant tracheal tumors in adults.[2] Tracheal tumors are usually malignant in adults and benign in children. ACC is predominantly a malignant tumor of the salivary glands and most common in the parotid gland representing about 10% of head and neck tumors.[4] ACC of the trachea is a rare neoplasm originating from submucosal glands of the tracheobronchial tree.[4] Tracheal ACC is found with almost equal frequency in males and females. ACC does not have definite association with cigarette smoking unlike squamous cell carcinoma. It is most common in patients in their 4th and 5th decades of life.[256] In the study by Calzada et al.,[4] ACC of the airway was described as laryngeal subsite and tracheal subsite. The laryngeal subsite was defined as the area between epiglottis superiorly and the cricoid cartilage inferiorly. The tracheal subsite was defined as the area distal to the cricoid cartilage. ACC is a low malignancy neoplasm having prolonged clinical course with late onset of metastases and late local recurrence.[137] It has a tendency to spread by direct extension, submucosally or along perineural planes and distant hematogenous spread. Pulmonary metastases are the most common distant metastases and may occur many years after treatment. However, occasional metastases have been reported to organs like liver, brain, bony skeleton, etc.[1] Lymphatic spread of tracheal ACC is relatively uncommon.[17] Lymph node metastases are reported in 10% of patients. Our patient did not have evidence of metastases at the time of diagnosis and 18 months after follow-up.
Most of the adult primary tracheal tumors arise in the distal third region of the trachea. In our patient, there was involvement of proximal trachea extending to the subglottis. ACC of proximal trachea is rare. ACC involving larynx is extremely rare and approximately 40 cases have been reported.[4] Symptoms associated with ACC are usually related to airway obstruction and these are dyspnea, cough, stridor, hemoptysis, wheezing, and change in voice. Unfortunately, many patients with ACC are mistakenly diagnosed and treated as asthma patients for months or years. Early diagnosis of ACC is important as it may improve surgical resectibility and thereby improve prognosis.
Routine chest X-rays and plain radiograph of neck are relatively insensitive in detecting tracheal lesion. However, sometimes plain radiograph of the neck maybe very helpful in detecting tracheal tumor as shown in our patient. On plain lateral radiograph, ACC of trachea may appear as broad-based or pedunculated polypoid mass. Tracheal wall may show smooth or nodular thickening with narrowing of lumen.[2] Both MDCT and MRI are very useful to assess the tracheal tumor radiologically. These two modalities help to demonstrate the primary tumor, its extent, and delineation of its relation to adjacent structures. MDCT has revolutionized the radiological assessment of the central airways with better quality of multiplanar and three-dimensional reconstruction images.[8] CT is considered to be the standard imaging modality for assessment of tracheal tumor and the reformatted images demonstrate both intraluminal and extraluminal extent of the tumor in addition to evaluation of its relationship to adjacent structures.[910] ACC has a tendency toward submucosal extension and on CT it appears as an intraluminal mass of soft tissue attenuation with extension through tracheal wall. Sometimes, the lesion may present as diffuse or circumferential wall thickening, a soft tissue mass filling the tracheal lumen, or thickened tracheal wall encircled by soft tissue mass in the transverse and longitudinal planes.[9] Craniocaudal extent of the lesion is usually greater than axial extent. More than 180 degree circumference of the trachea are usually involved.[9] These tumors are variable in shape (broad-based or polypoid) and margins (irregular, smooth, or lobulated).[9] Calcifications within the tumor are rare. MRI is also useful for assessment of tracheal tumor and its extent just like MDCT. However, MRI does not have distinct advantage over CT in the evaluation of tracheal tumors.[10] Our case highlights the importance of both imaging modalities in preoperative assessment of tracheal ACC.
Treatment of ACC includes surgery, radiotherapy, and combination of both.[3] However, recommended treatment consists of surgical resection with postoperative radiotherapy.[14] Early diagnosis and treatment by surgery with radiation therapy provide significantly prolonged survival or even the possibility of complete remission. Therefore, surgeons and radiologists should be aware of this rare tumor. Our patient is doing very well 18 months after surgery and postoperative radiotherapy without any evidence of local recurrence or distant metastases. Long-term survival of patients of ACC depends on the presence of distant metastases.[4] Therefore, regular follow-up at 6-month interval is very important.
CONCLUSION
ACC of the trachea is a rare primary malignant tumor in adults. MDCT is the imaging modality of choice for assessment of the tumor, its extension, and distant metastases. Surgical resection followed by radiotherapy is widely recommended protocol for treatment and provides the best chance of prolonged survival. Radiologists should be aware of this rare neoplasm as early diagnosis and treatment are essential for its improved prognosis.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2013/3/1/39/119021
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- Adenoid cystic carcinoma of the airway: Thirty-two-year experiences. J Thorac Cardiovasc Surg. 1996;112:1522-31.
- [Google Scholar]
- Trachea: Anatomy and Pathology. In: Som PM, Curtin HD, eds. Head and Neck Imaging (4th ed). St Louis Missouri: Mosby; 2003. p. :1700-26.
- [Google Scholar]
- Adenoid cystic carcinoma of the trachea: A report of seven cases and literature review. Chang Gung Med J. 2005;28:357-63.
- [Google Scholar]
- Adenoid cystic carcinoma of the airway: A 30-year review at one institution. Am J Otolaryngol. 2012;33:226-31.
- [Google Scholar]
- Adenoid cystic carcinoma of the trachea treated with PET-CT based intensity modulated radiotherapy. J Thorac Oncol. 2008;3:793-5.
- [Google Scholar]
- Multislice helical CT of the central airways. Radiol Clin North Am. 2003;41:561-74.
- [Google Scholar]
- Adenoid cystic carcinoma of the airways: Helical CT and histopathologic correlation. AJR Am J Roentgenol. 2004;183:277-81.
- [Google Scholar]






