Translate this page into:
Additional Merits of Two-dimensional Single Thick-slice Magnetic Resonance Myelography in Spinal Imaging
Address for correspondence: Dr. Rajiv Azad, Department of Radiology, SGRR Institute of Medical and Health Sciences, Patel Nagar, Dehradun - 248 001, Uttarakhand, India. E-mail: rajivas23@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
To validate the additional merits of two-dimensional (2D) single thick-slice Magnetic Resonance Myelography (MRM) in spinal imaging.
Materials and Methods:
2D single thick-slice MRM was performed using T2 half-Fourier acquisition single-shot turbo spin-echo (HASTE) sequence in addition to routine Magnetic resonance (MR) sequences for spine in 220 patients. The images were evaluated for additional diagnostic information in spinal and extra-spinal regions. A three-point grading system was adopted depending upon the utility of MRM in contributing to the detection of spinal or extra-spinal findings. Grade 1 represented no contribution of MRM while grade 3 would indicate that it was essential to detection of findings.
Results:
Utility of MRM in spine was categorized as grade 3 in 10.9% cases (24/220), grade 2 in 21.8% (48/220) cases and grade 1 in 67.3% cases (148/220). Thus, the overall additional merit of MRM in spine was seen in 32.7% (72/220) of cases. Besides in 14.1% cases (31/220) extra-spinal pathologies were identified.
Conclusion:
2D single thick-slice MRM could have additional merits in spinal imaging when used as an adjunct to routine MR sequences.
Keywords
Magnetic resonance
myelography
spine
INTRODUCTION

Magnetic resonance myelography (MRM) has been developed to evaluate the spinal subarachnoid space non-invasively. In addition, advantages of MRM as compared to conventional or computed tomography (CT) myelography are that it does not involve the use of intrathecal contrast or radiation.[1–4] On the heavily T2-weighted sequence used in this technique, cerebro-spinal fluid (CSF) in the subarachnoid space has hyperintense signal while normal or abnormal soft tissue structures are seen as filling defects or extrinsic compressions. MRM can be obtained either by multi-slice or single-slice techniques. Images obtained with single-slice thick-slab techniques require very short time as compared to multi-slice techniques. In addition, single-slice technique of MRM provides excellent suppression of background signals (from fat or paravertebral veins) and has significantly reduced CSF flow artifacts.[35–7] MRM has been previously used to assess spinal stenosis and nerve root compression with some benefits.[8–10] The aim of this study is to evaluate the advantages of routine use of 2-D single thick-slice MRM in providing additional information in spinal and extra-spinal regions.
MATERIALS AND METHODS
Subjects
The study was conducted in a tertiary care hospital after ethical committee approval. Normal Magnetic resonance imaging (MRI) examinations were excluded from the study. MRI data of 220 patients was retrospectively examined. The study included all patients who were referred for MR imaging irrespective of age, sex or clinical presentation. The study group included 143 cases that had mild to severe degenerative disease, 13 cases of congenital variants or abnormalities, 17 cases of tuberculous spondylitis, 12 cases of primary or secondary spinal tumors and 35 cases of spinal trauma.
Magnetic resonance imaging technique
The MR imaging examinations were performed by using an 18 channel, 1.5-T Avanto system (Siemens, Erlangen, Germany). Single thick-slice MRM projection images were obtained in mid-sagittal and coronal planes in addition to the routine MR sequences. T2 half-Fourier acquisition single-shot turbo spin-echo (HASTE) sequence was used with extremely long echo time (TE) of 1200 ms and repetition time (TR) of 8000 ms. Other sequence parameters were echo train length = 369, slice thickness = 50 mm, field of view = 280-400 mm, flip angle = 150, base resolution = 512, phase resolution = 72, signal to noise ratio (SNR) =1 and NEX = 2. Image matrix was 369 × 512 with voxel size of 0.8 × 0.5 × 50 mm. MRM images for a single region required an imaging time of 34 sec while whole spine MRM required an additional 34 sec. The MRM views of entire spine could be processed in single image using Total imaging matrix (TIM) technology by stepwise moving the patient table without repositioning the patient or changing the coil.
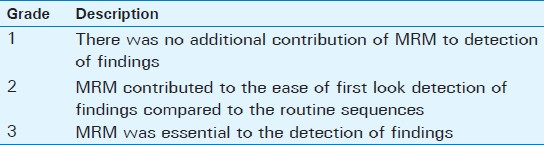
Image interpretation
One radiologist evaluated the MRM images while the second radiologist with sub-specialty training in neuroradiology evaluated the routine MR sequences. Each radiologist was blind to the other set of images. We tried to grade the additional merits of MRM in spinal and extra-spinal regions by using a 3 point grading scale which was modified from the one used by O’Connell et al. (2003),[8] [Table 1].
RESULTS
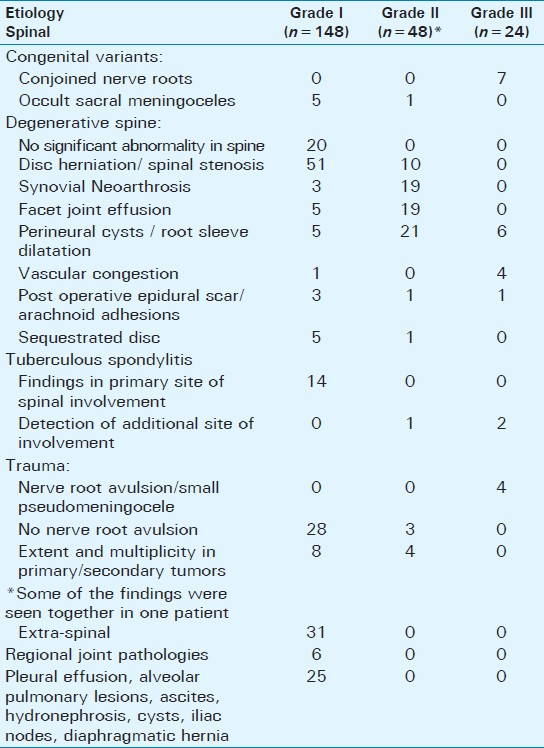
The utility of MRM was categorized as grade 3 in 10.9% cases (24/220) and grade 2 in 21.8% (48/220) cases [Table 2]. Thus, the overall additional merit of MRM in spine was seen in 32.7% (72/220) of cases. In 67.3% cases (148/220), the MRM did not give any contribution to the final diagnosis (grade 1). Extra-spinal pathologies were identified in 14.1% (31/220) cases on MRM.
DISCUSSION
MRM has been compared to conventional and CT myelography previously. Pictorial quality and resolution of conventional and CT myelography in evaluating thecal sac and nerve roots is better than that of MRM. We accept these facts but conventional and CT myelography are invasive procedures requiring contrast injection into the thecal sac with potential complications.[1–4]
Multi-slice as well as single-slice techniques have been used for obtaining MRM. Multi-slice techniques using fast spin-echo (FSE) sequences require long acquisition times and post processing of the data.[11] Single-slice MRM has been attempted with various sequences including rapid acquisition with relaxation enhancement (RARE),[712] single-shot turbo spin-echo (with long effective TE),[3] and T2 half-Fourier acquisition single-shot turbo spin-echo (HASTE).[8] Single-slice MRM is faster, does not require any post processing, provides excellent suppression of background signals and has markedly reduced CSF flow artefacts. However, limited data is available about the additional benefits of single-slice MRM as a routine sequence in spinal imaging.[8–10]
We selected HASTE for acquiring single thick-slice MRM images in two planes. O’Connell et al., also acquired MRM images using this sequence with following parameters; slice thickness: 20 mm, echo train length: 256, FOV: 25 cm and acquisition time of 3 min 20 sec.[8] We have modified the sequence parameters and used thicker slab (50 mm), and increased the echo train length (369) and field of view (28-40 cm). By using this protocol, we were able to obtain good quality images with negligible CSF pulsation artefacts and excellent suppression of background signal in a very short time of 34 seconds for single region and 68 seconds for whole spine. The larger FOV and thicker slab significantly reduced the image acquisition time and it also became easier for us to screen for abnormal fluid signal in extra spinal regions, nearby organs and joints.
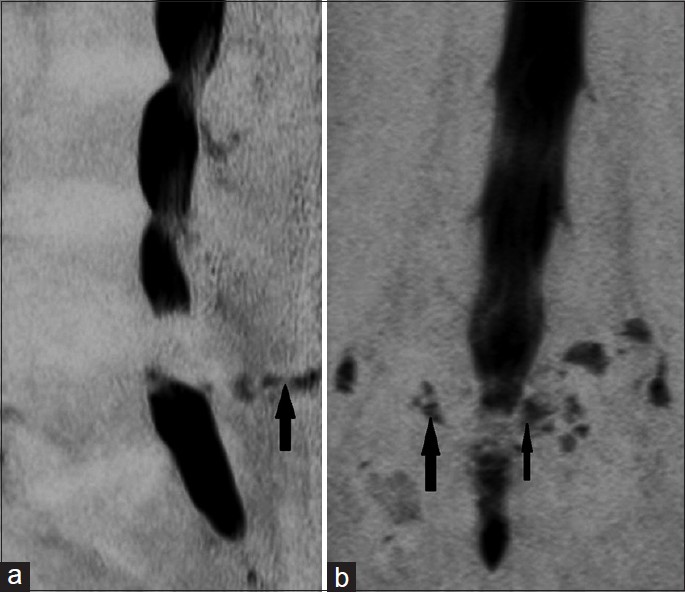
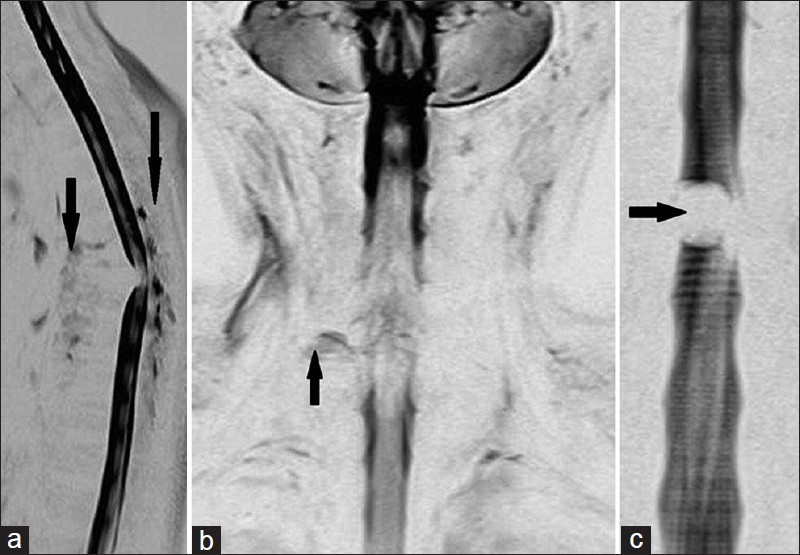
MRM has still not been uniformly recommended for routine use in spine because of long acquisition times and presumably limited information although previous studies have evaluated its role in diagnosing various spinal diseases.[235681112] The potential use of MRM in evaluating fluid signal in extra-spinal regions has not been studied previously. However, by employing this single-slice thick-slab technique of MRM in two planes, we could add diagnostic information in a substantial number of cases without any significant addition of imaging time or cost [Figures 1–9]. In our study, conjoined nerve roots and traumatic nerve root avulsions could be diagnosed only on MRM [Figure 2, 3b and 5]. MRM also demonstrated diagnostic or at least an initial interpretative value in intrathecal vascular congestion, post operative scars, arachnoid adhesions and sequestrated discs [Figure 7, 9]. The heavily T2-weighted sequence and larger FOV employed in our study resulted in prompt detection of additional foci of incidental or abnormal fluid signal in spinal or extra-spinal locations. Perineural cysts, synovial neoarthrosis and facetic effusions could be detected on MRM even by the relatively inexperienced observer [Figure 1]. It was also possible to reveal diaphragmatic hernia, ascites, regional joint pathologies and lymphadenopathy in patients who were just referred for spinal imaging. These findings had clinical significance in some patients. Routine spinal imaging [Figure 4] sequences were limited in providing information about these extra-spinal findings in the first look due to the limited FOV and anterior saturation bands which resulted in a signal drop anterior to the spine.
- (a, b) Magnetic myelography images in degenerative spine. (a) Sagittal image shows synovial neoarthrosis (black arrow), (b) Coronal image depicts facetic effusion (broad black arrow), Parafacetal cysts(thin black arrow).

- (a-c) Magnetic resonance myelograms in congenital variants/ abnormalities. (a) Coronal image demonstrates conjoined nerve roots (leftsided black arrow), tarlov's cyst (right-sided black arrow), (b) Sagittal image shows syrinx in diastematomyelia (black arrow), and (c) Sagittal image shows incidental occult sacral meningocele (black arrow).
- (a-c) (a) Sagittal image shows prevertebral and posterior epidural collection in tuberculous spondylitis, (b) Coronal image reveals pseudomeningocele secondary to nerve root avulsion, and (c) Coronal image demonstrates a well defined intradural filling defect due to meningioma. (Findings marked with black arrows).

- (a-c) Coronal magnetic resonance myelograms depicting various additional extra-spinal findings(black arrows), (a) Diaphragmatic hernia and left glenohumeral joint effusion, (b) Residual apical scar in chronic pulmonary tuberculosis, and (c) Small left-sided iliac lymph nodes.
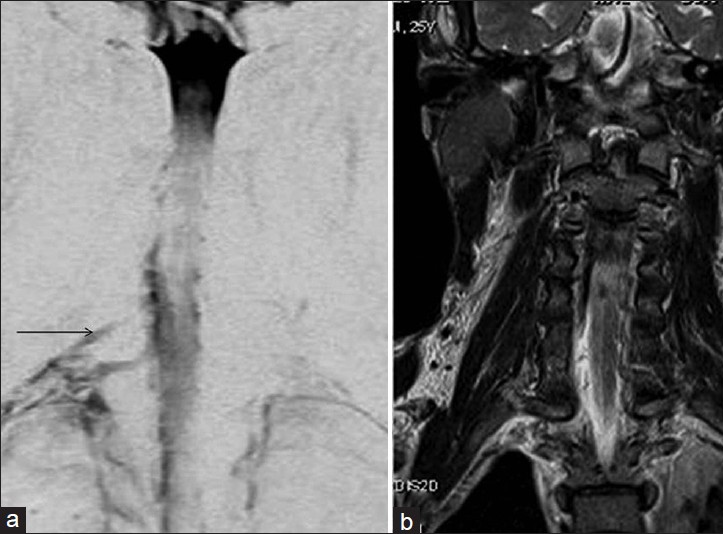
- a) Coronal magnetic resonance myelogram clearly shows nerve root avulsion (black arrow) compared to b) routine coronal T2 sequence scan.
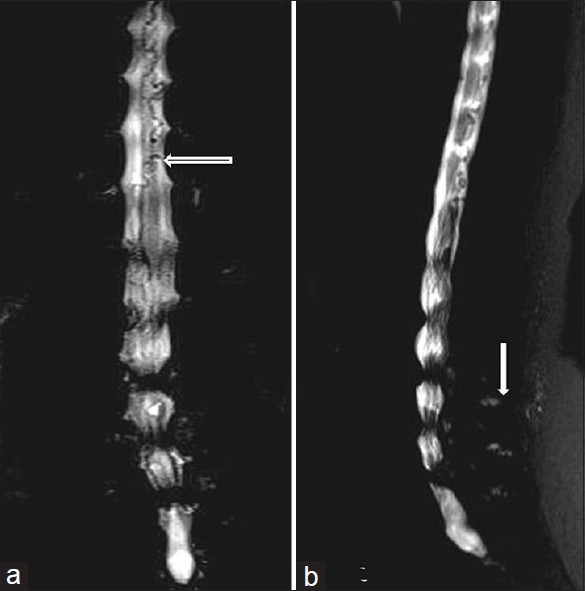
- a) Coronal and b) sagittal single thick-slice magnetic resonance myelograms show simultaneous first look detection of significant lumbar canal stenosis, spinal arterio-venous malformation (a) and synovial neoarthrosis (b). (Findings marked with white arrows).

- a) Coronal magnetic resonance myelogram reveals Intrathecal vascular congestion proximal to the level of spinal canal block (a-white arrow) while on b) Coronal T2 weighted image it is difficult to differentiate vessels from nerve roots.
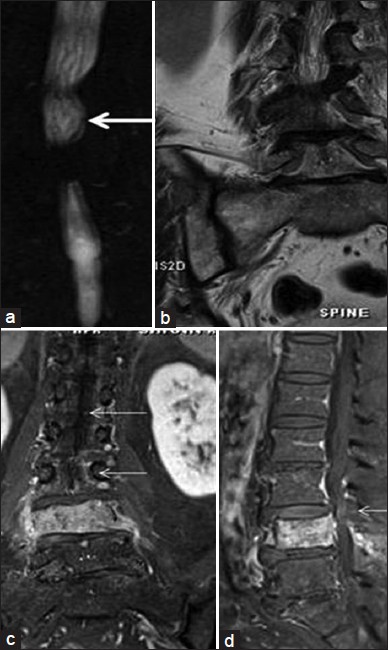
- Spinal intradural metastatic deposits. a) Coronal magnetic resonance myelographyshows thickening and nodularity of cauda equina nerve roots (white arrow) which on b) coronal T2 sequence is not discernable. Post-contrast fat-suppressed T1 sequence c) Coronal and d) Sagittal views show nodular enhancement along cauda equina nerve roots on reevaluation (white arrows).

- (a-f) Post-operative case of lumbar disc herniation. a) Coronal magnetic resonance myelogram depicts focal asymmetrical irregularity of margin of thecal sac on right side with root sleeve blunting and subtle thickening of cauda equina nerve roots cranially (black arrows). Routine T2 images b) sagittal, c) coronal, d) axial views the findings are difficult to delineate. On post-contrast fatsuppressed T1 sequence e) coronal, f) axial no abnormal enhancement is seen.
Limitations
In the single thick-slice technique, images are available in only two planes. At times, this leads to incomplete evaluation of spinal canal stenosis and difficulty in localization of the source of fluid signal. A repetition of the sequence is also required if the plane is not chosen correctly. Thicker slab selection can possibly lead to cross talk of the data but it was not experienced in our study.
CONCLUSION
Two-Dimensional single thick-slice MRM sequence could have additional merits in complimenting routine MR sequences in spinal imaging. We suggest that MRM using this technique be included in the routine spinal MRI protocol. It could aid in detection of abnormal fluid signals in the spinal and extra spinal regions and provide additional information beyond the referred region of interest without significantly prolonging overall imaging time.
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/84/105268
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- MR-myelography: A comparison with conventional myelography. Eur J Radiol. 1996;21:196-200.
- [Google Scholar]
- Evaluation of magnetic resonance myelography in the investigation of cervical spondylotic radiculopathy. Br J Radiol. 2003;76:525-31.
- [Google Scholar]
- Magnetic resonance myelography (MRM) as a spinal examination technique. Acta Neurochir (Wien). 1997;139:1080-4.
- [Google Scholar]
- MR myelography using heavily T2-weighted fast spin-echo pulse sequences with fat presaturation. AJR Am J Roentgenol. 1992;159:1315-20.
- [Google Scholar]
- Rapid lumbar spine MR myelography using rapid acquisition with relaxation enhancement. AJR Am J Roentgenol. 1997;168:377-8.
- [Google Scholar]
- The value of routine MR myelography at MRI of the lumbar spine. Acta Radiol. 2003;44:665-72.
- [Google Scholar]
- Value of MR myelography in the diagnosis of spine disorders. Med Clin (Barc). 2000;115:366-9.
- [Google Scholar]
- Value of magnetic resonance myelography in the diagnosis of disc herniation and spinal stenosis. Australas Radiol. 2000;44:281-4.
- [Google Scholar]
- Rapid non-tomographic approach to MR myelography without contrast agents. J Comput Assist Tomogr. 1986;10:375-8.
- [Google Scholar]






