Translate this page into:
Acute traumatic subtalar dislocation: A rare but important clinical entity with 15-year retrospective radiological analysis of 23 cases
*Corresponding author: King Shing Yung, Department of Radiology, Princess Margaret Hospital, Kwai Chung, Hong Kong. yungkingshing@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yung K, Kwok H, Pan N, Lo B. Acute traumatic subtalar dislocation: A rare but important clinical entity with 15-year retrospective radiological analysis of 23 cases. J Clin Imaging Sci. 2024;14:30. doi: 10.25259/JCIS_8_2024
Abstract
Objectives:
The objectives of this study were to contribute to the limited existing knowledge about subtalar dislocations, analyze the computed tomography (CT) findings and advantages over radiography, and report the rate and potential risk factors of post-traumatic peri-talar osteoarthritis (OA).
Material and Methods:
A total of 23 cases of traumatic subtalar dislocation during a 15-year period at three regional hospitals were retrospectively reviewed.
Results:
All 23 cases were closed dislocations. Successful close reduction was performed in 17 patients (73.9%) and 6 patients (26.1%) required open reduction and internal fixation. Twenty patients (87%) had associated foot and ankle fractures. Fractures of calcaneal medial tubercle were the most common (75%), followed by talar head (30%), sinus tarsi (25%), and medial malleolus (25%). The radiograph’s sensitivity for identifying fractures was 48.1%. The mean follow-up period is 30 months. Symptomatic OA affected 8 patients (36.4%). No post-trauatic talar avascular necrosis was noted. Fractures were present in all of those patients with post-traumatic OA (100%). Three out of five patients who sustained high-energy mechanism injury developed radiographic OA (66.7%). Three out of six patients (50%) treated with open reduction and internal fixation also developed radiographic OA.
Conclusion:
Subtalar dislocation remains a rare injury. It is strongly associated with foot and ankle fractures. Fractures of the calcaneal medial tubercle were the most common. The risk of post-traumatic symptomatic peritalar OA is high. CT is useful in detecting occult fractures and injured bony subregions. We postulated potential risk factors of post-traumatic OA (fracture, high-energy mechanism of injury, open reduction, and internal fixation); however, this requires further study.
Keywords
Acute traumatic dislocation
Osteoarthritis
Subtalar joint
INTRODUCTION
Subtalar joint (STJ) dislocation is a rare condition and has a strong association with fractures of the foot and ankle, which can result in significant morbidity. This study aimed to contribute to the existing knowledge about subtalar dislocations, evaluate the findings of multidetector computed tomography (MDCT), analyze the advantages of MDCT over conventional radiography, and report the rate and potential risk factors of post-traumatic peri-talar osteoarthritis (OA) following subtalar dislocations.
MATERIAL AND METHODS
This retrospective study took place at three regional hospitals in Hong Kong, including Princess Margaret Hospital, Caritas Medical Centre, and Tseung Kwan O Hospital. The electronic patient record and radiology information system of the institutions were utilized to obtain all computed tomography (CT) reports and relevant clinical data for subtalar dislocations from January 2008 to November 2023. Inclusion criteria included patients who sustained subtalar dislocations due to acute traumatic events, with or without polytrauma. Exclusion criteria included non-traumatic subtalar dislocation. During this 15-year period, we found 24 MDCT examinations of traumatic subtalar dislocations, of which 23 cases met the inclusion criteria. One case of non-traumatic subtalar dislocation caused by neuropathic arthropathy was excluded from the study.
We reviewed the patient demographic information and relevant radiological findings. The following details were documented: Laterality of the injury, type of subtalar dislocation (medial, lateral, anterior, posterior, and closed versus open), mechanism of injury, radiographic and CT findings, the treatment and surgical intervention, as well as a follow-up outcome. Radiographic OA was, further, documented according to the Kellgren-Lawrence classification [Table 1].
| Grade | Radiographic findings |
|---|---|
| 0 | No radiographic evidence of osteoarthritis |
| 1 | Possible osteophytes and/or doubtful narrowing of joint space |
| 2 | Definite osteophytes and possible narrowing of joint space |
| 3 | Moderate multiple osteophytes, definite narrowing of joint space, small pseudocystic areas with sclerotic walls, and possible deformity of bone contour |
| 4 | Large osteophytes, marked narrowing of joint space, severe sclerosis, and definite deformity of bone contour |
The diagnosis of acute traumatic subtalar dislocations in this retrospective investigation was based on MDCT, which was regarded as the gold standard. A radiologist with more than 10 years of experience in musculoskeletal imaging was involved in the retrospective evaluation of imaging studies.
RESULTS
The mean age of the patients was 46.7 (range 8–72) years at the time of injury. Injuries are more prevalent in older age groups: Individuals between the ages of 8 and 30 (four cases; 17.4% of subtalar dislocations); individuals between the ages of 31 and 50 (eight cases; 34.8% of subtalar dislocations); and individuals between the ages of 51 and 72 (11 cases; 47.8% of subtalar dislocations). Out of the 23 patients, the mean age of 14 males was 42.9 years, and the mean age of nine females was 52.8 years.
All 23 patients had their mechanism of injury documented; low-energy trauma (sports activities and fall from ground levels) accounted for 18 instances (78.2%), whereas high-energy trauma (motor vehicle accidents and falls from heights) accounted for 5 cases (21.8%).
All of the 23 cases of subtalar injuries were closed dislocations, with medial dislocations accounting for the majority of cases (22 cases; 95.7%). Only one lateral dislocation (4.3%) was identified. No anterior or posterior subtalar dislocation was found. Subtalar dislocation occurred on the left lower extremity in 12 patients (52.2%) and right in 11 patients (47.8%).
Closed reduction was performed successfully before MDCT examinations in 17 patients (73.9%). In six patients (26.1%), open reduction of the subtalar dislocations was required.
Of the 23 patients, 20 (87%) had associated ipsilateral foot and ankle fractures. Only 3 patients (13%) experienced an isolated subtalar dislocation without a corresponding fracture detected on CT. Of the 20 patients with CT-detected fractures, talar medial tubercle fracture was the most common (15 patients; 75%), followed by talar head fracture (six patients; 30%), sinus tarsi fracture (five patients; 25%), and medial malleolus fracture (five patients; 25%). Other associated fractures include calcaneum (four patients; 20%), talar neck (three patients; 15%), talar body (two patients; 10%), lateral malleolus (two patients; 10%), navicular (two patients; 10%), and fifth metatarsal (two patients; 10%). Injury to the talar lateral tubercle was uncommon (one patient; 5%). The number of associated injuries is shown in Table 2. The imaging findings are shown in Figures 1-4.
| Fracture location | No. of cases | Percentage |
|---|---|---|
| Talus | 19 | 95 |
| Neck | 3 | 15 |
| Medial tubercle of posterior process | 15 | 75 |
| Sinus tarsi | 5 | 25 |
| Head | 6 | 30 |
| Body | 2 | 10 |
| Lateral tubercle | 1 | 5 |
| Calcaneum | 4 | 20 |
| 5th metatarsal | 2 | 10 |
| Medial malleolus | 5 | 25 |
| Lateral malleolus | 2 | 10 |
| Navicular | 2 | 10 |
CT: Computed tomography

- A 46 year-old man sustained a right subtalar medial dislocation secondary to inversion sprain. Conventional radiographs in (a) lateral and (b) anteroposterior views showed evidence of fracture navicular and posterior process of talus with open reduction and K wire fixation done. Follow-up radiographs in 50 months post-injury in (c) lateral and (d) anteroposterior views showed osteophytes formation, joint space narrowing, subchondral sclerosis and mild bony deformity involving talonavicular and subtalar joints, in keeping with grade III osteoarthritis. (R: Right)

- A 63 year-old female sprained her right ankle during hiking resulting in subtalar medial dislocation. CT scan in (a) lateral view and three-dimensional reconstruction images in (b) anteroposterior and (c) lateral views showed previous open reduction and internal fixation, and associated bimalleolar fracture as well as intra-articular talar fracture involving the sinus tarsi. (d) MRI in T1-weighted and (e) T2-weighted fat-saturated sequences lateral views reviewed fat obliteration and edema at the sinus tarsi. Follow-up radiograph in (f) anteroposterior and (g) lateral views at 31 months after injury showed grade III osteoarthritis involving subtalar, talotibial and talonavicular joints. (MRI: Magnetic resonance imaging, CT: Computed tomography, RT, R: right)
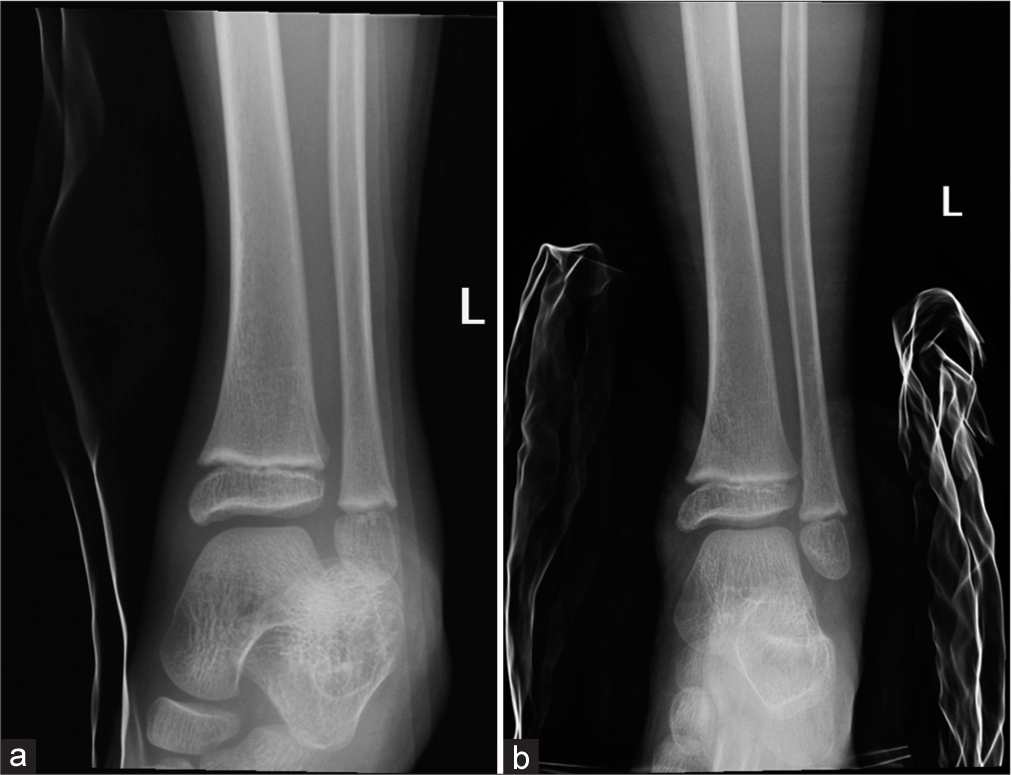
- A 8 year-old female sustained a left ankle injury during cycling where her ankle was trapped in the wheel. Radiographs in (a) anteroposterior view showed subtalar lateral dislocation, (b) which was successfully reduced. (L: left)

- A 41 year-old male sustained a right subtalar medial dislocation during a basketball game. Conventional radiographs performed after reduction in (a) oblique, (b) lateral and (c) frontal views did not reveal obvious fracture. CT in (d) axial and (e) lateral showed comminuted fracture of the talus involving the medial tubercle and posterior process, which were not visible on conventional radiographs. (R: Right)
For all 23 patients, primary radiographs were available in 100% of the cases. The radiographs overall sensitivity for identifying fractures was 48.1% [Table 3].
| Fracture location | No. of fractures on CT | Radiography | |
|---|---|---|---|
| True-positive | Sensitivity (%) | ||
| Talus | 19 | 8 | 42.1 |
| Calceaneum | 4 | 0 | 0 |
| 5th metatarsal | 2 | 1 | 50 |
| Medial malleolus | 5 | 2 | 40 |
| Lateral malleolus | 2 | 1 | 50 |
| Navicular | 2 | 1 | 50 |
| Total: | 27 | 13 | 48.1 |
CT: Computed tomography
One of the patients defaulted initial follow-up visit. The mean follow-up period for the remaining 22 patients is 30 months. OA affected eight patients (36.4%), and STJs were involved in all of those cases. There was talotibial OA in 1 (4.5%) and talonavicular OA in 4 (18.1%) of the cases. Four out of eight patients developed grade III OA (50%). The radiographic outcomes, the incidence of OA, and symptoms following subtalar dislocations are shown in Tables 4 and 5. In addition, no talar avascular necrosis was identified from the 23 cases studied.
| Joint | Osteoarthritis | ||||
|---|---|---|---|---|---|
| Grade 0 (no radiographic change) | Grade 1 | Grade 2 | Grade 3 | Grade 4 | |
| Subtalar | 14 | 2 | 2 | 4 | 0 |
| Talonavicular | 18 | 2 | 1 | 1 | 0 |
| Talotibial | 21 | 0 | 0 | 1 | 0 |
G1-G4: indicates grades of modified kellgren lawrence classification of osteoarthritis (table 1)
| Asymptomatic | Symptomatic | Percentage of symptomatic patients | |
|---|---|---|---|
| Osteoarthritis present | 0 | 8 | 100 |
| Osteoarthritis absent | 9 | 5 | 35.7 |
The influence of fracture, mechanism of injury, and treatment on radiographic OA is shown in Table 6. Fractures were present in all of those patients with post-traumatic OA. No OA was noted in those three patients with isolated subtalar dislocations. Among five patients who have sustained high energy mechanism injury, three of them (66.7%) developed radiographic OA. Three out of six patients (50%) treated with open reduction and internal fixation also developed radiographic OA subsequently. While there might be a possibility of an association between the above factors and the risk of post-traumatic OA, no significant statistical association was proven, possibly due to the limited sample size.
| Number of patients with CT detected fracture | Number of patients without CT detected fracture | High-energy mechanism injury | Low-energy mechanism injury | Open reduction and internal fixation | Closed reduction | |
|---|---|---|---|---|---|---|
| Osteoarthritis present | 8 | 0 | 3 | 5 | 3 | 3 |
| Osteoarthritis absent | 12 | 3 | 2 | 13 | 3 | 14 |
CT: Computed tomography
DISCUSSION
Traumatic subtalar dislocation is a rare injury, comprising approximately 1% of all traumatic foot injuries.[1] Because this injury is relatively uncommon, it is currently only illustrated at the case report and case series levels. Nonetheless, due to its strong association with foot and ankle fractures, which cause severe morbidity, it is of significant clinical relevance. Only 23 occurrences of traumatic subtalar dislocations were found when cases at three regional hospitals over a 15-years period were retrospectively reviewed. This suggests that more research is necessary to fully understand the rarity of this condition.
To the best of the authors’ knowledge, Bibbo et al. case series in 2003, where 25 cases of subtalar dislocations were included, was the biggest contemporary case series of traumatic subtalar dislocations.[2] They demonstrated that 88% of the patients had concomitant foot and ankle injuries, and 89% of the patients showed subsequent radiographic changes of the STJs at the mean follow-up of 5 years. Another case series with 13 cases of traumatic subtalar dislocations at a mean follow-up of 6 years is that of Ruhlmann et al. in 2017,[3] in which they illustrated a significant risk of post-traumatic subtalar and talonavicular OA in 46.1% and 23.1% of the cases, respectively. The most recent case series, by Sakkab et al. in 2022, comprised six examples of traumatic subtalar dislocations,[4] where concomitant ankle fractures were present in 50% of the cases, and post-traumatic OA involving the subtalar and talonavicular joint in 50% and 16.7%, respectively. They are graded by Kellgren-Lawrence classification for OA [Table 7].
| Case series | Patient number | Mean follow-up time (months) | Associated foot and ankle injuries (%) | Injured subregions of individual bones | Post-traumatic peri-talar osteoarthritis (%) | Grading of post-traumatic peri-talar osteoarthritis | Sensitivity of radiograph in detecting associated injuries | The AOFAS score |
|---|---|---|---|---|---|---|---|---|
| Our study | 23 | 30 | 87 (most common talar fracture) | Yes (most common talar medial tubercle, talar head and sinus tarsi) | 36.4 | Yes | 48.1% | - |
| Bibbo et al.[2] | 25 | 61 | 88 (most common talar fracture) | - | 89 | - | - | Yes |
| Ruhlmann et al.[3] | 13 | 72 | - | - | 46.2 | - | - | Yes |
| Sakkab et al.[4] | 6 | 17.7 | 50 (most common fibular fracture) | - | 50 | Yes | - | - |
AOFAS: American orthopedic foot and ankle society
We showed a strong association between subtalar dislocations and foot and ankle injuries, with talus injuries occurring most frequently, which is consistent with the findings in other case series.
We made a further contribution by describing related fractures of the foot and ankle based on distinct subregions of the separate bones on MDCT. This has important clinical significance. For instance, an undiagnosed fracture of the talus’s medial tubercle could potentially cause injury to the hallucis longus tendon, which could be interpositioned in between the fragments and make reduction challenging.[5] Another illustration is the increased risk of avascular necrosis in cases with talar neck fractures.[6] The authors are aware of no case series with subtalar dislocations that have documented fracture sinus tarsi. It is a frequently associated injury in our present study, accounting for 25% of the cases. It might potentially cause sinus tarsi syndrome.
Talar fractures are rare, constituting <1% of all fractures, and between 3% and 6% of all foot fractures.[7,8] However, in our analysis, it accounts for 95% of all cases and is the most often related injury with subtalar dislocation. Consistent with findings from other studies,[8,9] we observed that conventional radiographs are only modestly sensitive in detecting fractures associated with subtalar dislocation and were inadequate in delineating the type and extent of the fracture. Despite conventional radiographs remaining a quick and easily available tool of investigation for traumatic subtalar dislocation, MDCT is essential in detecting occult fractures not visible on radiographs, evaluating fracture details (including size, location, displacement, and comminution) as well as assessing of the STJ, which may alter subsequent management. Merchan reported on a case series consisting of 39 patients with traumatic subtalar dislocations in 1992.[10] Radiographs were the primary and sole investigations in this case series. Fractures were identified in 64% of the cases, where malleoli, fifth metatarsal base, cuboid, and navicular tuberosity were the most often related fractures with subtalar dislocations, according to this case series. Talar fractures were only reported in 2 (5.1%) out of 39 patients. The reported rate of concurrent fractures in subtalar dislocations diagnosed only by conventional radiographs – particularly talar fractures – was significantly lower than when CT scans were employed in place of the previously published recent case series. This emphasizes how much more important CT is than radiography when managing traumatic subtalar dislocations.
Despite the relatively short mean follow-up period in our study, we observe a substantial incidence of post-traumatic peri-talar OA. All the patients with radiographic OA present with clinical symptoms or signs (100%), which is higher than the previously reported figures by Bibbo et al.[2] It is reasonable to postulate that our figures might be underestimated given a limited follow-up period.
Although there might be a possible association between fracture, mechanism of injury, and treatment on the development of post-traumatic OA, we did not prove any significant statistical association, which is likely related to the limited sample size.
CONCLUSION
Subtalar dislocation remains a relatively rare injury. Due to the strong association between foot and ankle fractures and a significant risk of developing symptomatic post-traumatic peri-talar OA, subtalar dislocation may result in considerable morbidity, necessitating a detailed radiological and orthopedic evaluation. Because occult fractures are frequently invisible on conventional radiographs, post-reduction MDCT is required. Furthermore, using MDCT to characterize the fracture pattern and injured subregions of specific bones may help predict potential complications and guide subsequent management. We postulated an increased risk of post-traumatic OA with fracture, high-energy mechanism of injury, as well as treated by open reduction and internal fixation; however, this requires further larger-scale study.
Ethical approval
The research/study was approved by the Central IRB, reference number CIRB-2024-088-5, dated 26 June 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Subtalar dislocation: Management and prognosis for an uncommon orthopaedic condition. Int Orthop. 2016;40:999-1007.
- [CrossRef] [PubMed] [Google Scholar]
- Injury characteristics and the clinical outcome of subtalar dislocations: A clinical and radiographic analysis of 25 cases. Foot Ankle Int. 2003;24:158-63.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated acute traumatic subtalar dislocations: Review of 13 cases at a mean follow-up of 6 years and literature review. J Foot Ankle Surg. 2017;56:201-7.
- [CrossRef] [PubMed] [Google Scholar]
- Sequelae of subtalar joint dislocations at two level 1 trauma centers: A case series and literature review. Foot Ankle Surg Tech Rep Cases. 2022;2:100217.
- [CrossRef] [Google Scholar]
- Fracture of the medial tubercle of the posterior process of the talus: Magnetic resonance imaging appearance with clinical follow-up. HSS J. 2009;5:161-4.
- [CrossRef] [PubMed] [Google Scholar]
- Management Options in Avascular Necrosis of Talus. Indian J Orthop. 2018;52:284-96.
- [CrossRef] [PubMed] [Google Scholar]
- Talar fractures and dislocations: A radiologist's guide to timely diagnosis and classification. Radiographics. 2015;35:765-79.
- [CrossRef] [PubMed] [Google Scholar]
- Ankle and foot injuries: Analysis of MDCT findings. AJR Am J Roentgenol. 2004;183:615-22.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of process fractures of the talus using computed tomography. J Orthop Trauma. 1994;8:332-7.
- [CrossRef] [PubMed] [Google Scholar]
- Subtalar dislocations: Long-term follow-up of 39 cases. Injury. 1992;23:97-100.
- [CrossRef] [PubMed] [Google Scholar]






