Translate this page into:
A Computed Tomographic Study of Vietnamese C1-C2 Morphology for Atlantoaxial Crew Fixation Techniques

*Corresponding author: Nguyen Minh Duc, MD Department of Radiology, Pham Ngoc Thach University of Medicine, Ho Chi Minh City 700000, Vietnam. bsnguyenminhduc@pnt.edu.vn
-
Received: ,
Accepted: ,
How to cite this article: Hung ND, Duc NM, Dung LV, Sy TV, Dung LT, Hue ND. A computed tomographic study of Vietnamese C1-C2 morphology for atlantoaxial crew fixation techniques. J Clin Imaging Sci 2020;10:63.
Abstract
Objectives:
This study aimed to define variations in radiological C1 and C2 measurements among Vietnamese subjects and to determine the feasibility of implementing C1-2 fixation techniques.
Material and Methods:
From October 2017 to April 2018, 120 patients underwent thin slide computed tomography (CT) scans of the cervical spine, in our hospital. Various dimensions of the C1 and C2 were analyzed, using axial and sagittal reconstructions of CT images. Differences in characteristics between the two sides and between sexes were investigated, using Student’s t-test, with significance at P < 0.05.
Results:
The mean anteroposterior dimension and the transverse width of the C1 lateral mass were 19.7 ± 2.1 mm and 12.2 ± 1.7 mm, respectively. The mean angles of the screw, directed to the maximal medial, lateral, cranial, and caudal directions, were 36.6 ± 2.8°, 28.2 ± 3.0°, 49.6 ± 4.1°, and 26.4 ± 5.5°, respectively. The average isthmus height, internal height, and pedicle width of the C2 were 5.8 ± 1.0 mm, 4.8 ± 1.3 mm, and 5.0 ± 1.3 mm, respectively. No significant differences were observed for any parameters, between the left and right side of the C1 or C2 or between the two sexes.
Conclusion:
This study revealed that the morphology of the C1 and C2 did not differ between genders in the studied subjects, but morphologic variations exist between Vietnamese subjects and other populations. Pre-operative anatomy evaluations based on CT data are essential be performed for screw placement and trajectory planning to avoid neurovascular complications and to enhance the treatment outcome.
Keywords
C1-C2 morphology
Anatomy
Computed tomography
Atlantoaxial screw
Fixation techniques
INTRODUCTION
Atlantoaxial instability has been treated using various fixation techniques, including the broad use of transarticular screw-based fixation, along the posterior elements of the C1-2, and screw-rod constructs, along the C1 lateral mass (LM) and C2 pedicle. According to the previous studies, damage to the vertebral artery (VA), the internal carotid artery branches, the C1, C2 roots, and spinal cord can be caused by these techniques.[1,2] The rate of VA injury and incidence of malpositioned screws are higher when using transarticular screws than when using screw-rod constructs (VA injury: 4.1% vs. 2.0%; malpositioned screws: 7.1% vs. 2.4%).[3] A high-riding VA and a narrow C2 pedicle are anatomic variations that have been associated with VA injury.[1] In addition, the height, length, width, and angle of the C1 LM can play an important role in proper screw placement.[4] Therefore, understanding the potential anatomic variations of the C1 and C2 are crucial for choosing an appropriate screw and avoiding undesirable surgical injuries.
Wide anatomical variations in the C1-C2 region have been reported by cadaveric studies. Wang and Samudrala[5] analyzed the morphometric characteristics of the C1 in 74 cadaveric spines. The study suggested that LM screw fixation was a highly effective technique, despite significant variations in the C1 morphology. However, high-resolution computed tomography (CT) scans have been used by many authors to evaluate the morphometric dimensions of the C1 and C2.[6,7] Yeom et al.[8] used 1 mm slices from CT scans to assess the anatomy of the C2, on sagittal and axial images. Their study indicated that 82% of patients with narrow pedicles had a coincident high-riding VA, whereas only 54% high-riding VAs coexisted with a narrow pedicle.
Although some aforementioned CT-based and cadaveric studies have determined C1 and C2 morphometric characteristics to determine the practicability of the C1-2 fixation techniques, none of these studies have included a Vietnamese population. Therefore, this study aimed to determine the differences in the radiological C1 and C2 measurements among Vietnamese subjects and to provide additional information for pre-operative decision-making.
MATERIAL AND METHODS
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The research in this study was approved by the Institutional Review Board.
A total of 192 cervical spinal CT scans, from the petrous apex to the first thoracic vertebra, were obtained, from October 2017 to April 2018, in Viet Duc Hospital, Hanoi, Vietnam. The raw image data set, reconstructed in the axial, coronal, and sagittal planes, was used, with a section thickness of 0.625 mm in the bone algorithm. CT images from patients younger than 18 years and those from patients with trauma, tumor, infections, congenital malformations, surgical histories associated with the upper cervical spine, and scans exposing metallic artifacts were excluded from the analysis. Consequently, 72 scans were dismissed, based on exclusion criteria, and the remaining 120 patients were included in the study.
Routine axial and sagittal reconstructions in the bone algorithm were utilized for measurements. The axial plane (1 mm thick) was included in the orthogonal horizontal slice. The sagittal plane (3 mm thick) was vertical to the coronal plane (CP) of the body.
The length of the C1 LM, or the screw length (SL), was defined in the axial plane as the longest anteroposterior (AP) axis, including the outer cortex (OC) of the posterior and anterior wall [Figure 1a]. The transverse width (TW) of C1 LM was also defined in the axial plane, as the lateromedial axis perpendicularly to the AP axis [Figure 1a]. The maximal medial angle (MA) of the screw (AOS) was defined as the angle between a line drawn through the middle of the LM, parallel to the midline, and a line drawn anteromedially to the most medial position of the anterior LM wall, in the axial plane [Figure 1b]. The maxima lateral AOS was defined as the angle between a line drawn through the middle of the LM, parallel to the midline, and a line drawn anterolaterally to the most lateral position of the anterior LM wall, in the axial plane [Figure 1c]. The maximal cranial AOS was defined as the angle between a line drawn through the middle of the LM, parallel to the horizontal plane, and a line drawn anterosuperiorly to the most superior position of the anterior LM wall, the CP [Figure 1d]. The maximal caudal AOS was defined as the angle between a line drawn through the middle of the LM, parallel to the horizontal plane, and a line drawn anteroinferiorly to the most inferior position of the anterior LM wall in the CP [Figure 1e].
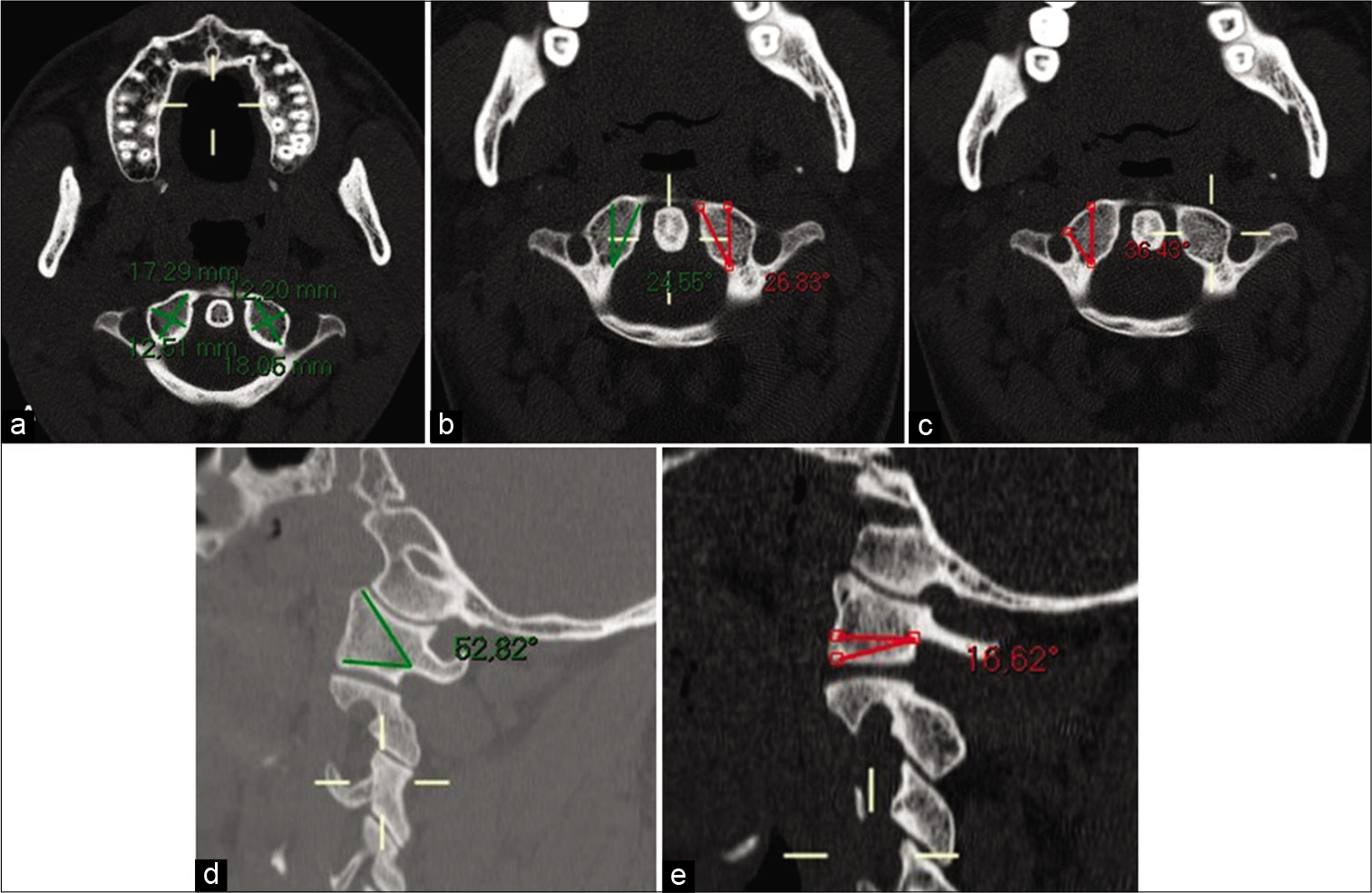
- The length of C1 lateral mass or the screw length of a 39-year-old male. An axial slice (a) shows the length and the transverse width of C1 lateral mass, (b) the AOS directed to maximal medial, (c) the AOS directed to maximal lateral. A sagittal reformation slice (d) shows the AOS directed to maximal cranial, (e) the AOS directed to maximal caudal.
The isthmus height (ISH) and the internal height (INH) of the C2 were calculated using the most paracenter slide, from the sagittal to lateral walls of the spinal canal (SC) (3 mm from the lateral wall of the SC). The measurement was performed from the dome of the VA groove to the OC of the superior facet [Figures 2a and b]. The width of the C2 pedicle was measured at those sites where the lateral cortical boundary of the pedicle could be distinctly observed on axial images [Figure 2c].
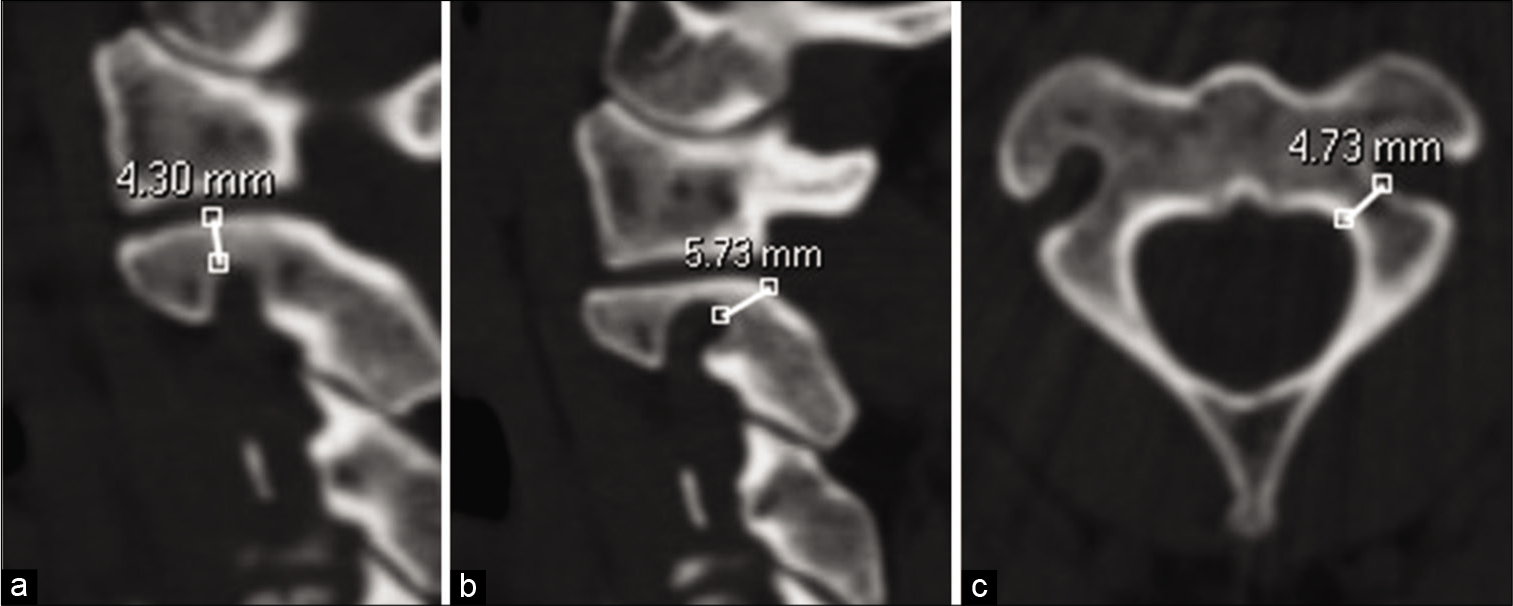
- The isthmus height and the internal height of C2 of a 39-year-old male. A sagittal reformation slice (a) shows the internal height of lateral mass and (b) the isthmus height of the C2. An axial slice (c) shows the width of C2 pedicle.
SPSS, ver. 22, was used to analyze all data (IBM Corp., New York, USA). The means and standard deviations of the C1 and C2 measurements were assessed. The Student’s t-test was used to determine differences between the left and right sides of the C1 and C2 dimensions and between male and female subjects. Correlations among the various dimensions were also determined. Significance was determined at P < 0.05.
RESULTS
Overall, 120 cervical spinal CT scans that fulfilled the selection criteria were analyzed, including 97 males and 23 females, aged between 18 and 86 years.
The characteristics of the C1 LM, ISH, INH, and axis pedicle width (PW) of the C2 are presented as the mean and standard deviation, in Tables 1-3. No significant differences were found for the dimensions of the C1 and C2 between the two sides or between males and females, according to comparisons using Student’s t-test (P > 0.05).
| Sex | AP dimension (mm) | Transverse width (mm) | ||
|---|---|---|---|---|
| Right | Left | Right | Left | |
| Male (n=97) | 19.6±2.0 (16.7–24.1) | 19.7±2.1 (16.5–25.6) | 12.2±1.6 (7.0–14.8) | 12.3±1.7 (7.7–15.1) |
| Female (n=23) | 19.6±2.6 (16.8–25.0) | 19.8±2.5 (16.5–25.8) | 11.5±2.0 (6.9–14.5) | 11.9±1.7 (7.6–14.5) |
| P(male vs. females) | 0.954 | 0.826 | 0.107 | 0.269 |
| Both sexes | 19.6±2.1 (16.7–25.0) | 19.7±2.2 (16.5–25.8) | 12.1±1.7 (6.9–14.8) | 12.2±1.7 (7.6–15.1) |
| 19.7±2.1 (16.5–25.8) | 12.2±1.7 (6.9–15.1) | |||
Values are presented as mean±standard deviation (min-max)
| Sex | The angle of the screw directed to maximal medial | The angle of the screw directed to maximal lateral | The angle of the screw directed to maximal cranial | The angle of the scredirected to maximacaudal | ||||
|---|---|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | Right | Left | |
| Male (n=97) | 36.9±2.9 (29.0–47.0) | 36.6±2.6 (29.0–42.0) | 28.2±3.0 (20.0–37.0) | 28.0±3.0 (19.0–35.0) | 49.6±4.0 (38.0–58.0) | 49.6±4.0 (38.0–59.0) | 27.0±5.6 (16.0–40.0) | 25.8±5(16.0–50 |
| Female (n=23) | 35.7±3.0 (30.0–40.0) | 36.5±3.0 (31.0–45.0) | 29.1±2.2 (25.0–34.0) | 27.9±3.3 (21.0–33.0) | 50.0±4.6 (38.0–58.0) | 49.7±4.2 (35.0–56.0) | 27.0±5.5 (17.0–38.0) | 25.8±5(18.0–37 |
| P(male vs. females) | 0.106 | 0.907 | 0.081 | 0.882 | 0.720 | 0.939 | 0.961 | 0.972 |
| Both sexes | 36.7±2.9 | 36.5±2.7 | 28.3±2.8 | 28.0±3.0 | 49.7±4.2 | 49.6±4.0 | 27.0±5.6 | 25.8±5 |
| 36.6±2.8 (29.0–47.0) | 28.2±3.0 (19.0–37.0) | 49.6±4.1 (35.0–59.0) | 26.4±5.5 (16.0–50.0) | |||||
Values are presented as mean±standard deviation (min-max)
| Sex | Isthmus height (mm) | Internal height (mm) | Pedicle width (mm) | |||
|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | |
| Male | 5.7±0.9 (2.5–7.9) | 5.7±1.1 (1.2–8.3) | 4.8±1.1 (1.7–9.9) | 4.6±1.2 (1.3–9.5) | 4.9±1.4 (0.4–9.7) | 5.1±1.3 (1.1–9.2) |
| Female | 6.0±0.9 (3.9–7.2) | 5.9±1.1 (2.3–7.2) | 5.3±1.9 (0.8–8.6) | 5.1±1.5 (2.3–8.8) | 5.4±0.8 (3.7–6.8) | 5.1±1.3 (1.6±6.6) |
| P(male vs. females) | 0.159 | 0.588 | 0.197 | 0.119 | 0.059 | 0.902 |
| Both sexes | 5.8±0.9 (2.5–7.9) | 5.7±1.1 (1.2–8.3) | 4.9±1.3 (0.8–9.9) | 4.7±1.3 (1.3–9.5) | 5.0±1.3 (0.4–9.7) | 5.1±1.3 (1.1–9.2) |
| 5.8±1.0 (1.2–8.3) | 4.8±1.3 (0.8–9.9) | 5.0±1.3 (0.4–9.7) | ||||
Values are presented as mean±standard deviation (min-max)
The maximal SL of the C1 LM necessary to achieve bicortical purchase in all studied subjects was 25.8 mm, and the minimal SL was 16.5 mm [Table 1]. The TW of the C1 LM averaged 12.2 mm, with a minimum of 6.9 mm and a maximum of 15.1 mm [Table 1].
The mean maximum screw medialization across all subjects was 36.6° (ranging from 29° to 47°). The mean maximum screw lateralization was 28.2° (ranging from 19° to 37°). The mean maximum superiorly directed angle was 49.6° (ranging from 35° to 59°). The mean maximum inferiorly directed angle was 26.4° [ranging from 16° to 50°, Table 2].
For the dimensions of the C2 in the studied population, the mean ISH was 5.8 mm (ranging from 1.2 mm to 8.3 mm). The mean INH was 4.8 mm (ranging from 0.8 mm to 9.9 mm). The mean PW was 5.0 mm [ranging from 0.4 mm to 9.7 mm, Table 3].
According to the descriptions by Bloch et al.[9] and Neo et al.,[10] for the detection of a high-riding VA (ISH ≤5 mm and/ or INH ≤2 mm on the sagittal image), 33 high-riding VAs (13.8%) were diagnosed, and 43 (17.9%) narrow pedicles (axis PW ≤4 mm) were detected, relative to the diameters of widely used screws, which are 3.5 mm and 4.0 mm.
DISCUSSION
The C1-C2 fixation techniques aim to enhance the stabilization of the spinal column, protect the spinal cord, and reduce neural tissue compression and deformity. Although these screw fixation techniques have been widely used, anatomic variations, VA anomalies, and the proximity of the vertebrae proximity to the spinal cord and nerve plexuses can result in negative outcomes. Therefore, detailed anatomical knowledge can be critical for choosing the optimal screws and assessing the best entry point and trajectory for the screw. Several cadaveric and radiographic studies examining C1 and C2 morphology have been published in recent years,[7,11-13] most of which have recommended the performance of pre-operative CT scans to choose the best surgical techniques.
The AP dimensions of the C1 LM are usually used to determine the SL and were found to have mean values of 19.6 ± 2.1 mm, on the right side, and 19.7 ± 2.2 mm, on the left side, in our study. Our results were comparable to the values reported in American subjects, by Christensen et al.[4] (19.73 ± 1.71 mm), and in a Turkish population, by Sengul et al.[14] (19.2 ± 3.4 mm). In contrast, the values in the present study were lower than those reported by Patel and Gupta[13] for both sides (20.73 ± 1.68 mm for the right side and 20.86 ± 1.97 for the left side). The mean TW values for the C1 LM in our study were 12.1 ± 1.7 mm and 12.2 ± 1.7 mm, for the right and left sides, respectively, which were higher than the values in several previous reports. According to an anatomical study on the dried, intact human atlas reported by Patel and Gupta,[13] this dimension was 11.34 ± 1.82 mm, for the right side, and 11.39 ± 1.5 mm, for the left side, whereas the values reported in a study by Gosavi and Vatsalaswamy[12] were 10.36 ± 1.72 mm and 10.47 ± 1.61 mm, respectively.
According to a literature review, in addition to potential VA injury, possible C1-2 LM screw fixation complications include SC or atlantooccipital joint penetration and occipital neuralgia, due to C2 root retraction and injury.[1,7] Therefore, screw trajectory planning is an important factor that must be determined preoperatively. In this study, the maximal MA was calculated as 36.7 ± 2.9°, on the right side, and 36.5 ± 2.7°, on the left side. The study by Carvalho et al.[11] reported similar angle parameters, as 36.99 ± 5.25° and 36.20 ± 5.07°, on the right and the left sides, respectively. Simsek et al.[15] stated that the optimal MA was 13.5 ± 1.9° and the maximal MA was 29.4 ± 3.0°. Some studies have suggested that the medial trajectory should not be greater than 30°, to avoid penetrating the SC.[7,15] The mean maximal lateral AOS values were similar between the right and left sides, at 28.3 ± 2.8° and 28.3 ± 3.0°, respectively, in our study. This result was higher than the angles determined in the study by Akay et al.[7] (24.5° and 22.7° on the right and left sides, respectively). These numbers were even greater than those reported by Wang and Samudrala[5] and Chamoun et al.[16] (13° and 17°, respectively). The maximum superior angles have been reported as 29.6 ± 2.6°, by Simsek et al.,[15] 33.73 ± 6.30°, by Carvalho et al.,[11] and 19 ± 5°, by Wang and Samudrala[5] Our measurement was larger than those in the previous studies, calculated as 49.7 ± 4.2°, on the right side, and 49.6 ± 4.0°, on the left side. The maximal cranial angle was calculated as 23.63 ± 5.25°, for the right side, and 22.99 ± 5.62°, for the left side, by Carvalho et al.[11] In contrast, Akay et al.[7] defined the cranial angulation between 10° and 47°. In the current study, a similar angulation was identified, as 27.0 ± 5.6°, on the right side, and 25.8 ± 5.3°, on the left side.
According to several studies, one complication associated with C1-2 transarticular screw fixation and C2 pedicle screws were VA injury.[1,8] In a simulation study, using CT scans and 3D screw trajectory software, Yeom et al.[8] found that the rate of VA injury was 9.5% for transarticular screw fixation and 8.0% for pedicle screws. Yoshida et al.[17] mentioned that these two techniques had similar anatomic risks for VA injury. Therefore, most authors have emphasized the important role played by CT scans during the pre-operative evaluation, to prevent iatrogenic VA injury.[1,8,17] The mean ISH was 5.8 mm and the mean INH was 4.8 mm, in the present study, which were lower than those reported by Wajanavisit et al.[1] (10.18 mm and 5.61 mm, respectively) and Vanek et al.[18] (8.0 mm and 6.4 mm, respectively). Moreover, the incidence of a high-riding VA has been investigated by several cadaveric and radiographic studies.[1,8,19] The prevalence of a high-riding VA in the present study was 13.8%, which was lower than most results reported by the previous studies. Chamoun et al.,[16] using three-dimensional CT angiography to analyze 100 surgical cases, reported a rate of high-riding VA of 31%. High-riding VA prevalence was reported as 16.5% in the study by Wajanavisit et al.[1] who applied a novel CT reconstruction technique. These disagreements could be explained by differences in technique and by racial differences.
The present study found that the C2 pedicle had a mean width of 5.0 ± 1.3 mm, on the right side, and 5.1 ± 1.3 mm, on the left side, which are lower values than those reported by several previous studies. The C2 pedicle width was reported by Singla et al.[20] as 10.07 mm and by Gosavi and Vatsalaswamy[12] as 7.7 mm, among the Indian population, and by Sengul et al.[14] as 9.5 mm, among the Turkish population. However, the study by Wajanavisit et al.[1] reported a finding similar to that for the current study, of 5.07 mm. The rate of narrow pedicles in the previous studies ranged from 9.5% to 32%.[1,8] In this study, we found that 17.9% of C2 pedicles had widths ≤4 mm. Yeom et al.[8] stated that the cranial portion of the C2 pedicle may be much wider than the caudal portion, which was well evaluated on 3D reconstructed images. Therefore, the use of axial images alone could be misleading when predicting the outcomes of pedicle screw installations.
Our study was limited by a small sample size from a single center, which may not be representative of all ethnic groups in Vietnam. A single observer took all measurements in this study, which was another weakness. Therefore, future studies using larger sample sizes and more observers will likely provide more accurate results.
CONCLUSION
Our data indicated that the C1 and C2 morphology did not differ between genders in the studied subjects; however, the results of this study confirmed the presence of morphologic variations for the C1 and C2 between the Vietnamese population and other populations. Furthermore, a small number of cases exist for which current screw fixation techniques may not be feasible. Therefore, pre-operative CT scans are indispensable for improving the accuracy of screw placement and avoiding neurovascular injuries.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Declaration of patient consent
Institutional Review Board permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Prevalence of high-riding vertebral artery and morphometry of C2 pedicles using a novel computed tomography reconstruction technique. Asian Spine J. 2016;10:1141-8.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior atlanto-axial fixation with polyaxial C1 lateral mass screws and C2 pars screws. Acta Neurochir (Wien). 2009;151:223-9.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome comparison of atlantoaxial fusion with transarticular screws and screw-rod constructs: Meta-analysis and review of literature. J Spinal Disord Tech. 2014;27:11-28.
- [CrossRef] [Google Scholar]
- C1 anatomy and dimensions relative to lateral mass screw placement. Spine (Phila Pa 1976). 2007;32:844-8.
- [CrossRef] [PubMed] [Google Scholar]
- Cadaveric morphometric analysis for atlantal lateral mass screw placement. Neurosurgery. 2004;54:1436-9.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic study for ideal and safe posterior C1-C2 transarticular screw fixation. Spine (Phila Pa 1976). 1998;23:1703-7.
- [CrossRef] [PubMed] [Google Scholar]
- An anatomical and radiological study for C1 lateral mass screw fixation. J Neurol Sci (Turk). 2013;30:328-36.
- [Google Scholar]
- Risk of vertebral artery injury: Comparison between C1-C2 transarticular and C2 pedicle screws. Spinal J. 2013;13:775-85.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of frameless stereotaxy on the accuracy of C1-2 transarticular screw placement. J Neurosurg. 2001;95:74-9.
- [CrossRef] [PubMed] [Google Scholar]
- Atlantoaxial transarticular screw fixation for a high-riding vertebral artery. Spine (Phila Pa 1976). 2003;28:666-70.
- [CrossRef] [Google Scholar]
- Estudo tomográfico do atlas relacionado com a inserção de implantes na massa lateral. Acta Ortop Bras. 2009;17:136-8.
- [CrossRef] [Google Scholar]
- Morphometric study of the atlas vertebra using manual method. Malays Orthop J. 2012;6:18-20.
- [CrossRef] [PubMed] [Google Scholar]
- A morphometric study of adult human atlas vertebrae in South Gujarat population, India. Int J Res Med Sci. 2016;4:4380-6.
- [CrossRef] [Google Scholar]
- Morphometric anatomy of the atlas and axis vertebrae. Turk Neurosurg. 2006;16:69-76.
- [Google Scholar]
- Ideal screw entry point and projection angles for posterior lateral mass fixation of the atlas: An anatomical study. Eur Spine J. 2009;18:1321-5.
- [CrossRef] [PubMed] [Google Scholar]
- Computed tomography morphometric analysis for C-1 lateral mass screw placement in children. Clinical article. J Neurosurg Pediatr. 2009;3:20-3.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the anatomical risk for vertebral artery injury associated with the C2-pedicle screw and atlantoaxial transarticular screw. Spine (Phila Pa 1976). 2006;31:E513-7.
- [CrossRef] [PubMed] [Google Scholar]
- Vertebral artery and osseous anomalies characteristic at the craniocervical junction diagnosed by CT and 3D CT angiography in normal Czech population: Analysis of 511 consecutive patients. Neurosurg Rev. 2017;40:369-76.
- [CrossRef] [PubMed] [Google Scholar]
- Morphologic considerations of C2 isthmus dimensions for the placement of transarticular screws. Spine (Phila Pa 1976). 2000;25:1542-7.
- [CrossRef] [PubMed] [Google Scholar]
- Morphometric analysis of axis and its clinical significance-an anatomical study of Indian human axis vertebrae. J Clin Diagn Res. 2015;9:AC4-9.
- [CrossRef] [PubMed] [Google Scholar]







