Translate this page into:
A comparison of balloon-assisted versus dilator in percutaneous gastrostomy tube placement

*Corresponding author: Nabeel M. Akhter, Department of Radiology and Nuclear Medicine, Mercy Medical Center, Baltimore, Maryland, United States. nakhter@mdmercy.com
-
Received: ,
Accepted: ,
How to cite this article: Lee S, Ghosh A, Raymond A, Akhter NM. A comparison of balloon-assisted versus dilator in percutaneous gastrostomy tube placement. J Clin Imaging Sci 2023;13:25.
Abstract
Objectives:
This study assesses the safety and efficacy of balloon-assisted gastrostomy (BAG) compared to conventional techniques using dilators.
Material and Methods:
A single-center retrospective review of all fluoroscopically-guided percutaneous gastrostomy tube insertions from July 2017 to September 2020 was performed. Two hundred and seventy-three patients were included in this study, with 183 patients and 90 patients in the BAG and dilator groups, respectively. Fluoroscopy time, peak radiation dose, pain management, days to interventional radiology (IR) reconsultation, and post-operative complications (major and minor) for each procedure were reviewed to evaluate for statistical differences.
Results:
There were shorter fluoroscopy times (5.13 min vs. 7.05 min, P = 0.059) and a significantly lower radiation use (Avg = 102.13 mGy vs. 146.98 mGy, P < 0.05) in the BAG group. The BAG group required significantly lower operating time (41 min vs. 48 min, P < 0.01) and received lower pain management (fentanyl 75 mcg and midazolam 1.5 mg, P < 0.001). The mean days to IR reconsultation for the BAG group was greater (29 days vs. 26 days, P = 0.38). The overall rate of minor complications (grades 1 and 2, according to the CIRSE classification system) was higher in the dilator group (39% vs. 35% in BAG group, P = 0.53). No major complications were reported in either group.
Conclusion:
BAG is a safe and efficient technique for percutaneous gastrostomy tube placement. BAG patients required significantly lesser radiation, OR time, post-operative pain management, and recorded lower postoperative complications compared to their counterparts in gastrostomies utilizing dilators.
Keywords
Gastrostomy tubes
Balloon-assisted gastrostomy
Percutaneous gastrostomy
Enteral nutrition
INTRODUCTION
Gastrostomy tubes (G-tubes) are indispensable medical devices employed for enteral access in patients unable to maintain adequate nutrition or receive necessary medications orally. These tubes are typically inserted into the stomach through the abdominal wall using surgical, endoscopic, or percutaneous techniques.[1-3] Percutaneous G-tubes (PEG-tubes) represent a notable advancement in terms of patient comfort and esthetic appeal compared to traditional tube-style devices.[1,4] Among the different types of PEG tubes available, the balloon and dilator variants have emerged as prominent options, each with its distinct set of advantages and considerations.[1,5,6] Balloon-based devices secure their position within the gastric lumen using an inflatable balloon, while dilators encompass a range of rigid or flexible plastic designs.[2,3]
This study aims to investigate and compare the efficacy and safety of balloon and non-balloon gastrostomy devices in the context of fluoroscopy time, radiation dose, analgesic requirements, and post-operative complications. A comprehensive understanding of their respective advantages/disadvantages, as well as general clinical and technical considerations involved, holds paramount importance for interventionalists. By elucidating the nuances of these procedures, we can enhance patient outcomes and optimize the use of radiographic PEG tubes in clinical practice.
MATERIAL AND METHODS
Patient demographics
A single-center retrospective review of all fluoroscopically guided PEG-tube insertions from July 2017 to September 2020 was performed. Two hundred and seventy-three patients were included in this study, with 183 patients and 90 patients in the balloon-assisted gastrostomy (BAG) and dilator groups, respectively. The majority of G-tube referrals in our institution are due to neuromotor impairment (55.9% of the study population). These patients were retrospectively reviewed within two groups: BAG approach (183 patients, mean age 63.1 ± 13.78, median age 64 [interquartile range [IQR] = 16]) and dilator approach (90 patients, mean age 62.5 ± 13.79, median age 64 [IQR = 18]).
Data collection
This retrospective study, which was performed under clinical study guidelines, was approved by the Institutional Review Board (IRB) and determined to be IRB-exempt. The demographic information and radiation-related data were collected based on electronic medical records. Fluoroscopy time, peak radiation dose, pain management, days to interventional radiology (IR) reconsultation, and post-operative complications (major and minor) for each procedure were reviewed to evaluate for statistical differences.
Percutaneous gastric tube placement
For image-guided percutaneous placement, two groups of patients were created based on the method of tract dilatation: BAG and dilator. The procedural selection was based on the individual preferences of seven highly experienced interventional radiologists, all of whom had served as faculty members in a tertiary care hospital for varying durations, ranging from 2 to over 20 years. Importantly, each operator demonstrated equal proficiency in both balloon and dilator percutaneous gastrostomy procedures, ensuring consistency, and eliminating potential bias due to variations in training. The choice of insertion technique was solely determined by the operator’s personal preference, allowing for a comprehensive evaluation of the two methods within the study cohort.
The percutaneous placement of G-tubes is a minimally invasive procedure performed under local anesthesia and conscious sedation. Before the procedure, the abdominal region is prepared using standard sterile techniques. To ensure patient comfort, intravenous midazolam and fentanyl citrate are administered for sedation and analgesia. Under the guidance of the operator, the stomach is gently inflated with air through an existing nasogastric tube. Once the stomach is adequately distended and the optimal access site is determined, a gastropexy procedure is employed, involving the placement of three T-bar fasteners (Avanos Medical; Georgia, US) around the selected percutaneous access point. A small incision, approximately 3–4 mm in size, is carefully made at the center of the gastropexy fasteners, allowing access to the stomach. With fluoroscopic guidance, an 18-gauge needle is introduced through the abdominal wall, and a meticulously positioned stiff guide wire is slowly advanced. This step-by-step approach ensures precise wire placement. At this stage, the decision between the BAG and dilator method determines the subsequent tract dilatation technique used for the G-tube insertion.
Balloon gastric tube approach
In the BAG approach, tract dilation is accomplished using a Mustang balloon [Figure 1] (Boston Scientific; Washington, D.C., US), which is inflated to expand the gastric pathway. Following successful tract dilatation, a 16-French G-tube is gently advanced into the stomach, ensuring proper positioning. To secure the tube and establish a stable connection with the gastric wall, the intraluminal balloon of the gastrostomy catheter is filled with sterile water. The correct placement is confirmed by encountering resistance when retracting the catheter, indicating the optimal positioning within the gastrointestinal tract.
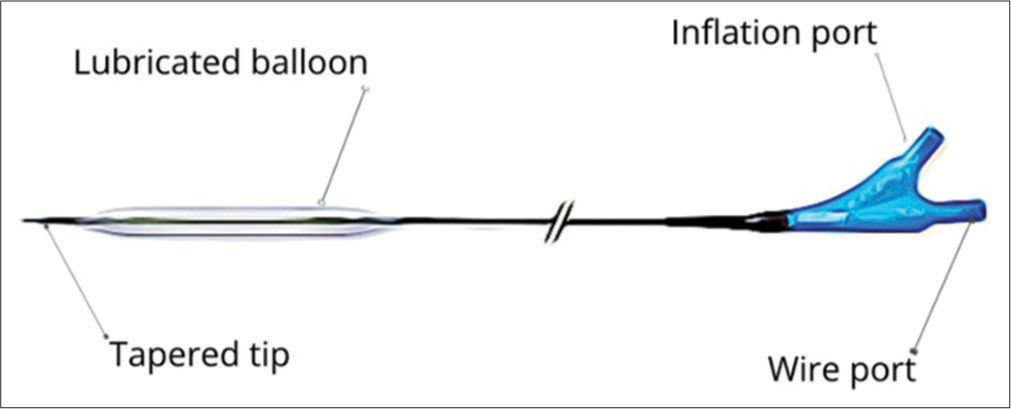
- Balloon dilator features a tapered tip for enhanced navigation, an easy-to-access inflation port for precise control, and a durable silicone balloon.
Dilator gastric tube approach
The dilator group employed a sequential telescoping dilator system (Avanos Medical; Georgia, US) [Figure 2] accompanied by an introducer sheath to progressively widen the gastrostomy tract. Subsequently, a G-tube was carefully inserted through the sheath and positioned within the stomach. Following tube placement, the sheath was removed, and the retention balloon was inflated using sterile water. To accommodate any potential post-procedural abdominal wall swelling, the plastic disk of the gastropexy retention sutures was securely maintained in position and anchored to the suture. In the event of significant discomfort, the retention sutures can be selectively released while ensuring continued stability of the catheter by the retention balloon.

- The serial dilator incorporates a telescoping design along with a convenient peel-away sheath.
Post-procedure discharge
Data were collected on the technical outcomes, procedural issues, and post-operative catheter-related complications. Repeat evaluation of the access site was performed for all patients before discharge. The follow-up appointment was made based on a future management plan.
Statistical analysis
To evaluate the differences, the data regarding procedure time (min), fluoroscopy time (min), radiation dose (mGy Peak Skin Dose), pain management (Fentanyl in mcg and Midazolam in mg), IR reconsultation (days), and post-operative complications (major and minor) were collected for both groups. The outcomes of the treatment groups were analyzed using t-test, Wilcoxon rank test, and chi-square test, as appropriate. P < 0.05 was considered statistically significant. All results of this study were analyzed using appropriate statistical software (SPSS Statistics 26.0, IBM Inc).
RESULTS
This study noted a total of 273 patients with 183 patients in the balloon group and 90 patients in the dilator group [Table 1]. There were no significant differences in terms of age between the two groups (P > 0.05 for over and under 65 y/o). The median age of patients was 63 years (IQR = 16) in the balloon group, and 62 years (IQR = 18) in the dilator group [Table 1].
| Variable | Overall (n=273) | Balloon (n=183) | Dilator (n=90) |
|---|---|---|---|
| Patient Age (years) | 63.11 [56.50, 73] | 63.43 [57, 73] | 62.47 [55, 73.25] |
| BMI | 26.6 (7.7) | 26.7 (7.7) | 26.3 (7.7) |
| Sex | |||
| Male | 198 (72.5) | 132 (72.1) | 66 (73.3) |
| Female | 75 (27.5) | 51 (27.9) | 24 (26.7) |
Data presented as mean (SD), median [IQR], or frequency (%)
Among the meta-indications of the study population, neuromotor impairment was the most common (n = 152, 55.9%) in both balloon and dilator groups [Table 2]. Similarly, head/neck cancer was the second most common disease etiology observed in all patients (n = 47, 17.3%), followed by gastric outlet issues (n = 8, 2.9%), and inadequate PO intake (n = 16, 5.9%) [Table 2]. Patients in the balloon group had a higher incidence of facial trauma (n = 4, 2.2%) and inadequate oral intake (n = 4, 2.2%) compared to the dilator group, while the dilator group had a higher incidence of proximal obstruction (n = 5, 5.6%) compared to balloon group [Table 2].
| Variable | Overall (n=273) | Balloon (n=183) | Dilator (n=90) |
|---|---|---|---|
| Facial trauma | 4 (1.5) | 4 (2.2) | 0 |
| Failure to thrive 2/2 CHF | 1 (0.4) | 1 (0.5) | 0 |
| Gastric outlet issue | 8 (2.9) | 4 (2.2) | 4 (4.4) |
| Gastroparesis | 1 (0.4) | 0 | 1 (1.1) |
| Head/neck cancer | 47 (17.3) | 32 (17.6) | 15 (16.7) |
| Inadequate oral intake | 5 (1.8) | 4 (2.2) | 1 (1.1) |
| Inadequate PO intake | 16 (5.9) | 12 (6.6) | 4 (4.4) |
| Neuro-motor impairment | 152 (55.9) | 104 (57.1) | 48 (53.3) |
| Proximal obstruction | 9 (3.3) | 4 (2.2) | 5 (5.6) |
| Trach | 24 (8.8) | 14 (7.7) | 10 (11.1) |
| Venting G-tube | 5 (1.8) | 3 (1.6) | 2 (2.2 |
The major demographic variables of the patients are presented in [Table 1], showcasing a mean body mass index (BMI) of 26.6 for the overall sample. The balloon group had a significantly higher BMI than the dilator group [Table 1]. Fluoroscopy time was automatically calculated by the computer based on real exposure to X-ray during percutaneous gastrostomy placement. There were significantly shorter fluoroscopy times (Avg = 5.13 min vs. 7.05 min, P = 0.059) in the balloon group than in the dilator group [Table 3]. Accordingly, there was a trend toward significantly lower radiation exposure dose (mGy PSD) in the balloon group than in the dilator group (Avg = 102.13 mGy vs. 146.98 mGy, P < 0.05) [Table 3]. The BAG group required significantly lower operating time (41 min vs. 48 min, P < 0.01) and received significantly lower pre-operative sedation in the form of fentanyl (81.7 mcg vs. 116.2 mcg, P < 0.05) [Table 4]. Versed (1.5 mg vs. 1.8 mg, P < 0.326) was also lower in the BAG group, although insignificant [Table 4].
| Outcome | Overall (n=273) | Balloon (n=183) | Dilator (n=90) | P value |
|---|---|---|---|---|
| Fluoroscopy time (min) | 5.8 (7.5) | 5.1 (4.6) | 7.1 (11.1) | 0.045* |
| Radiation dose (mGy) | 116.9 (189.4) | 102.1 (184.6) | 147.0 (196.2) | 0.066* |
| In room time (min) | 43.8 (23.8) | 41.4 (23.3) | 48.6 (24.3) | 0.018* |
| Outcome | Overall (n=273) | Balloon (n=183) | Dilator (n=90) | P value |
|---|---|---|---|---|
| Versed (mg) | 1.6 (2.1) | 1.5 (2.3) | 1.8 (1.6) | 0.326* |
| Fentanyl (mcg) | 93.0 (99.4) | 81.7 (80.7) | 116.2 (127.0) | 0.007* |
No major complications were observed in either group [Table 5]. However, a total of 106 patients (38.8%) experienced minor complications, classified as CIRSE grades 1 and 2[7] [Table 5]. These complications included dislodgement, leakage, clogged tube, infection, pain, bleeding, and pneumoperitoneum. The overall rate of minor complications was higher in the BAG group; however, it did not reach statistical significance (39.9% vs. 36.7%, P = 0.61) [Table 5]. G-tube insertion was successful in 99.6% of the patient population with one failure in which the operator was unable to access gastrojejunostomy with BAG method but returned 2 days later for successful revision. In terms of specific complications, 22 patients from the BAG group were referred for dislodgement compared to six from the dilator group. Clogged G-tubes occurred at similar frequencies (4.4%) [Table 5]. The infection rate was significantly higher in the dilator group compared to the BAG group, (7.8% vs. 2.2%, P = 0.03) [Table 5]. Pain associated with gastrostomy placement was reported in 32 patients in the BAG group compared to 11 patients in the dilator group [Table 5]. Catheter leakage was reported in six patients from the BAG group, whereas three patients from the dilator group experienced this issue [Table 5]. Bleeding occurred in five patients from the dilator group, while six cases were observed in the BAG group [Table 5]. Six patients, three from each group, experienced pneumoperitoneum [Table 5].
| Outcome | Overall (n=273) | Balloon (n=183) | Dilator (n=90) | P value |
|---|---|---|---|---|
| Major Complications | ||||
| None | 273 (100.0) | 100 (100.0) | 100 (100.0) | |
| Any of Minor Complication | 0.608* | |||
| Yes | 106 (38.8) | 73 (39.9) | 33 (36.7) | |
| No | 167 (61.2) | 110 (60.1) | 57 (63.3) | |
| Dislodged | 0.170* | |||
| Yes | 28 (10.3) | 22 (12.0) | 6 (6.7) | |
| No | 245 (89.7) | 161 (88.0) | 84 (93.3) | |
| Clogged | 0.978* | |||
| Yes | 12 (4.4) | 8 (4.4) | 4 (4.4) | |
| No | 261 (95.6) | 175 (95.6) | 86 (95.6) | |
| Infection | 0.027* | |||
| Yes | 11 (4.0) | 4 (2.2) | 7 (7.8) | |
| No | 262 (96.0) | 179 (97.8) | 83 992.2) | |
| Pain | 0.262* | |||
| Yes | 43 (15.8) | 32 (17.5) | 11 (12.2) | |
| No | 230 (84.2) | 151 (82.5) | 79 (87.8) | |
| Leakage | 0.981* | |||
| Yes | 9 (3.3) | 6 (3.3) | 3 (3.3) | |
| No | 264 (96.7) | 177 (96.7) | 87 (96.7) | |
| Bleeding | 0.368* | |||
| Yes | 11 (4.0) | 6 (3.3) | 5 (5.6) | |
| No | 262 (96.0) | 177 (96.7) | 85 (94.4) | |
| Pneumoperitoneum | 0.369* | |||
| Yes | 6 (2.2) | 3 (1.6) | 3 (3.3) | |
| No | 267 (97.8) | 180 (98.4) | 87 (96.7) |
Data presented as frequency (%). P values calculated by t-test, Wilcoxon rank test and Chi-square test were appropriate.
DISCUSSION
Much of the research conducted on radiologically guided PEG-tube insertion have reported its superior safety and efficacy, with studies emphasizing its lower complication rate when compared to endoscopic or surgical techniques.[1,8,9] Relatively few studies have compared the performance and outcomes of BAG versus dilators techniques. The BAG approach correlates with lower fluoroscopy time, radiation exposure, and perioperative pain management.[9,10] This study highlights key aspects of care that can be optimized to improve morbidity and mortality in radiologically guided PEG-tube.
Percutaneous endoscopic gastrostomy has been recognized as an effective method for providing enteral nutrition to patients with neuromotor impairment as well as head-and-neck cancer.[11] These conditions often lead to complications such as dysphagia, airway obstruction, weight loss, and aspiration pneumonia, making gastrostomy placement a necessary intervention.[11] Neuromotor impairment accounted for the majority of G-tube referrals (55.9% of the study population) at our institution. Within this subpopulation, 33.6% experienced at least one minor complication. Several factors may contribute to the higher incidence of complications in this patient population, including the inherent morbidity and frailty associated with neurodegenerative disease, preexisting malnutrition or poor nutritional status, and ongoing risk factors for aspiration.
As aforementioned, the results pertaining to fluoroscopy time, radiation exposure, and in-room time are quite noteworthy in this study. There was a trend toward lower radiation exposure dose (mGy PSD) in the BAG group compared to the dilator group. A potential explanation for the decreased radiographic parameters observed in the BAG group centers on the fact that the tube can be mounted onto the balloon wire, gradually dilating the gastrostomy tract, and expediently guided to the correct position within the stomach. This streamline approach facilitates a more efficient procedure, thus minimizing the risk of radiation-related complications. Conversely, the extended fluoroscopy time observed in the dilator group can be attributed to the utilization of peel-away sheaths and serial dilators, which contribute to a more elaborate preprocedural arrangement. Subsequently, the sheath is meticulously peeled back, revealing the tip of an inserted gastric tube. The intricate nature of this sequential process necessitates a greater number of procedural steps when compared to the BAG group, thus accounting for the protracted fluoroscopy duration.
Consistent with previous studies, there were no major complications in our study related to either gastrostomy devices. In a review of published studies on balloon gastrostomy catheters, the occurrence of minor complications exhibited a range from 27% to 68%.[6,12] Our study found minor complications occurring in similar frequencies between the balloon-mounted (BAG) and dilator groups. The observed trend toward increased minor complications in the BAG group is particularly intriguing, as it contrasts with the existing literature.[1] In theory, the utilization of a BAG technique presents a distinct advantage in terms of the smaller stoma diameter, which is tailored to accommodate the precise insertion of the gastric tube. The smaller diameter achieved through balloon-mounted gastrostomy can potentially contribute to a reduction in complications. Increased minor complications within the BAG group are likely attributable to a combination of factors such as underlying comorbidities, anatomical considerations, and technical challenges during the procedure. To better understand the factors contributing to minor complications, a larger-scale analysis encompassing a more diverse patient population and considering various clinical variables would be valuable.
In our study, it is important to note that the BAG group showed higher rates of pain and dislodgement. While the BAG approach has a simplified process, the use of a balloon-mounted G-tube may displace the stomach from the insertion point. This lack of stabilization can result in increased discomfort and pain. The process of balloon inflation creates additional pressure and stretching within the gastric tract, leading to heightened sensations of pain. Tube dislodgement caused by either accidental balloon deflation or breakage occurred in 17% of patients receiving BAG catheters. In rare instances, pneumoperitoneum can occur when air is not filled into the right inserted mark in the stomach because balloon dilatation moves the stomach from the insertion site. In contrast to the balloon-mounted approach, the utilization of dilators is associated with a lesser degree of gastric manipulation. However, it is noteworthy that the dilator approach potentially enlarges the gastrostomy tract beyond the optimal size. This practice, while intended to facilitate the G-tube placement, may inadvertently result in a larger opening and subsequently increase the risk of complications. Our study findings support this observation, as we identified a significantly higher infection rate in the dilator group compared to the balloon-mounted gastrostomy group (7.8% vs. 2.2%). Such an approach warrants careful consideration as it could potentially lead to increased complications and suboptimal outcomes.
The present study possesses some limitations, including its retrospective design and the potential for operator biases in G-tube placement. While the observed trends favored the BAG approach, it is important to acknowledge that the number of patients in the balloon group significantly exceeded that of the dilator group. Notably, the choice of catheters employed was determined by operator preference, with a preference for balloon-retained tubes observed particularly in cases involving facial trauma or failure to thrive subpopulation. The prevailing prevalence of BAG within our institution can be attributed to its ease of access, reduced radiation exposure, and observed expedited recovery times following the procedure. Furthermore, the investigators of this study expressed a preference for balloons due to their perceived lower risks of complications related to clogging and dislodgement. In future investigations, the implementation of randomized controlled trials would aid in mitigating biases associated with BAG utilization and offer additional validation of the study’s findings.
CONCLUSION
This study provides insight into the comparative efficacy of balloon and dilators for percutaneous gastrostomy tube placement. The findings suggest that the use of BAG is a safe and efficient approach with significantly lower radiation exposure, operating time, and perioperative pain management compared to dilator-based gastrostomies. This research highlights the benefits of utilizing balloon catheters over dilators in optimizing patient outcomes and also aids interventionalists in making informed decisions regarding the selection of percutaneous gastrostomy devices.
Declaration of patient consent
The Institutional Review Board (IRB) permission was obtained for the study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Radiologic, endoscopic, and surgical gastrostomy: An institutional evaluation and meta-analysis of the literature. Radiology. 1995;197:699-704.
- [CrossRef] [PubMed] [Google Scholar]
- Large or small bore, push or pull: A comparison of three classes of percutaneous fluoroscopic gastrostomy catheters. J Vasc Interv Radiol. 2008;19:557-63. quiz 564
- [CrossRef] [PubMed] [Google Scholar]
- Image guided percutaneous gastrostomy catheter placement: How we do it safely and efficiently. World J Gastroenterol. 2020;26:383-92.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of balloon and nonballoon gastrostomy tubes in children. J Pediatr Surg. 2020;55:852-4.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous gastrostomy and gastrojejunostomy: Additional experience in 519 procedures. Radiology. 1995;194:817-20.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous feeding gastrostomy with the Seldinger technique: Review of 252 patients. Radiology. 1989;171:359-62.
- [CrossRef] [PubMed] [Google Scholar]
- CIRSE standards of practice guidelines on gastrostomy. Cardiovasc Intervent Radiol. 2016;39:973-87.
- [CrossRef] [PubMed] [Google Scholar]
- Radiologically guided placement of pull-type gastrostomy tubes. Radiology. 1997;205:669-73.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous radiologic, surgical endoscopic, and percutaneous endoscopic gastrostomy/gastrojejunostomy: Comparative study and cost analysis. Cardiovasc Intervent Radiol. 1998;21:324-8.
- [CrossRef] [PubMed] [Google Scholar]
- Efficiency and safety of balloon-assisted gastrostomy. Cardiovasc Intervent Radiol. 2021;44:1423-9.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous endoscopic gastrostomy tube insertion in neurodegenerative disease: A retrospective study and literature review. Clin Endosc. 2017;50:270-8.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of balloon-and mushroom-retained large-bore gastrostomy catheters. AJR Am J Roentgenol. 2001;177:359-62.
- [CrossRef] [PubMed] [Google Scholar]






